Risks of sitting too long can lead to a multitude of health problems, impacting both physical and mental well-being. From musculoskeletal issues to cardiovascular risks, and even mental health concerns, understanding the dangers of prolonged sitting is crucial for maintaining a healthy lifestyle. This exploration delves into the various facets of this sedentary habit, highlighting the consequences and offering practical strategies for mitigation.
Prolonged sitting can have a detrimental effect on our bodies, weakening our muscles and potentially leading to pain and discomfort. This sedentary behavior is linked to numerous physical issues, including a higher risk of developing back pain, neck pain, and other musculoskeletal problems. Beyond physical symptoms, prolonged sitting has been correlated with increased risks for heart disease, stroke, and metabolic syndrome, demonstrating the far-reaching consequences of a sedentary lifestyle.
Physical Health Impacts
Prolonged sitting, a common feature of modern lifestyles, has profound and multifaceted effects on physical health. While seemingly innocuous, the sedentary nature of many jobs and leisure activities can contribute significantly to a range of health issues. This section delves into the physiological mechanisms behind these effects, focusing on the musculoskeletal system, cardiovascular health, metabolic health, and the link to weight gain.Prolonged periods of inactivity cause muscles to weaken, and joints to stiffen.
This reduced mobility, combined with the constant pressure on the spine and other joints, can lead to chronic pain and discomfort. Furthermore, the lack of movement can impair blood circulation, potentially affecting various bodily functions.
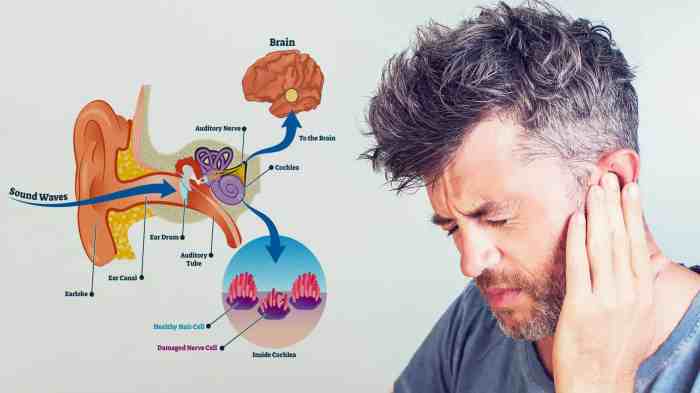
Musculoskeletal System Effects
Prolonged sitting puts considerable stress on the spine, particularly the lumbar region. The sustained flexion of the spine in a seated posture can exacerbate existing back problems or lead to new ones. Tightened hip flexors and hamstrings, often a result of sitting, can also contribute to lower back pain. The constant pressure on the discs and vertebrae can lead to degenerative changes over time, increasing the risk of herniated discs or spinal stenosis.
Neck pain is also a common complaint, as the head is held in a forward position for extended durations. This forward head posture places excessive strain on the neck muscles and ligaments, potentially leading to stiffness and pain.
Sitting still for extended periods isn’t great for your health, leading to various issues like stiffness and potential circulation problems. To combat these sedentary lifestyle downsides, fueling your body with the right foods is key. For example, incorporating foods rich in complex carbohydrates and protein, like those found in foods that give you energy , can help maintain energy levels throughout the day, which can indirectly help combat the sluggishness often associated with prolonged sitting.
Ultimately, a combination of movement and good nutrition is the best way to counteract the risks of prolonged sitting.
Risk Factors for Pain
Several factors contribute to the development of back and neck pain associated with prolonged sitting. These include: inadequate posture, poor ergonomics in the work environment, lack of regular movement, and pre-existing conditions like scoliosis. A sedentary lifestyle combined with these risk factors can significantly increase the chances of experiencing back pain and neck pain. Moreover, individuals who frequently engage in activities that require repetitive movements or forceful exertions while sitting can also be susceptible to these issues.
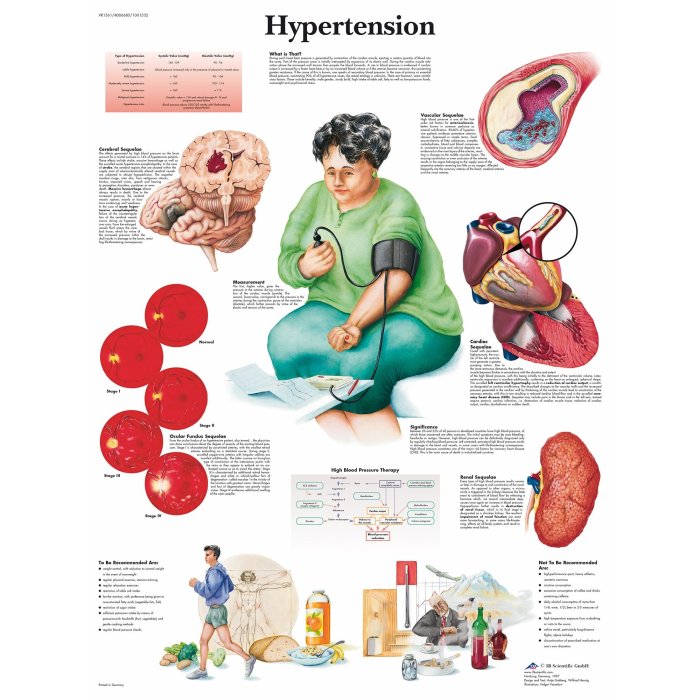
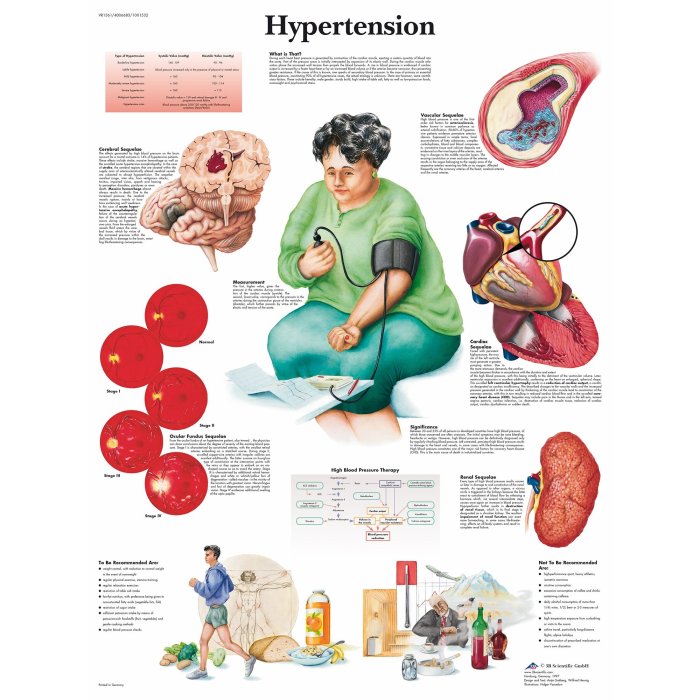
Cardiovascular Health Risks
The correlation between prolonged sitting and cardiovascular health risks is well-established. A sedentary lifestyle can contribute to increased blood pressure, elevated cholesterol levels, and an accumulation of visceral fat, all of which are major risk factors for heart disease and stroke. This is often due to reduced blood circulation and metabolic rate when sitting for extended periods. A lack of physical activity can also impair the body’s ability to regulate blood sugar, which is linked to heart disease and stroke.
Metabolic Syndrome
Prolonged sitting is linked to metabolic syndrome, a cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes. These conditions include high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels. The sedentary nature of prolonged sitting can directly contribute to these factors, further emphasizing the importance of regular physical activity.
Impact on Blood Sugar and Insulin Sensitivity
Studies have shown a strong correlation between prolonged sitting and impaired blood sugar control and insulin sensitivity. Inactivity reduces the body’s ability to effectively utilize insulin, leading to elevated blood sugar levels and potentially increasing the risk of type 2 diabetes. Individuals who spend significant time sitting may experience impaired glucose tolerance, meaning their bodies have difficulty regulating blood sugar.
Weight Gain and Obesity
Prolonged sitting is often a contributing factor to weight gain and obesity. A lower metabolic rate during periods of inactivity can result in the body storing more calories as fat. The reduced energy expenditure associated with sitting for long periods can lead to a calorie surplus, making it harder to maintain a healthy weight. This is further exacerbated by the tendency to overeat when sedentary.
Comparison of Sedentary Behaviors
| Sedentary Behavior | Risk Factors |
|---|---|
| Prolonged Sitting | Increased risk of back pain, neck pain, cardiovascular disease, metabolic syndrome, weight gain, impaired glucose tolerance. |
| Screen Time (e.g., Gaming, Social Media) | Increased risk of eye strain, carpal tunnel syndrome, poor posture, decreased physical activity, and potentially elevated stress levels. |
| Driving | Increased risk of back pain, muscle stiffness, poor posture, and decreased physical activity. |
| Standing for Extended Periods | Increased risk of varicose veins, leg cramps, and foot pain, along with potential musculoskeletal issues if not managed properly. |
Mental Health Consequences

Prolonged sitting, while seemingly innocuous, can have a profound impact on our mental well-being. The sedentary lifestyle often associated with prolonged sitting can lead to a cascade of negative psychological effects, impacting mood, cognitive function, and overall emotional regulation. Understanding these connections is crucial for promoting a healthier lifestyle.Prolonged periods of sitting can disrupt the delicate balance of our mental health, leading to a decreased sense of well-being.
This isn’t simply about feeling tired or sluggish; it can manifest in more significant psychological distress, affecting our ability to cope with daily stressors. The body’s physical response to prolonged inactivity plays a role in this process.
Psychological Effects on Mood and Well-being
Prolonged sitting can significantly influence mood and overall well-being. The lack of physical activity associated with a sedentary lifestyle can lead to feelings of lethargy, low energy, and irritability. This can negatively impact our perception of ourselves and our ability to enjoy daily activities.
Relationship Between Prolonged Sitting and Mental Health Conditions
A clear link exists between prolonged sitting and the development or exacerbation of mental health conditions such as anxiety, depression, and stress. Studies have shown a correlation between increased sedentary time and higher rates of these conditions. This correlation doesn’t necessarily prove causation, but it highlights the potential negative impact of prolonged sitting on mental health. Reduced physical activity can alter neurochemical processes in the brain, contributing to feelings of anxiety and depression.
Impact on Cognitive Function and Focus
Prolonged sitting can impair cognitive function and focus. Studies have indicated a connection between sedentary behavior and reduced cognitive performance, including difficulties with memory, attention span, and processing speed. The brain, like the body, benefits from movement. Physical activity enhances blood flow to the brain, which is crucial for optimal cognitive function. Reduced blood flow due to prolonged sitting can negatively impact mental clarity and focus.
Impact on Motivation and Engagement
Prolonged sitting can lead to a decrease in motivation and engagement in daily activities. A lack of physical activity can contribute to feelings of apathy and disinterest, impacting productivity and overall life satisfaction. This is often due to the link between physical activity and the release of endorphins, which have mood-boosting effects.
Impact on Sleep Quality
Prolonged sitting can negatively impact sleep quality. A sedentary lifestyle can disrupt the body’s natural sleep-wake cycle, leading to difficulty falling asleep, staying asleep, and experiencing restorative sleep. The lack of physical activity can contribute to feelings of restlessness and anxiety, making it harder to relax and prepare for sleep.
Impact on Emotional Regulation
Prolonged sitting can negatively impact emotional regulation. The lack of physical activity can lead to an increased susceptibility to negative emotions and difficulty managing stress. Physical activity, on the other hand, can help regulate emotions and improve mood.
Mental Health Risks of Prolonged Sitting
| Mental Health Risk | Description | Possible Interventions |
|---|---|---|
| Decreased Mood | Reduced feelings of happiness and well-being. | Increase physical activity, engage in enjoyable activities, seek support. |
| Anxiety | Excessive worry and fear. | Regular exercise, mindfulness practices, therapy. |
| Depression | Persistent sadness and loss of interest. | Regular exercise, social support, therapy. |
| Stress | Feelings of pressure and overwhelm. | Mindfulness techniques, relaxation exercises, stress management strategies. |
| Reduced Cognitive Function | Difficulty with memory, attention, and processing speed. | Incorporate regular physical activity, break up long sitting periods, engage in mentally stimulating activities. |
| Decreased Motivation | Loss of interest and drive. | Engage in enjoyable activities, set realistic goals, seek support. |
| Poor Sleep Quality | Difficulty falling asleep, staying asleep, or experiencing restorative sleep. | Establish a regular sleep schedule, create a relaxing bedtime routine, avoid caffeine and alcohol before bed, consider physical activity during the day. |
| Impaired Emotional Regulation | Difficulty managing emotions effectively. | Develop coping mechanisms for stress, engage in emotional regulation techniques, consider therapy. |
Practical Strategies for Mitigation
Sitting for extended periods takes a toll on our bodies, impacting both physical and mental well-being. Fortunately, proactive strategies can significantly reduce these negative consequences. By incorporating regular movement and mindful breaks into our daily routines, we can mitigate the risks associated with prolonged sitting. This involves understanding the importance of various approaches and tailoring them to our individual needs and work environments.Adopting these practical strategies is crucial for maintaining a healthy lifestyle, particularly in today’s predominantly sedentary work culture.
Integrating these techniques allows us to regain control over our physical health, enhancing our overall well-being and productivity.
Organizing Strategies for Reducing Sitting Time, Risks of sitting too long
Effective strategies for reducing sitting time throughout the day involve a multifaceted approach. This requires mindful planning and proactive implementation of techniques that seamlessly integrate movement into daily routines. Consistency and adaptability are key to achieving long-term success.
- Scheduling Regular Movement Breaks: Integrating scheduled movement breaks into your daily routine is crucial. This could involve setting alarms for short, 5-10 minute walks or stretches every hour. Pre-planning these breaks ensures they aren’t overlooked amidst busy schedules. For example, a 10-minute walk after lunch or a 5-minute stretching session during a lull in the workday can significantly improve physical health.
- Incorporating Movement into Work Tasks: Consider tasks that require movement. Instead of sending emails while seated, walk to a colleague’s desk or use the opportunity to make a quick walk around the office. Making small changes in work tasks can help incorporate movement seamlessly. For example, if your job involves a lot of phone calls, take them while walking around your office.
Sitting all day can lead to a whole host of issues, from back pain to poor circulation. One often overlooked consequence is puffy eyes, which can really drag down your appearance. Luckily, there are some simple home remedies to combat this, like using cold compresses or getting enough sleep. For a deeper dive into how to get rid of puffy eyes, check out this helpful guide: how to get rid of puffy eyes.
But seriously, moving around more is key to preventing those unsightly bags and overall better health! Regular movement and breaks throughout the day are essential to counteract the risks of prolonged sitting.
If your work allows for it, perform tasks that require standing or moving, such as fetching materials or handling deliveries, instead of just sitting down.
Importance of Incorporating Regular Movement
Regular movement is not just about avoiding prolonged sitting; it’s about fostering a healthier, more active lifestyle. Incorporating movement into daily routines is fundamental for maintaining physical and mental well-being.
- Promoting Circulation and Blood Flow: Movement enhances circulation, promoting healthy blood flow throughout the body. This prevents blood clots and reduces the risk of cardiovascular issues associated with prolonged inactivity. Improved circulation also benefits muscle function and reduces stiffness.
- Strengthening Muscles and Bones: Regular movement strengthens muscles and bones, reducing the risk of osteoporosis and other age-related conditions. Consistent activity also helps maintain muscle mass, which is essential for maintaining a healthy weight.
Taking Short Breaks and Standing Up Frequently
Regular short breaks and frequent standing are vital components of a healthy work environment. These practices help alleviate the negative impacts of prolonged sitting.
- Frequency and Duration of Breaks: Aim for standing or moving around every 30 minutes to an hour. Even short, 5-10 minute breaks can significantly improve circulation and reduce stiffness. Taking these breaks regularly reduces the negative effects of prolonged sitting.
- Types of Movement During Breaks: Vary the types of movement during breaks to keep things engaging. This could involve walking, stretching, or simple exercises. This helps to maintain interest and consistency in your break routines. A quick walk around the block or a few minutes of yoga or tai chi can be very beneficial. The key is to choose activities you enjoy.
Ergonomic Workspaces and Furniture
Ergonomic workspaces and furniture are crucial for minimizing the risks associated with prolonged sitting. Appropriate design reduces strain on the body and promotes better posture.
- Adjusting Chair Height and Support: Ensure your chair height and backrest support your lower back, promoting good posture. This prevents slouching and reduces strain on the spine. An adjustable chair with proper lumbar support is key to good posture.
- Selecting Appropriate Desk Height: A desk height that allows for a natural posture is essential. A height that allows your arms to rest comfortably at your sides and your elbows to be at a 90-degree angle promotes good posture.
Effective Ways to Break Up Sitting Time
Breaking up sitting time is vital for overall well-being. These techniques integrate movement into various work tasks.
- Standing Meetings and Phone Calls: Consider standing meetings and phone calls. This allows for movement while engaging in work tasks. Holding meetings while walking around can increase productivity and reduce the negative impact of sitting for long periods.
- Using a Standing Desk: A standing desk offers an alternative to a traditional seated workstation. This allows for flexibility in posture and movement throughout the workday. It’s an effective strategy for those who spend long hours at a desk.
Comparing and Contrasting Approaches to Promoting Physical Activity
Various approaches to promoting physical activity throughout the workday offer different advantages. Understanding these differences allows for a tailored approach to suit individual needs.
| Approach | Advantages | Disadvantages |
|---|---|---|
| Scheduled Breaks | Structured, predictable, easier to integrate | May not be suitable for all work environments |
| Movement-integrated Tasks | Naturally incorporates movement into workflow | Requires adjustments to existing work processes |
Designing a Schedule that Incorporates Movement Breaks
Creating a schedule that incorporates movement breaks involves careful planning and consideration of individual work routines. This schedule should be tailored to the specific demands of the job and personal preferences.
- Consider Workflows and Tasks: Analyze the workday’s structure to identify opportunities for incorporating movement. Look for tasks that can be performed while standing or moving.
- Personal Preferences and Needs: Prioritize activities that are enjoyable and align with personal preferences. Choose activities that are sustainable and adaptable to the specific work environment. This ensures adherence to the schedule and prevents burnout.
Workplace Interventions: Risks Of Sitting Too Long
Creating a supportive work environment that encourages movement is crucial for employee well-being and productivity. Prolonged sitting is a significant health risk, and companies have a responsibility to mitigate this by promoting active work styles. By implementing proactive strategies, organizations can foster healthier, happier, and more productive workforces.Addressing the issue of prolonged sitting requires a multifaceted approach, encompassing both individual and organizational interventions.
Encouraging movement throughout the workday, through designated breaks and supportive workstation options, demonstrably reduces the risks associated with sedentary behavior. This proactive approach not only benefits employees’ physical health but also positively impacts their mental well-being, leading to increased job satisfaction and decreased absenteeism.
Best Practices for a Movement-Encouraging Work Environment
Implementing effective workplace interventions requires a comprehensive strategy that fosters a culture of movement. This encompasses a variety of initiatives, from promoting standing desks to incorporating movement breaks into company policies. A supportive environment that recognizes the importance of physical activity significantly improves employee health and well-being.
- Promoting Standing Desks and Adjustable Workstations: Providing employees with access to adjustable height desks and standing desks is a crucial first step. This allows employees to alternate between sitting and standing throughout the day, promoting natural movement and reducing prolonged periods of sitting. Many companies are now recognizing the value of offering a variety of workstation options to meet individual needs.
This is a direct way to address the issue of prolonged sitting, and can have a positive effect on both physical and mental health.
- Incorporating Movement Breaks into Company Policies: Formalizing movement breaks in company policies sends a strong message that employee well-being is a priority. Scheduling regular, short movement breaks, such as walking meetings or quick stretches, can significantly reduce the risks associated with prolonged sitting. These breaks can be as short as 5-10 minutes, but their frequency is crucial for encouraging movement and avoiding health issues.
Examples of Successful Workplace Initiatives
Numerous companies have successfully implemented initiatives to combat prolonged sitting, with positive results. These initiatives showcase the potential for a supportive work environment to positively impact employee health and productivity. A key element is the active involvement of management.
- Company X: Implemented a program where employees rotate between standing desks and seated desks throughout the day, with a dedicated break time for stretching and light exercise. This initiative significantly reduced musculoskeletal issues and improved employee morale.
- Company Y: Introduced a “walking meeting” policy, encouraging teams to hold meetings while walking around the office or nearby parks. This simple change improved communication and promoted physical activity, improving employee satisfaction and reducing stress.
Role of Management in Encouraging Employee Well-being
Management plays a critical role in fostering a supportive work environment. Leaders who actively promote employee well-being demonstrate a commitment to their workforce’s overall health and productivity. This includes prioritizing employee health through actionable initiatives.
- Leading by Example: Managers who actively participate in promoting movement, such as taking the stairs or incorporating movement breaks into their own schedule, set a positive example for employees.
- Providing Resources and Support: Managers can provide access to resources, such as ergonomic assessments and guidance on proper posture, to ensure employees have the support they need to adopt healthy work habits.
Benefits of Activity-Based Workspaces
Activity-based workspaces provide a dynamic environment that encourages movement and flexibility. By incorporating various work zones, such as standing areas and collaborative spaces, these workspaces promote movement and interaction among employees.
- Flexibility and Choice: Employees have the choice to work in different zones based on their tasks and preferences. This flexibility encourages movement throughout the workday.
- Improved Collaboration: Activity-based workspaces promote interaction among employees, which can lead to improved collaboration and creativity.
Policies for Incorporating Movement Breaks
| Work Environment | Policy for Movement Breaks |
|---|---|
| Office Setting | Schedule 5-10 minute movement breaks every hour, encourage walking meetings. |
| Retail Environment | Encourage employees to move around the store, provide opportunities for short stretching breaks. |
| Manufacturing Setting | Designate specific break times for stretching and light exercise, incorporate movement into tasks wherever possible. |
Preventive Measures for Individuals
Sitting for extended periods is a significant health concern, impacting both physical and mental well-being. This necessitates proactive measures to combat the negative consequences of prolonged inactivity. Individuals can take practical steps to mitigate these risks and enhance their overall health and quality of life. These measures include incorporating movement into daily routines, choosing active hobbies, and maintaining a consistent exercise regimen.
Sitting all day can wreak havoc on your body, leading to various health issues. Beyond the obvious aches and pains, prolonged sitting can also impact your overall well-being. For example, some medications, like Xanax, might have unexpected side effects, such as potential erectile dysfunction. Check out this article to learn more about the link between Xanax and this specific concern: can xanax cause erectile dysfunction.
Ultimately, maintaining a healthy balance between sitting and movement is crucial for a well-functioning body.
Incorporating Movement into Daily Activities
Integrating movement into daily activities is crucial for combating the detrimental effects of prolonged sitting. This involves conscious efforts to incorporate physical activity throughout the day, rather than solely relying on dedicated exercise sessions. Walking, cycling, and stair climbing are readily accessible options that significantly contribute to an active lifestyle.
- Walking: Regular walking, even short bursts throughout the day, can significantly improve cardiovascular health and reduce the risk of various diseases. Taking the stairs instead of the elevator, or parking farther away from your destination are simple examples of incorporating walking into daily routines.
- Cycling: Cycling is an excellent cardiovascular exercise that can be incorporated into commutes and recreational activities. Choosing to cycle to work or for errands offers a healthy and efficient way to combine travel and exercise.
- Stair Climbing: Climbing stairs instead of using elevators is a simple yet effective way to increase physical activity. Taking the stairs at work, school, or home can add up to significant activity throughout the day.
Incorporating Activity into Commute Routines
The commute often represents a significant period of sedentary behavior. However, individuals can transform this time into an opportunity for movement.
- Walking or Cycling to Work: Instead of driving, consider walking or cycling to work, weather permitting. This offers a convenient way to combine travel with exercise, promoting physical health and reducing environmental impact.
- Utilizing Public Transportation: Public transportation often involves walking or cycling to and from stations. This naturally incorporates movement into the commute, minimizing sedentary time.
- Active Transportation Options: Explore options like walking or cycling to meetings, errands, or appointments, whenever feasible.
Choosing Active Hobbies and Recreational Activities
Active hobbies and recreational pursuits are essential for maintaining an active lifestyle and reducing the negative impact of prolonged sitting.
- Outdoor Activities: Engage in activities like hiking, gardening, or playing sports outdoors. These activities naturally incorporate movement and fresh air, fostering overall well-being.
- Dancing: Dancing is a fun and engaging way to increase physical activity and improve coordination. It’s a great way to socialize and stay active.
- Team Sports: Team sports like basketball, soccer, or volleyball offer a social environment that encourages regular physical activity.
Incorporating Stretching and Other Physical Exercises
Regular stretching and other physical exercises are vital for maintaining flexibility, muscle strength, and overall physical health.
- Stretching routines: Incorporate regular stretching routines into your daily schedule to maintain flexibility and prevent stiffness. Simple stretches, held for a few seconds, can make a noticeable difference.
- Yoga and Pilates: Yoga and Pilates offer a structured approach to exercise, combining physical postures, breathing techniques, and mindfulness. They help improve flexibility, strength, and balance.
- Strength Training: Strength training exercises help build muscle mass, which in turn boosts metabolism and improves overall physical health. This can be done at home or at the gym.
Comparing and Contrasting Methods for Increasing Physical Activity
Different methods of increasing physical activity have varying benefits and drawbacks. Understanding these differences helps individuals choose the most suitable methods for their lifestyle and preferences.
- Structured Exercise: Structured exercise, such as gym workouts or fitness classes, offers a focused and supervised approach to physical activity. However, it requires dedicated time and resources.
- Incorporating Movement into Daily Activities: This approach involves integrating movement into everyday tasks, which is often more sustainable and convenient for many individuals. It requires less dedicated time but more conscious effort.
- Active Hobbies: Active hobbies and recreational pursuits offer a fun and engaging way to incorporate physical activity into leisure time. They encourage long-term adherence and provide opportunities for social interaction.
Recommendations for Incorporating Movement into Daily Life
This table offers recommendations for incorporating movement into different aspects of daily life.
| Aspect of Daily Life | Recommendation |
|---|---|
| Commute | Walk, cycle, or utilize public transportation whenever possible. |
| Work | Take the stairs, stand up frequently, and engage in short movement breaks. |
| Errands | Walk or cycle instead of driving for short errands. |
| Leisure Time | Engage in active hobbies like hiking, dancing, or playing sports. |
| Household Chores | Incorporate physical activity into tasks like gardening or cleaning. |
Illustrative Examples
Prolonged sitting, a ubiquitous aspect of modern life, poses significant health risks. Understanding how these risks manifest in various scenarios is crucial for preventative measures. This section provides concrete examples of the detrimental effects of prolonged sitting, illustrating the impact on different professions and individuals.
Scenarios Illustrating Prolonged Sitting Risks
Prolonged sitting, often overlooked, can lead to a cascade of negative health outcomes. These outcomes can be exacerbated by factors like poor posture, inadequate ergonomic support, and lack of breaks. Consider these examples:
- A software developer, accustomed to hours of uninterrupted coding, might experience back pain, stiffness, and potential circulatory issues due to a lack of movement throughout the workday. This lack of movement can contribute to muscle fatigue and stiffness.
- A cashier, confined to a stationary position for extended periods, could develop varicose veins, a common complication of prolonged sitting. This is particularly true if the cashier lacks adequate leg elevation opportunities or doesn’t incorporate regular stretching into their routine.
- A factory worker on an assembly line, subjected to repetitive motions and long periods of sitting, may develop carpal tunnel syndrome or other musculoskeletal disorders. The repetitive nature of the work, combined with prolonged sitting, can lead to chronic pain and reduced productivity.
Impact on Specific Professions
Certain professions inherently involve prolonged sitting. Understanding these impacts is crucial for implementing appropriate preventative measures.
- Data Entry Clerks: These professionals are often confined to a desk for extended hours, processing data. This prolonged sitting can contribute to lower back pain, stiff necks, and poor posture. Implementing regular breaks and promoting standing workstations can help mitigate these risks.
- Call Center Agents: Call center agents are often in a stationary position, making them susceptible to the same health issues as data entry clerks. The stress of customer interactions can also exacerbate the negative effects of prolonged sitting.
- Truck Drivers: While driving is a physically demanding activity, prolonged sitting in the cab can contribute to a variety of health issues. The lack of movement and repetitive driving motions can lead to muscle stiffness, circulation problems, and back pain.
Real-World Case Studies
Real-world examples demonstrate the correlation between prolonged sitting and health outcomes. While specific case studies may not be publicly available, the general trends are supported by scientific research.
Correlation Between Prolonged Sitting and Health Conditions
The link between prolonged sitting and various health conditions is well-documented.
- Cardiovascular Disease: Studies consistently demonstrate a strong correlation between prolonged sitting and an increased risk of cardiovascular disease. The lack of movement during prolonged sitting can negatively impact blood circulation and increase blood pressure.
- Obesity: A sedentary lifestyle, often characterized by prolonged sitting, is a significant contributor to obesity. The reduced energy expenditure associated with prolonged sitting contributes to weight gain.
- Type 2 Diabetes: Research suggests that prolonged sitting is a risk factor for developing type 2 diabetes. The impact on insulin sensitivity and glucose metabolism can lead to an increased likelihood of developing this condition.
Potential Sitting Time Risks by Job Type
This table illustrates potential sitting time risks across various job types. Note that these are general estimates, and individual factors can influence actual sitting times.
| Job Type | Potential Sitting Time Risk |
|---|---|
| Office Worker (General) | High |
| Data Entry Clerk | Very High |
| Call Center Agent | High |
| Truck Driver | High |
| Retail Cashier | Medium to High |
| Construction Worker (Manual Labor) | Low to Medium |
Closing Summary

In conclusion, the risks associated with prolonged sitting are substantial and multifaceted, affecting both physical and mental health. While seemingly harmless, the detrimental effects of prolonged sitting underscore the importance of incorporating regular movement and activity into our daily routines. By implementing practical strategies for reducing sitting time, creating supportive work environments, and adopting preventive measures, we can significantly mitigate these risks and cultivate healthier lifestyles.





 (Note: This is a placeholder, an image of valine’s structure would be ideal here.)
(Note: This is a placeholder, an image of valine’s structure would be ideal here.) (Note: This is a placeholder, an image of leucine’s structure would be ideal here.)
(Note: This is a placeholder, an image of leucine’s structure would be ideal here.) (Note: This is a placeholder, an image of isoleucine’s structure would be ideal here.)
(Note: This is a placeholder, an image of isoleucine’s structure would be ideal here.)