Menopause facts and statistics paint a compelling picture of this significant life transition. From global prevalence rates and demographic breakdowns to the intricate interplay of symptoms, health impacts, and management strategies, this exploration provides a comprehensive overview. Understanding the realities of menopause empowers women and healthcare professionals alike.
This deep dive examines the prevalence of menopause across diverse populations, considering factors like geographical location, socioeconomic status, and ethnicity. We’ll explore the average age of onset and its variability, alongside projected future trends. This includes a look at common symptoms and their potential long-term effects on various aspects of health, from cardiovascular well-being to cognitive function.
Prevalence and Demographics
Menopause, a natural biological process marking the end of a woman’s reproductive years, is a significant life event impacting a substantial portion of the global population. Understanding its prevalence across different demographics is crucial for tailoring healthcare strategies and addressing the diverse needs of affected women. This section delves into the global distribution, average age of onset, and future projections for menopause prevalence.
Global Distribution and Socioeconomic Factors
Menopause affects all women, but the experience varies significantly based on geographical location and socioeconomic status. Factors like access to healthcare, nutrition, and overall lifestyle influence the timing and experience of menopause.
| Region | Percentage of Women Experiencing Menopause | Average Age of Onset | Notes |
|---|---|---|---|
| North America | ~50% | 51 years | Generally higher socioeconomic status, varied access to healthcare. |
| Western Europe | ~52% | 51-52 years | High healthcare access, but variations exist based on specific countries. |
| Sub-Saharan Africa | ~48% | 49-50 years | Significant variations in access to healthcare and nutrition, potentially influenced by environmental factors. |
| South Asia | ~45% | 48-49 years | Variations in nutrition and lifestyle choices. |
| East Asia | ~51% | 50 years | Varying levels of access to healthcare, influenced by socioeconomic factors and cultural practices. |
The table above provides a simplified overview. Actual figures can vary significantly within each region based on factors such as ethnicity, specific geographic location, and individual lifestyle. Further research is needed to pinpoint these variations more accurately.
Average Age of Menopause Onset
The average age of menopause onset globally is approximately 51 years. However, variations are significant and can be influenced by a multitude of factors. Genetic predisposition, ethnicity, and lifestyle choices all play a role in determining when menopause occurs.
- Genetics: Family history of early or late menopause can significantly impact an individual’s experience. This is a complex genetic interaction.
- Ethnicity: Studies suggest variations in the average age of menopause onset across different ethnic groups, potentially influenced by genetic and environmental factors.
- Lifestyle Choices: Factors like diet, exercise, and overall health contribute to the timing of menopause. A healthy lifestyle may lead to a slightly later onset.
These factors often interact in complex ways, making precise predictions challenging.
Future Trends in Menopause Prevalence, Menopause facts and statistics
As global populations age, the prevalence of menopause is expected to increase. This trend is particularly evident in developed countries with aging demographics.
“The aging of global populations will lead to a larger proportion of women experiencing menopause, potentially placing greater strain on healthcare systems.”
This increase in the number of women experiencing menopause could lead to an increased demand for healthcare services focused on managing the symptoms and promoting overall well-being during this life stage. For example, increased awareness and prevention strategies could be crucial in mitigating the potential impact of menopause-related conditions.
Symptoms and Experiences

Navigating menopause can be a unique journey for each woman, marked by a complex interplay of physical and emotional changes. Understanding the common symptoms, their potential impact, and how they vary across different populations is crucial for both personal well-being and healthcare decision-making. This section dives deep into the experiences associated with menopause, focusing on the common symptoms and their potential long-term consequences.
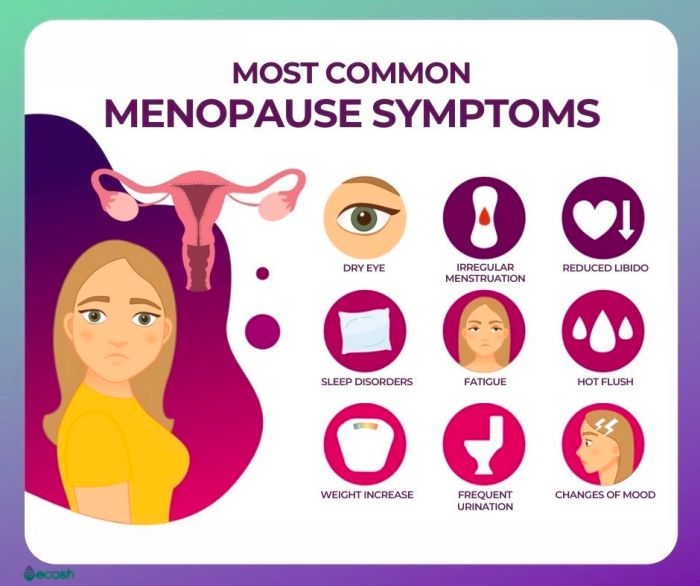
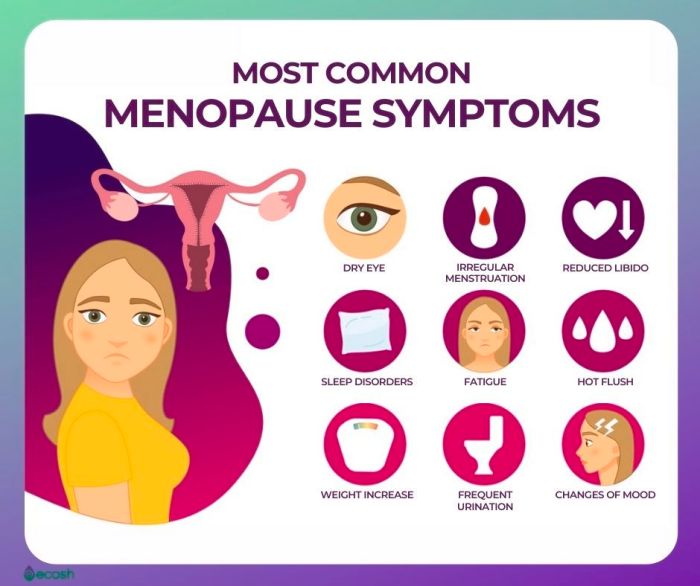
Common Symptoms of Menopause
Menopause is characterized by a range of physical and emotional symptoms, varying greatly in intensity and duration. Hot flashes, sleep disturbances, and mood swings are frequently reported. These symptoms often emerge gradually, impacting daily life and well-being.
Did you know that menopause affects millions worldwide? Understanding the facts and statistics surrounding this life stage is crucial. However, some recent research suggests a potential link between weight-loss medications like Wegovy and hair loss. Investigating the wegovy hair loss risk is important for those considering these medications. Ultimately, more research into the full spectrum of menopause-related factors is always welcome.
Hot Flashes
Hot flashes, a sudden sensation of warmth, often accompanied by sweating, are a hallmark symptom of menopause. Their frequency and severity differ considerably between individuals. These episodes can occur at any time of day or night, interrupting sleep and daily activities. Some women experience mild, fleeting sensations, while others have more intense and prolonged episodes that significantly impact their quality of life.
Sleep Disturbances
Sleep disturbances are a frequent companion during menopause. These problems can manifest as difficulty falling asleep, frequent awakenings during the night, or early morning awakenings. The underlying mechanisms contributing to sleep disturbances are multifaceted, potentially including hormonal fluctuations, night sweats, and anxiety. These sleep difficulties can have a cascading effect, impacting daytime alertness, mood, and overall well-being.
Mood Changes
Mood swings are another frequently reported symptom. Fluctuations in hormone levels can contribute to irritability, anxiety, and feelings of sadness or depression. These emotional changes can vary in intensity and duration, sometimes affecting interpersonal relationships and daily functioning.
Variability Across Populations
The frequency and severity of menopausal symptoms are influenced by various factors, including genetics, lifestyle, and underlying health conditions. For example, women from certain ethnic backgrounds or with pre-existing conditions like cardiovascular disease might experience symptoms differently. Socioeconomic factors, access to healthcare, and cultural norms also play a role in how symptoms are perceived and managed.
Long-Term Health Implications of Untreated Symptoms
Untreated menopausal symptoms can contribute to a range of long-term health issues. For example, persistent hot flashes can lead to cardiovascular problems, and sleep disturbances can exacerbate existing mental health concerns. Furthermore, untreated mood changes can increase the risk of developing chronic conditions.
Symptom Summary Table
| Symptom | Frequency | Severity | Potential Long-Term Health Implications |
|---|---|---|---|
| Hot Flashes | Variable; can range from infrequent to frequent, often episodic. | Variable; some women experience mild, short-lived episodes, while others experience severe, prolonged episodes. |
|
| Sleep Disturbances | Common; many women report difficulty falling asleep, frequent awakenings, or early morning awakenings. | Variable; can range from mild to severe, significantly affecting daily life. |
|
| Mood Changes | Common; many women experience irritability, anxiety, or feelings of sadness. | Variable; can range from mild fluctuations to severe mood swings. |
|
Health Impacts of Menopause
Menopause marks a significant transition in a woman’s life, bringing about hormonal shifts that impact various aspects of her health. Understanding these impacts is crucial for proactive health management during and after this stage. This section delves into the effects of menopause on cardiovascular health, bone density, cognitive function, and the increased risk of certain diseases. It also explores the controversial topic of hormone replacement therapy (HRT).
Cardiovascular Health
The decline in estrogen levels during menopause is linked to an increased risk of cardiovascular disease. Estrogen plays a vital role in maintaining healthy blood vessels and regulating cholesterol levels. Without adequate estrogen, women may experience a higher risk of developing atherosclerosis, a condition where plaque builds up in the arteries, potentially leading to heart attacks and strokes.
This risk is often exacerbated by other factors like obesity, lack of physical activity, and smoking. Observational studies show a correlation between declining estrogen levels and an increase in heart disease incidence in postmenopausal women.
Did you know that menopause affects millions of women globally? Understanding the facts and statistics surrounding this life stage is crucial. While that’s important, it’s also fascinating to delve into less common topics, like whether Gleason 6 prostate cancer is truly cancer. This question often pops up in conversations about men’s health, and I’ve found some interesting insights on this topic at is gleason 6 prostate cancer really cancer.
Regardless, menopause facts and statistics are still incredibly important for women’s health. It’s all about learning more and supporting each other.
Bone Density
Menopause significantly increases the risk of osteoporosis, a condition characterized by reduced bone density. Estrogen is essential for maintaining bone strength and preventing bone loss. As estrogen levels decrease, bone turnover accelerates, resulting in weakened bones, making them more susceptible to fractures. Post-menopausal women are at a higher risk of fractures, especially in the hip, spine, and wrist.
Factors like calcium deficiency, lack of vitamin D, and lifestyle choices contribute to this increased risk. Bone density scans are crucial for early detection and intervention.
Cognitive Function
Research suggests a potential link between menopause and cognitive function, though the exact nature of this relationship is still being explored. While some studies indicate a possible association between declining estrogen levels and cognitive decline, the effects appear complex and influenced by various factors. These factors may include age, lifestyle, and overall health. While more research is needed, maintaining a healthy lifestyle, including a balanced diet, regular exercise, and mental stimulation, can be beneficial for cognitive health throughout the menopausal transition.
Risk of Certain Diseases
Menopause is associated with an increased risk of certain chronic diseases. The loss of estrogen protection contributes to a higher likelihood of developing conditions like osteoporosis and cardiovascular disease. Other possible links to menopausal changes are under investigation, highlighting the need for further research.
Hormone Replacement Therapy (HRT)
Hormone replacement therapy (HRT) is a treatment option for managing menopausal symptoms, but it’s crucial to weigh the potential risks and benefits carefully. HRT aims to replenish estrogen and potentially other hormones, alleviating symptoms like hot flashes, night sweats, and vaginal dryness. However, HRT has been linked to an increased risk of certain health problems, including blood clots, stroke, and breast cancer.
The decision to use HRT should be made in consultation with a healthcare professional, carefully considering individual health history and risk factors. A personalized risk assessment is essential.
Comparison of Risk Factors
| Factor | Pre-menopausal | Peri-menopausal | Post-menopausal |
|---|---|---|---|
| Cardiovascular Disease | Lower risk, influenced by lifestyle factors | Risk increases due to hormonal changes | Increased risk, hormonal changes and lifestyle factors |
| Osteoporosis | Low risk, influenced by lifestyle factors | Risk increases due to hormonal changes | Increased risk, hormonal changes and lifestyle factors |
| Cognitive Decline | Lower risk, influenced by lifestyle factors | Potential for increased risk, complex interplay of factors | Potential for increased risk, complex interplay of factors |
Note: This table is a simplified representation of complex factors and does not include all possible risk factors. Individual risk factors may vary.
Management and Treatment Options
Navigating menopause can be challenging, but effective strategies exist to manage symptoms and improve quality of life. This section explores various approaches, from lifestyle adjustments to medical interventions, to help you understand the options available. We’ll delve into the efficacy and potential side effects of each approach, highlighting the crucial role of a balanced lifestyle in managing menopausal symptoms.Understanding the diverse range of treatment options is key to making informed decisions.
This involves considering personal preferences, symptom severity, and overall health. We’ll also emphasize the importance of open communication with healthcare providers to tailor a personalized management plan.
Lifestyle Modifications
Lifestyle modifications are often the first line of defense against menopausal symptoms. They are generally non-invasive and can significantly reduce discomfort. Adopting healthy habits can have a positive impact on overall well-being, contributing to a more comfortable transition through menopause.
- Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help manage symptoms. Foods rich in calcium and vitamin D are crucial for maintaining bone health. Reducing processed foods, sugary drinks, and excessive caffeine can also contribute to symptom relief.
- Exercise: Regular physical activity, including cardiovascular exercise and strength training, can help alleviate symptoms like hot flashes, mood swings, and sleep disturbances. Exercise also contributes to overall fitness and well-being.
- Stress Management: Chronic stress can exacerbate menopausal symptoms. Techniques like yoga, meditation, deep breathing exercises, and spending time in nature can help manage stress and promote relaxation.
Alternative Therapies
Several alternative therapies are explored for managing menopausal symptoms, though their efficacy is often debated. Research on their effectiveness varies, and individual experiences may differ.
- Herbal Remedies: Some herbal remedies, like black cohosh, are commonly used to manage hot flashes. However, it’s crucial to consult with a healthcare professional before using herbal remedies, as they can interact with medications and may not be suitable for everyone.
- Acupuncture: Some studies suggest that acupuncture can help reduce hot flashes and improve sleep quality. It’s a non-invasive treatment that can be considered as a complementary therapy.
Medical Interventions
Hormone therapy (HT) remains a common medical intervention for managing menopausal symptoms. It’s crucial to understand the different types of HT, their effectiveness, and potential risks.
- Hormone Therapy (HT): HT, also known as hormone replacement therapy (HRT), involves replacing hormones lost during menopause. It can effectively alleviate hot flashes, night sweats, and vaginal dryness. However, HT carries potential risks, including an increased risk of blood clots, stroke, and certain cancers. The decision to use HT should be made in consultation with a healthcare professional, considering individual risk factors and symptom severity.
- Other Medications: Certain medications, such as selective serotonin reuptake inhibitors (SSRIs), may be prescribed to manage mood swings and sleep disturbances associated with menopause. These medications can also be used to treat other conditions, and the appropriateness of their use in menopause management needs to be discussed with a healthcare provider.
Comparison of Treatment Options
| Treatment Option | Effectiveness | Potential Side Effects | Suitability |
|---|---|---|---|
| Lifestyle Modifications | Generally effective for symptom management | Minimal side effects | Suitable for most individuals |
| Alternative Therapies (e.g., Herbal Remedies, Acupuncture) | Varied effectiveness; some evidence of benefit | Potential interactions with medications; individual responses may differ | May be suitable as complementary therapies, but requires consultation |
| Hormone Therapy (HT) | Highly effective for managing many symptoms | Potential risks, including blood clots, stroke, and certain cancers | Suitable for individuals with severe symptoms and low risk factors |
| Other Medications (e.g., SSRIs) | May be effective for specific symptoms | Potential side effects, such as nausea, headaches, and sleep disturbances | Suitable for individuals with specific symptom profiles, in consultation with a physician |
Social and Cultural Perspectives: Menopause Facts And Statistics
Menopause, a natural biological process, is often shrouded in social and cultural perceptions that vary significantly across different societies and throughout history. These perceptions can profoundly affect a woman’s experience during this transition and her access to appropriate healthcare. Understanding these nuances is crucial for fostering a more supportive and informed approach to menopause.Different cultures have historically viewed menopause through varying lenses, from stigmatization and fear to reverence and acceptance.
Did you know that around 80% of women experience some form of menopausal symptom? It’s a fascinating period of life with a lot of interesting facts and statistics, but finding healthy ways to manage those symptoms is key. One thing I’ve been exploring is the potential benefits of different teas, like black tea vs green tea, on overall well-being.
This article dives deep into the differences between these two popular beverages, and I’m hoping to learn more about which might be best for managing those pesky menopausal symptoms. Understanding these statistics and finding helpful coping strategies is really important for women going through this phase.
These perspectives have a direct impact on how women navigate the physical and emotional changes associated with menopause and their overall well-being.
Varying Cultural Perceptions
Cultural beliefs about menopause can range from viewing it as a debilitating condition to a rite of passage or even a time of increased wisdom. These differing perceptions stem from a combination of historical practices, religious beliefs, and societal norms. Understanding these varying viewpoints is essential for creating a more inclusive and supportive environment for women experiencing menopause.
Historical Evolution of Understanding
The understanding of menopause has evolved significantly throughout history. In ancient times, menopause was often viewed with fear and mystery. As medical knowledge advanced, so did our comprehension of the physiological changes associated with menopause. Early medical texts often reflected the societal views of the time, with some cultures attributing symptoms to supernatural causes. However, with advancements in medical research, we now have a much clearer picture of the hormonal changes and their impact on women’s health.
Impact on Healthcare Access
The social and cultural context surrounding menopause can significantly impact women’s access to healthcare. In some societies, women may hesitate to seek medical attention for menopausal symptoms due to cultural stigma or a lack of awareness about available treatments. Conversely, in other cultures, there may be a greater emphasis on seeking support from family members or traditional healers, which can either complement or hinder formal medical care.
Cultural Differences in Management
Different cultures have developed diverse approaches to managing menopausal symptoms. Some cultures emphasize traditional remedies and herbal treatments, while others rely heavily on modern medical interventions. The availability and accessibility of healthcare services also play a crucial role in shaping these approaches.
“Cultural perceptions of menopause range from stigmatization and fear to acceptance and reverence, significantly influencing women’s experiences and healthcare access.”
Research and Future Directions
Unraveling the complexities of menopause requires ongoing research to improve understanding and management. Current studies are shedding light on the multifaceted nature of this transition, from hormonal fluctuations to their impact on various aspects of women’s health. This exploration of ongoing research and future directions will highlight the significance of these studies in enhancing the lives of women experiencing menopause.
Current Research Areas
Research into menopause and its associated health issues is broad and multifaceted. Studies are investigating the intricate interplay between hormonal changes, lifestyle factors, and the development of various health conditions. Understanding the long-term health consequences of menopausal transitions is crucial for preventative measures and personalized care. Researchers are actively exploring the genetic and environmental factors that influence the onset, duration, and severity of menopausal symptoms.
Research Methodologies
Numerous methodologies are employed in menopause research. Observational studies track changes over time, while randomized controlled trials rigorously evaluate the efficacy of interventions. Molecular studies delve into the cellular mechanisms underlying menopausal symptoms and associated diseases. Epidemiological studies examine the prevalence and risk factors for various health conditions related to menopause. These diverse approaches provide a comprehensive picture of menopause, encompassing its biological, psychological, and social dimensions.
Anticipated Outcomes
The anticipated outcomes of menopause research are substantial. Improved diagnostic tools for early detection of menopausal symptoms and associated health risks are a key goal. Tailored treatment strategies for managing menopausal symptoms and preventing long-term health issues are also anticipated. Ultimately, the aim is to personalize treatment plans based on individual needs and genetic predispositions, thus enhancing the quality of life for women experiencing menopause.
This personalization can be seen in examples of targeted hormone replacement therapies or lifestyle interventions, specific to individual needs.
Future Directions
Future research directions will focus on personalized medicine approaches. Research is likely to delve into the identification of biomarkers that predict an individual’s response to different treatments and interventions. The development of more effective and safer treatments, including non-hormonal options, is a critical area for future investigation. The integration of technology into monitoring and managing menopausal symptoms will likely play a pivotal role.
Examples include wearable devices that track hormonal fluctuations and provide personalized recommendations for lifestyle adjustments.
Key Research Areas, Methodologies, and Anticipated Outcomes
| Key Research Area | Research Methodology | Anticipated Outcomes |
|---|---|---|
| Impact of lifestyle factors on menopausal symptoms | Randomized controlled trials, observational studies, cohort studies | Development of tailored lifestyle interventions to alleviate symptoms, identification of risk factors |
| Genetic predisposition to menopausal health conditions | Genome-wide association studies, molecular studies | Improved identification of women at risk for specific conditions, development of personalized preventive strategies |
| Development of non-hormonal therapies | Randomized controlled trials, clinical trials | Increased treatment options for women who cannot or choose not to use hormone therapy, improved safety profiles |
| Role of gut microbiota in menopausal health | Metagenomic studies, interventional studies | Identification of gut microbiota imbalances linked to menopausal symptoms, development of targeted dietary interventions |
Menopause and Mental Health
Navigating the hormonal shifts of menopause can be challenging, impacting not just physical well-being but also emotional and mental health. Many women experience fluctuations in mood, anxiety, and even depression during this transitional period. Understanding the connection between these changes and potential support strategies is crucial for managing this life stage effectively.The intricate interplay between hormonal changes and the brain makes menopause a period where mental health can be significantly affected.
Estrogen, a key hormone, plays a vital role in brain function, mood regulation, and stress response. Fluctuations and decline in estrogen levels during menopause can lead to a range of emotional and mental health challenges.
The Link Between Menopause and Mental Health Conditions
Menopause is associated with an increased risk of developing or experiencing a worsening of existing mental health conditions, such as anxiety and depression. This is not a simple cause-and-effect relationship; rather, a complex interplay of biological, psychological, and social factors contributes to the experience. These factors often intertwine, making it difficult to isolate specific triggers.
Potential Risk Factors
Several factors can increase the risk of experiencing mental health challenges during menopause. Significant life changes, such as the transition to a new phase of life or the loss of a loved one, can significantly impact mental health, regardless of hormonal fluctuations. Pre-existing mental health conditions can also increase vulnerability during menopause.
Protective Factors
Conversely, certain factors can act as protective measures against negative mental health impacts. Strong social support networks, healthy lifestyle choices, and coping mechanisms can buffer the effects of hormonal changes. A positive outlook and resilience can also play a crucial role in navigating the challenges of menopause.
Importance of Mental Health Support
Seeking professional help is essential for women experiencing mental health challenges during menopause. Mental health support can provide evidence-based strategies and resources to manage symptoms effectively. Open communication with healthcare providers is vital for identifying and addressing potential issues. A multi-faceted approach that combines medical interventions, lifestyle adjustments, and emotional support is often the most effective strategy.
Potential Symptoms of Anxiety and Depression During Menopause
| Symptom | Description | Risk Factors | Support Resources |
|---|---|---|---|
| Anxiety | Excessive worry, fear, nervousness, panic attacks, restlessness, difficulty concentrating | Prior anxiety disorders, stressful life events, social isolation, lack of sleep | Therapists specializing in women’s health, support groups, relaxation techniques, medication |
| Depression | Persistent sadness, loss of interest in activities, changes in appetite or sleep, feelings of worthlessness or guilt, fatigue | Prior depressive disorders, hormonal fluctuations, relationship difficulties, financial strain | Therapists specializing in women’s health, support groups, medication, regular exercise |
The table above highlights some potential symptoms of anxiety and depression during menopause. It also suggests some risk factors and support resources that can assist women experiencing these challenges.
Menopause and Lifestyle
Navigating menopause can feel like a rollercoaster, but incorporating healthy lifestyle choices can significantly impact the experience. This journey is deeply personal, and understanding how diet, exercise, stress management, and sleep quality intertwine with menopausal symptoms is crucial for managing discomfort and overall well-being. From optimizing nutrition for bone health to finding stress-reducing techniques, proactive steps can make a substantial difference in quality of life during this transition.
The Impact of Diet on Menopausal Symptoms
Nutrition plays a vital role in managing menopausal symptoms. A balanced diet rich in fruits, vegetables, whole grains, and lean protein can provide essential nutrients, supporting overall health and potentially mitigating some menopausal discomforts. Choosing foods rich in calcium and vitamin D is particularly important for maintaining bone density, a concern often heightened during menopause. Foods high in phytoestrogens, like soy and flaxseeds, are sometimes highlighted for their potential to alleviate certain symptoms, although the evidence is not conclusive for all individuals.
Furthermore, adequate hydration is crucial for overall health and comfort during menopause.
The Role of Exercise in Managing Menopause
Regular physical activity is a cornerstone of managing menopause. Exercise can help regulate mood, improve sleep quality, and reduce stress, all factors that contribute to a more positive experience. The benefits of exercise extend beyond emotional well-being, as physical activity can contribute to bone health and maintain muscle mass, which is essential for preventing age-related decline. Moderate-intensity activities, such as brisk walking, swimming, or cycling, can be highly effective in managing menopausal symptoms and promoting overall well-being.
Consistency is key.
Stress Management Techniques for Menopause
Stress can exacerbate menopausal symptoms, affecting mood, sleep, and energy levels. Finding healthy ways to manage stress is essential for a smoother transition. Practices such as yoga, meditation, deep breathing exercises, and spending time in nature can significantly reduce stress levels and promote relaxation. Identifying and addressing sources of stress, whether work-related, relationship-based, or personal, is also crucial.
Prioritizing self-care and establishing a routine that incorporates relaxation techniques can dramatically improve the experience of menopause.
The Importance of Sleep Quality During Menopause
Adequate sleep is essential for overall health and well-being, and even more crucial during menopause. Sleep disturbances, a common symptom, can impact mood, energy levels, and cognitive function. Establishing a regular sleep schedule, creating a relaxing bedtime routine, and ensuring a comfortable sleep environment are crucial steps. Reducing caffeine and alcohol intake before bed can also improve sleep quality.
Consider consulting a healthcare professional if sleep disturbances persist or significantly impact daily life.
Nutrition and Bone Health During Menopause
Maintaining bone density is paramount during menopause due to the decrease in estrogen production. Adequate calcium and vitamin D intake are critical for preserving bone health. Calcium-rich foods, such as dairy products, leafy greens, and fortified cereals, are essential components of a bone-healthy diet. Sunlight exposure can help the body synthesize vitamin D, while dietary sources include fatty fish and fortified foods.
Regular weight-bearing exercise, such as walking or jogging, further supports bone health.
Lifestyle Factors and Their Impact on Menopause
| Lifestyle Factor | Impact on Menopause | Recommended Strategies |
|---|---|---|
| Diet | A balanced diet rich in fruits, vegetables, and calcium-rich foods can mitigate some symptoms and support overall health. | Prioritize whole foods, limit processed foods and sugar, and focus on calcium and vitamin D intake. |
| Exercise | Regular physical activity can improve mood, sleep quality, and bone health. | Incorporate at least 150 minutes of moderate-intensity exercise per week. |
| Stress Management | Stress can exacerbate menopausal symptoms. Effective stress management techniques are essential. | Practice relaxation techniques like yoga, meditation, or deep breathing. |
| Sleep | Adequate sleep is crucial for managing overall well-being and menopausal symptoms. | Establish a regular sleep schedule, create a relaxing bedtime routine, and optimize your sleep environment. |
Ending Remarks
In conclusion, menopause facts and statistics highlight the multifaceted nature of this life stage. By understanding the prevalence, symptoms, health impacts, and management options, we can better support women navigating this transition. This exploration emphasizes the importance of personalized care and holistic approaches to managing menopausal symptoms. Future research is crucial to continue improving outcomes for women.