Why am I getting headaches every day all of a sudden? This perplexing question plagues many, and understanding the potential causes is crucial for finding relief. Headaches can stem from various factors, ranging from simple lifestyle choices to underlying medical conditions. This exploration delves into the possible physical, lifestyle, environmental, and medical contributors to this frequent discomfort.
From the subtle tension in your neck to the throbbing intensity of a migraine, understanding the nuances of different types of headaches is key. We’ll examine the characteristics of common headaches like tension, migraine, and cluster headaches, comparing and contrasting their symptoms. Furthermore, we’ll explore the role of stress, sleep, diet, and environmental triggers in exacerbating these daily headaches.
Potential Physical Causes
Sudden and persistent daily headaches can be alarming. Understanding the potential physical triggers and their associated symptoms is crucial for determining the underlying cause and taking appropriate action. This section explores common physical causes, their characteristics, and the importance of seeking professional medical advice.
Ugh, daily headaches? I’ve been dealing with them out of the blue, and it’s driving me crazy. I’ve been researching everything from stress to dehydration, but nothing seems to quite hit the mark. While I’m not sure if drinking whiskey will help my headache, some people swear it helps with a cold, does whiskey help a cold , but I’m definitely not going to try that route.
I think I’ll need to see a doctor and get some professional advice on this sudden headache issue.
Common Physical Headache Triggers
Numerous physical factors can contribute to daily headaches. Dehydration, stress, and poor posture are common culprits, but other less obvious triggers exist. Identifying these triggers is often the first step toward effective management.
| Cause | Symptoms | Potential Triggers |
|---|---|---|
| Stress | Often described as a dull, pressing pain, typically located on both sides of the head. Can be accompanied by muscle tension and stiffness in the neck and shoulders. | High-pressure situations, deadlines, relationship problems, financial worries |
| Dehydration | A throbbing or aching sensation, often located in the temples or forehead. Can be accompanied by dizziness, fatigue, and a dry mouth. | Insufficient water intake, excessive sweating, prolonged physical activity |
| Poor Posture | A persistent, aching or throbbing pain, often localized in the back of the head or neck. Associated with neck stiffness and pain. | Prolonged periods of sitting or standing with poor posture, slouching, using electronic devices for extended periods |
| Eye Strain | A throbbing or aching pain around the eyes, often accompanied by eye fatigue, blurry vision, and sensitivity to light. | Prolonged screen time, poor lighting, focusing on small print, refractive errors (uncorrected vision problems) |
| Dental Issues | Pain located around the jaw or temple. Often triggered by chewing or biting. | Teeth grinding, temporomandibular joint (TMJ) disorders, cavities, abscesses |
| Sinus Infections | Pain centered around the forehead, cheeks, or nose. Often accompanied by facial pressure, nasal congestion, and fever. | Viral or bacterial infections, allergies, environmental irritants |
| Hormonal Fluctuations | Pain can vary in location and intensity. Associated with symptoms like mood changes and fatigue. | Menstruation, pregnancy, menopause |
Comparing Headache Types
Different types of headaches have distinct characteristics. Understanding these distinctions can aid in identifying the potential cause. This table illustrates the differences in location, intensity, duration, and accompanying symptoms.
| Headache Type | Location | Intensity | Duration | Accompanying Symptoms |
|---|---|---|---|---|
| Tension Headache | Usually bilateral (both sides of the head), often encompassing the forehead, temples, and back of the head. | Mild to moderate | 30 minutes to several hours | Muscle tenderness, neck stiffness, and fatigue. |
| Migraine | Often unilateral (one side of the head), but can be bilateral. May involve the temples, forehead, or back of the head. | Moderate to severe | 4-72 hours | Nausea, vomiting, sensitivity to light and sound, aura (visual disturbances) |
| Cluster Headache | Usually behind or around one eye, and can involve the forehead or temple. | Severe | 15-180 minutes | Redness and tearing in the affected eye, runny nose, restlessness, and nasal congestion. |
Importance of Professional Diagnosis
While this information provides insight into potential causes, it is crucial to remember that accurate diagnosis requires a consultation with a healthcare professional. Self-treating without a proper diagnosis can lead to delayed or mismanaged care. A medical evaluation is necessary to rule out any underlying serious conditions and determine the most appropriate course of action.
Lifestyle Factors
Daily headaches can stem from various lifestyle factors, significantly impacting their frequency and severity. Understanding the interplay between sleep, stress, and diet is crucial in managing these headaches. Addressing these factors can lead to a noticeable reduction in headache episodes.Lifestyle choices profoundly affect the body’s overall well-being, influencing its ability to cope with pain and discomfort. Poor sleep hygiene, high stress levels, and an unbalanced diet can all act as triggers, leading to a cascade of physiological responses that manifest as headaches.
Identifying these triggers and adopting proactive strategies to mitigate them is often the first step toward effective headache management.
Sleep Patterns and Headaches
Sleep deprivation and poor sleep quality are strongly linked to headache frequency. Adequate sleep allows the body to repair and restore itself, helping to prevent and manage pain. Disruptions to the sleep-wake cycle, whether due to insufficient sleep or irregular sleep schedules, can lead to increased headache susceptibility. This is because sleep plays a vital role in regulating neurochemicals and hormones that influence pain perception.
Individuals who consistently get less than 7-8 hours of sleep per night may find themselves more prone to headaches.
Stress Levels and Headaches
Stress is a powerful trigger for many types of headaches. Chronic stress can activate the body’s stress response system, leading to heightened muscle tension, hormonal imbalances, and increased sensitivity to pain. This can manifest as tension-type headaches or exacerbate existing conditions. Prolonged periods of stress can also weaken the body’s natural coping mechanisms, increasing the likelihood of experiencing headaches.
The stress response system plays a role in pain signaling. Chronic stress can cause a cascade of neurochemical changes that increase pain sensitivity.
Diet and Headaches
Diet plays a significant role in triggering headaches. Certain foods and beverages can directly stimulate the production of pain-causing substances in the body. Caffeine withdrawal or intake can trigger headaches, particularly in individuals sensitive to caffeine. Fluctuations in blood sugar levels, such as those caused by excessive sugar intake or prolonged periods without sufficient carbohydrate intake, can also contribute to headache development.
Individuals with specific food sensitivities, such as to certain types of cheeses or processed meats, might experience headaches as a reaction.
Stress Management Techniques
Effective stress management techniques can significantly reduce headache triggers. Various methods can help individuals regulate their stress responses. Meditation and mindfulness practices have shown promise in reducing stress levels and improving emotional regulation, thereby mitigating the likelihood of headaches. Yoga and deep breathing exercises can help to relax muscles and promote relaxation, thus potentially reducing headache pain.
The effectiveness of different techniques can vary from person to person. Experimentation and finding the methods that work best for an individual is key to successful stress management. Deep breathing exercises can be highly effective in reducing stress and promoting relaxation, lowering the potential for headache triggers.
Dietary Factors and Headaches
Certain dietary factors can significantly influence headache frequency and intensity. Caffeine withdrawal can induce headaches, as the body adjusts to the absence of the stimulant. Sugar spikes and crashes can lead to fluctuations in blood sugar levels, potentially contributing to headaches. Food sensitivities, such as those to certain types of dairy products, processed foods, or specific fruits, can trigger headaches in susceptible individuals.
A balanced diet, including a moderate intake of caffeine, and consistent blood sugar levels, are essential for preventing these triggers.
Environmental Factors
Your daily headaches might not be solely linked to internal factors. External elements, often overlooked, can significantly impact your well-being. Understanding environmental triggers can be crucial in managing and potentially preventing these persistent headaches.Environmental factors can interact with pre-existing conditions or lifestyle choices to intensify headache episodes. For example, someone with a history of tension headaches might find their symptoms worsen during periods of high stress and exposure to loud noises.
I’ve been battling daily headaches out of the blue, and I’ve been doing a lot of research. It turns out there’s a fascinating connection between hormones and gastrointestinal problems, which can sometimes trigger headaches. For example, hormones and gastrointestinal problems can sometimes disrupt the nervous system, leading to these unexpected headaches. I’m still trying to figure out the precise cause of my headaches, but I’m hoping understanding this link will help me pinpoint the issue.
Maybe it’s time to look into some changes in my diet or lifestyle.
Similarly, someone prone to migraines might experience heightened sensitivity to specific smells or changes in air pressure.
Environmental Triggers for Headaches
Environmental factors can trigger headaches in various ways, including influencing the body’s physiological responses. Changes in barometric pressure, temperature fluctuations, and air quality can all play a role. Certain smells, chemicals, and pollutants can also act as triggers, causing inflammation or altering neurochemical pathways.
Weather Patterns and Headaches
Fluctuations in weather patterns are frequently cited as triggers for headaches. Changes in barometric pressure, often associated with storms or rapid temperature shifts, can affect blood vessels and nerves, leading to pain. The sudden drop in temperature can also trigger headaches in susceptible individuals.
Exposure to Specific Smells
Certain scents, such as perfumes, cleaning products, or even certain foods, can act as triggers for some individuals. These smells can irritate the nasal passages and trigger a cascade of responses that lead to headache pain. In some cases, these triggers can also influence the body’s neurochemical processes, contributing to headache episodes.
Air Quality and Pollutants
Poor air quality, often characterized by high levels of pollutants like ozone, particulate matter, or volatile organic compounds (VOCs), can trigger headaches in susceptible individuals. Exposure to these pollutants can irritate the respiratory system, leading to inflammation and headache pain. Smog and other forms of air pollution are well-known headache triggers.
Noise Pollution and Headaches
Prolonged exposure to loud noises, such as traffic noise or construction, can contribute to headaches. The constant stimulation of the auditory system can lead to tension in the head and neck muscles, ultimately triggering headaches. This is particularly relevant in urban environments with high levels of noise pollution.
Common Environmental Headache Triggers
- Perfumes and strong scents
- Cleaning products containing ammonia or other harsh chemicals
- Pollutants such as ozone and particulate matter
- Changes in barometric pressure
- Sudden temperature drops or increases
- Loud noises and noise pollution
Environmental Factors, Symptoms, and Prevention Strategies
| Environmental Factor | Potential Symptoms | Prevention Strategies |
|---|---|---|
| Changes in weather patterns (e.g., barometric pressure changes) | Headache, migraine, tension-type headache | Monitor weather forecasts, stay hydrated, use pain relievers as needed |
| Exposure to strong smells (e.g., perfumes, cleaning products) | Headache, migraine, nasal irritation | Avoid strong scents, use air purifiers, ventilate rooms, wear a mask |
| Poor air quality (e.g., pollutants like ozone, VOCs) | Headache, respiratory issues | Stay indoors during high pollution days, use air purifiers, wear a mask outdoors |
| Noise pollution (e.g., traffic, construction) | Headache, tension-type headache, stress | Minimize exposure to loud noises, use earplugs or noise-canceling headphones, take breaks from loud environments |
Medical Conditions
Daily headaches can stem from various underlying medical conditions. It’s crucial to understand that persistent headaches, especially those that are new or different from your usual experience, demand investigation. Ignoring these symptoms can lead to delayed diagnosis and potentially more severe complications. Proper medical evaluation is vital for identifying the root cause and developing an effective treatment plan.Medical conditions can significantly impact your well-being and daily life.
Ugh, daily headaches are seriously no fun! I’ve been dealing with them out of the blue, and I’m starting to wonder if my diet might be playing a role. Maybe incorporating more fiber into my meals could help. Recent research suggests that apple pectin, a soluble fiber found in apples, could be a game changer for digestive health, potentially reducing inflammation and improving gut function.
Exploring the benefits of apple pectin might be key to finding a solution to these pesky headaches. the benefits of apple pectin I’m hoping that tweaking my gut health with this natural fiber could finally stop these daily headaches for good.
Many of these conditions, if left untreated, can lead to a range of health problems. Early detection and intervention are key to managing these issues effectively.
Potential Medical Conditions
A variety of medical conditions can cause daily headaches. These conditions often present with additional symptoms beyond just head pain. Recognizing these additional symptoms can aid in early diagnosis and appropriate treatment.
- Sinus Infections: Sinus infections, also known as sinusitis, are characterized by inflammation of the sinus cavities. Common symptoms include facial pain or pressure, nasal congestion, and a thick, discolored nasal discharge. In some cases, fever and a cough can also be present.
- Teeth Grinding (Bruxism): Chronic teeth grinding can lead to significant head pain, often felt in the temples or jaw. Additional symptoms may include jaw pain, a stiff jaw, and teeth sensitivity. The grinding action itself can also cause wear and tear on the teeth over time.
- Neck Injuries: Whiplash or other neck injuries can trigger persistent headaches. These injuries may cause pain and stiffness in the neck, and can radiate to the head and shoulders. Symptoms often include difficulty moving the neck and pain that worsens with movement.
- Migraines: Migraines are a type of severe headache that can be debilitating. They typically involve throbbing pain, often on one side of the head. Accompanying symptoms may include nausea, vomiting, and extreme sensitivity to light and sound.
- Cluster Headaches: Cluster headaches are characterized by severe, intense pain, usually located around one eye. These headaches occur in clusters, with periods of intense pain followed by periods of remission. The pain often involves a burning or stabbing sensation.
- Tension Headaches: Tension headaches are often described as a dull, pressing pain, like a tight band around the head. These headaches can range from mild to moderate in intensity and may be accompanied by muscle tension in the neck and shoulders.
Symptoms Warranting Immediate Medical Attention, Why am i getting headaches every day all of a sudden
Certain headache symptoms necessitate immediate medical attention. These symptoms often indicate a serious underlying condition requiring urgent evaluation and treatment.
- Sudden, severe headache accompanied by a stiff neck, fever, or confusion.
- Headache accompanied by numbness or weakness in an arm or leg.
- Headache with a sudden loss of vision or speech.
- Headache that worsens significantly and rapidly over a short period.
- Headache associated with seizures or other neurological symptoms.
Potential Long-Term Consequences of Untreated Headaches
Untreated headaches, especially those stemming from underlying medical conditions, can have detrimental long-term consequences. Prolonged pain can negatively affect daily life and lead to emotional distress and decreased quality of life.
- Chronic pain and discomfort.
- Reduced productivity and work performance.
- Difficulty concentrating and learning.
- Sleep disturbances and fatigue.
- Increased risk of depression and anxiety.
Importance of Seeking Medical Advice
Persistent headaches, regardless of their cause, should prompt a consultation with a healthcare professional. Early diagnosis and treatment are crucial for managing headaches effectively and preventing potential complications. A medical expert can determine the cause and recommend the most appropriate course of action.
- Professional diagnosis is essential for effective management.
- A healthcare professional can assess the severity and potential causes of the headaches.
- Treatment plans are tailored to address the specific cause and symptoms.
- Long-term health and well-being are protected by addressing the underlying issue.
Medication and Supplements: Why Am I Getting Headaches Every Day All Of A Sudden
Daily headaches can sometimes be linked to the medications we take, both over-the-counter and prescription. Understanding these potential connections is crucial for effective headache management. This section explores the possible roles of various medications and supplements in triggering or exacerbating headaches.Medications, while intended to alleviate pain and discomfort, can sometimes paradoxically lead to new or worsening headaches. This can stem from the medication’s direct impact on the body or from its interaction with other substances.
It’s important to be aware of these possibilities and to carefully consider the potential side effects.
Potential Link Between Medications and Headaches
Many over-the-counter pain relievers, such as ibuprofen and aspirin, can be effective for treating headaches. However, overuse or improper use can trigger rebound headaches, where the pain relief medication itself becomes a cause of further pain. Similarly, prescription medications, including some blood pressure medications and antidepressants, can sometimes cause headaches as a side effect.
Side Effects of Certain Medications
Different medications have different potential side effects. For instance, some blood pressure medications can cause headaches, dizziness, and nausea. Antihistamines, often used for allergies, can lead to headaches as a secondary effect. Careful attention to medication labels and discussions with healthcare professionals can help to identify and mitigate these risks.
Importance of Discussing Medication Use with a Healthcare Professional
Open communication with your doctor about all medications, including over-the-counter drugs and supplements, is vital. This allows your healthcare provider to assess the potential interactions and identify any possible correlations between medication use and your headaches. A thorough medical history is essential for understanding the potential impact of various substances.
Comparison of Pain Relief Options
Various pain relief methods exist, each with its own advantages and disadvantages. Over-the-counter pain relievers, such as ibuprofen and acetaminophen, offer quick relief for mild to moderate headaches but may carry risks of side effects if taken excessively. Prescription medications, when prescribed by a doctor, can often offer more targeted relief but may have more significant potential side effects.
Alternative therapies, like relaxation techniques and biofeedback, may help manage underlying tension-type headaches, but are not always effective for more severe types of headaches.
Herbal Remedies and Supplements
Some herbal remedies and supplements, like feverfew, butterbur, and magnesium, are sometimes used for headache relief. However, the effectiveness of these remedies for headaches varies, and there is a lack of rigorous scientific evidence supporting their efficacy in many cases. Furthermore, some herbal remedies and supplements can interact with other medications, potentially leading to adverse effects. Always consult with a healthcare professional before incorporating any herbal remedy or supplement into your routine.
Important note: Self-treating with herbal remedies or supplements can be risky, especially if you have underlying health conditions. It’s crucial to prioritize professional medical guidance before making any changes to your treatment plan.
Diagnostic Procedures
Figuring out the root cause of your daily headaches requires a methodical approach. A thorough evaluation by a healthcare professional is crucial to pinpoint the specific reason behind these persistent headaches. This process involves a combination of physical examinations, neurological assessments, and potentially, imaging scans. The accuracy of the diagnosis directly influences the effectiveness of the subsequent treatment plan.The medical evaluation for headaches typically begins with a detailed history.
This involves discussing the frequency, intensity, location, and characteristics of the headaches, as well as any associated symptoms. Factors like stress levels, recent lifestyle changes, or underlying medical conditions are also considered. This initial assessment helps narrow down potential causes and guides the subsequent diagnostic steps.
Physical Examinations
Physical examinations are fundamental in assessing overall health and identifying any physical signs related to headaches. These examinations often include checking vital signs like blood pressure, heart rate, and temperature. The doctor will also examine the head and neck for any abnormalities, tenderness, or swelling. A thorough neurological examination is often part of this process, assessing reflexes, coordination, and cranial nerve function.
This multifaceted approach helps to identify potential underlying conditions.
Neurological Tests
Neurological tests are designed to evaluate the function of the nervous system. These tests can include assessments of reflexes, coordination, sensation, and strength. Specific tests may be employed to evaluate cranial nerve function, which can be impacted by various conditions. These tests are essential in detecting neurological problems that could be contributing to the headaches. Neurological tests help determine if the headaches are associated with a more serious neurological condition.
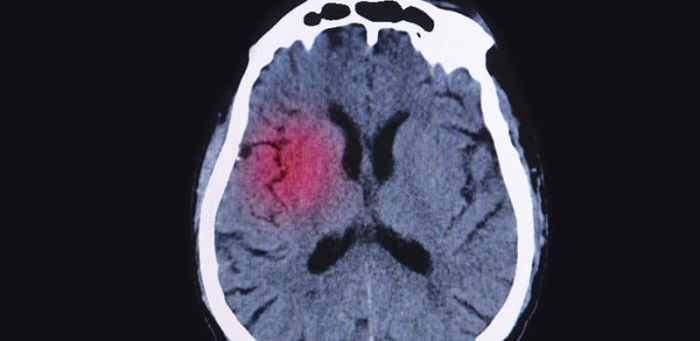
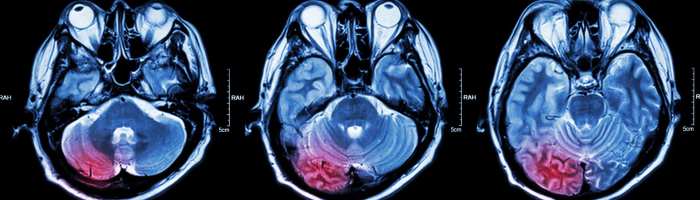
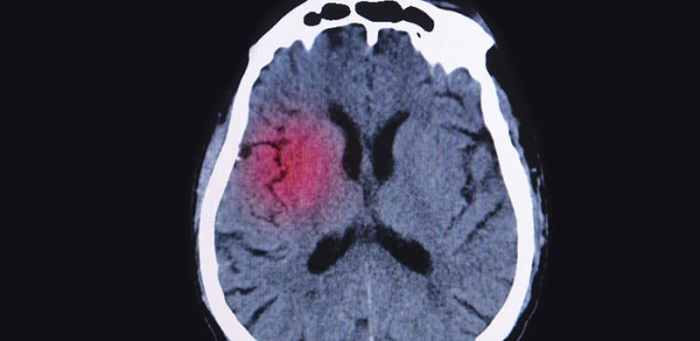
Imaging Scans
Imaging scans, such as CT scans and MRIs, are powerful tools for visualizing the structures within the head. These scans can identify potential structural abnormalities, tumors, or other abnormalities that might be causing the headaches. CT scans are often preferred for detecting bony structures and calcium deposits, while MRIs offer a clearer view of soft tissues and blood vessels.
The choice of scan depends on the suspected cause and the specific symptoms. Imaging scans are particularly valuable in ruling out potentially serious conditions.
Diagnostic Tests Summary
| Diagnostic Test | Purpose | Typical Outcomes |
|---|---|---|
| Physical Examination | Assess overall health, identify physical signs related to headaches | Normal findings, identification of tenderness or swelling, abnormal reflexes |
| Neurological Tests | Evaluate nervous system function, check reflexes, coordination, and sensation | Normal function, abnormal reflexes, altered coordination, or reduced sensation. |
| CT Scan | Visualize bony structures and calcium deposits within the head | Normal scan, presence of tumors, blood clots, or structural abnormalities |
| MRI | Visualize soft tissues and blood vessels within the head | Normal scan, identification of tumors, abnormalities in blood vessels, or structural problems. |
Role of Specialists
A neurologist or headache specialist possesses specialized knowledge and experience in diagnosing and managing headaches. They can provide a comprehensive evaluation, conduct advanced tests, and develop a tailored treatment strategy. These specialists are crucial in complex cases or when the cause of the headaches remains unclear after initial evaluations. The involvement of a specialist is important in cases where the headaches are severe, persistent, or associated with other concerning symptoms.
Ultimate Conclusion
In conclusion, the sudden onset of daily headaches demands a thorough investigation into potential causes. From physical factors like dehydration and poor posture to lifestyle choices and underlying medical conditions, the root of the problem varies. Consulting a healthcare professional for a proper diagnosis and tailored treatment plan is essential for effective management. This comprehensive exploration provides a starting point for understanding the multifaceted nature of headaches and empowers individuals to take proactive steps toward finding lasting relief.