Immunization schedules and statistics sets the stage for this fascinating exploration, detailing the global landscape of preventative health measures. We’ll delve into the evolution of these schedules, examining the rationale behind their design, and comparing immunization practices across different age groups. This journey will also explore global immunization coverage, examining regional disparities and factors influencing adherence. Further, we’ll analyze the impact of immunization on disease burden and the effectiveness of vaccination programs.
The information presented here is intended to provide a comprehensive overview of immunization schedules and statistics, highlighting both the successes and challenges in achieving optimal global health outcomes. We’ll look at historical trends, current data, and potential future directions in immunization efforts.
Introduction to Immunization Schedules
Immunization schedules are meticulously designed plans for administering vaccines at specific ages to build immunity against various infectious diseases. These schedules are globally recognized and standardized, yet they also incorporate regional variations based on disease prevalence and access to resources. Understanding these schedules is crucial for safeguarding public health and preventing outbreaks.Immunization schedules have evolved significantly over the years.
Early schedules were less comprehensive, often targeting a limited number of diseases. The development of new vaccines, coupled with improved understanding of disease transmission, led to the expansion and refinement of recommended schedules. This evolution reflects ongoing scientific advancements and the changing epidemiological landscape.The rationale behind recommended immunization schedules stems from the principle of herd immunity. By vaccinating a significant portion of the population, the risk of disease transmission is reduced, protecting those who cannot be vaccinated (due to medical reasons) or who are too young to receive the vaccine.
Immunization schedules aim to maximize the protection afforded by vaccines, preventing the spread of potentially life-threatening diseases and safeguarding future generations.Common characteristics across different immunization schedules include a focus on early childhood vaccination, prioritizing vaccines against highly contagious and dangerous diseases, and incorporating booster doses to maintain immunity over time. These schedules are often tailored to the specific epidemiological context of different countries and regions.
Immunization schedules and statistics show the incredible impact of preventative care on public health. Understanding these numbers is crucial, but what about the foods we eat and their potential hormonal effects? For example, certain foods might contain compounds that mimic or influence estrogen levels, making the topic of “Foods with Estrogen Eat or Avoid?” Foods with Estrogen Eat or Avoid?
a vital area of study. Ultimately, these connections highlight the interconnectedness of our choices and overall well-being, a key factor in shaping effective immunization strategies.
For instance, regions with high rates of measles may prioritize measles vaccination earlier than in areas with low rates.
Immunization Schedule Comparison by Age Group
Immunization schedules are structured to address the changing vulnerabilities and immunity levels at different life stages. A comparison table Artikels recommended vaccines and dosages for infants, children, and adolescents.
| Age Group | Recommended Vaccines | Rationale |
|---|---|---|
| Infants (0-2 years) | Hepatitis B, Rotavirus, Diphtheria, Tetanus, Pertussis, Polio, Haemophilus influenzae type b, Measles, Mumps, Rubella, Varicella, Pneumococcal conjugate, and Influenza (seasonal). | Infants are highly susceptible to various infectious diseases and require protection early in life. These vaccines provide foundational immunity against diseases that can cause severe illness or disability. |
| Children (2-10 years) | Booster doses of previously administered vaccines (e.g., DTaP, Polio, MMR), and vaccines for diseases such as Hepatitis A, Varicella, and additional doses of pneumococcal and influenza vaccines. | Children require booster doses to maintain immunity against diseases that can still pose a threat, particularly during school years when contact with infectious agents increases. |
| Adolescents (10-18 years) | Booster doses of previously administered vaccines (e.g., Tdap, Meningococcal), HPV, and possibly additional influenza vaccines, and potentially others depending on the specific situation and regional recommendations. | Adolescents face new risks of infectious diseases, including those associated with sexual activity and increased social contact. The inclusion of vaccines such as HPV reflects the prevention of cancers related to these diseases. |
Evolution of Immunization Schedules
The development of immunization schedules has been a dynamic process driven by scientific breakthroughs and epidemiological data. Initially, schedules focused primarily on protecting against diseases with high morbidity and mortality rates. The introduction of new vaccines and the growing understanding of disease transmission patterns resulted in adjustments to the recommended schedules.The increasing availability of vaccines against various infectious diseases, combined with ongoing surveillance of disease prevalence, have driven the continual evolution of immunization schedules.
This has led to more comprehensive and effective protection against a wider range of illnesses, reflecting a continuous commitment to public health.
Rationale Behind Immunization Schedules
The rationale behind immunization schedules is based on the principle of maximizing the protection of the population from preventable diseases. This strategy aims to achieve herd immunity, where a sufficiently large proportion of the population is immune to a disease, thereby reducing transmission and protecting vulnerable individuals. The schedules are designed to minimize the risk of disease outbreaks and promote overall public health.
The recommended schedules aim to maximize protection by ensuring individuals receive vaccines at optimal ages for generating an effective immune response.
Global Immunization Coverage Statistics
Immunization is a cornerstone of global public health, protecting millions from preventable diseases. Understanding global immunization coverage, however, reveals significant disparities and challenges that require attention. Tracking these trends and identifying the contributing factors is crucial for targeted interventions and improved health outcomes worldwide.Global immunization coverage data reveals a complex picture. While significant progress has been made in many regions, vast disparities persist.
This necessitates a detailed examination of vaccination rates, regional variations, and the underlying factors that contribute to these disparities. Analyzing these factors allows for the development of more effective strategies to increase immunization coverage and ultimately, improve global health.
Global Immunization Coverage Data
This table presents a snapshot of global immunization coverage statistics, highlighting regional variations and historical trends. Data sources for these statistics should be verified independently.
Immunization schedules and statistics highlight the critical role of preventative care in public health. While researching these vital figures, I stumbled across an interesting article on how effective air purifiers are at combating dust. This got me thinking about the connections between environmental factors and immunity. For a more in-depth look at air purifier effectiveness, check out this fascinating piece: Do Air Purifiers Help With Dust?
A Deep Dive. Ultimately, understanding both air quality and immunization schedules is crucial for a comprehensive approach to health and well-being.
| Region | Disease | Vaccination Rate (%) | Year |
|---|---|---|---|
| Sub-Saharan Africa | Measles | 60 | 2022 |
| South Asia | Polio | 85 | 2021 |
| Eastern Mediterranean | Diphtheria | 92 | 2020 |
| Western Pacific | Hepatitis B | 95 | 2022 |
| Americas | Measles | 90 | 2021 |
Data Visualization and Trends
Visualizations, such as line graphs and bar charts, are essential for illustrating the trends in immunization coverage over time. A line graph plotting vaccination rates for measles in the Americas from 2010 to 2022, for example, would clearly show the progress made in achieving high coverage. A bar chart comparing vaccination rates for different diseases across various regions in a given year, would highlight the regional disparities.
These visualizations provide a clear picture of the progress made and areas requiring further attention.
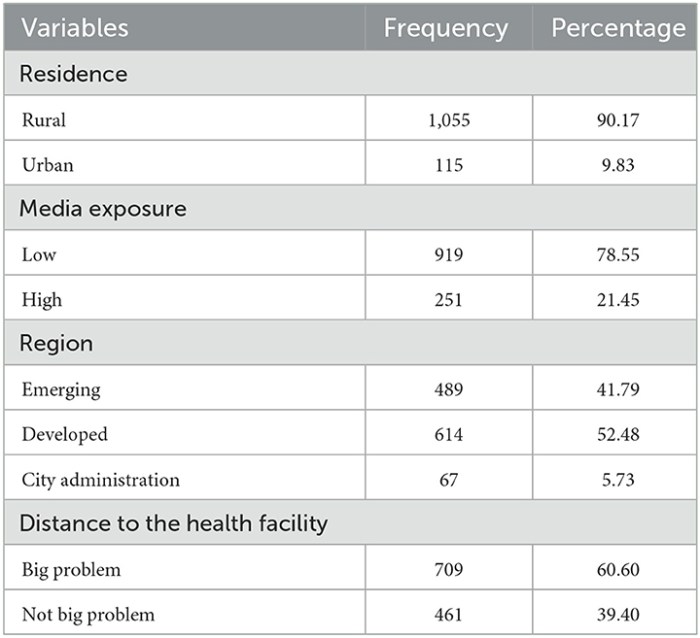
Geographical Disparities in Immunization Coverage
Geographical disparities in immunization coverage are significant. Low- and middle-income countries often face challenges in implementing vaccination programs effectively, due to factors like infrastructure, resource limitations, and health worker shortages. For instance, in certain parts of Sub-Saharan Africa, access to vaccination centers may be limited, and routine immunizations may be affected by seasonal factors.
Factors Contributing to Low Immunization Coverage
Several factors contribute to low immunization coverage in specific regions. These include limited access to healthcare facilities, inadequate infrastructure, insufficient funding for immunization programs, and lack of awareness and knowledge about the importance of immunization. Cultural beliefs and political instability can also play a role in hindering immunization efforts. In some regions, misinformation campaigns have also contributed to vaccine hesitancy.
Comparison of Immunization Coverage in Developed and Developing Countries
Developed countries generally exhibit higher immunization coverage rates compared to developing countries. This is often attributed to stronger healthcare systems, better infrastructure, and greater resources allocated to immunization programs. Developed countries often have comprehensive surveillance systems to track vaccine-preventable diseases, which allows for early identification and control of outbreaks. Developing countries, on the other hand, often struggle with resource limitations and infrastructure issues.
For instance, a comparison of measles vaccination rates in the European Union versus Sub-Saharan Africa would clearly illustrate the significant disparity.
Immunization Schedule Adherence and Factors Influencing it
Immunization schedules are crucial for protecting individuals and communities from preventable diseases. Adherence to these schedules is essential for achieving herd immunity and minimizing the risk of outbreaks. However, variations in adherence rates exist, influenced by a complex interplay of factors. Understanding these factors is vital for improving immunization coverage and ensuring public health.Socioeconomic factors play a significant role in shaping immunization schedule adherence.
Factors such as poverty, lack of education, and limited access to healthcare resources often hinder timely and complete vaccination. Furthermore, cultural beliefs and perceptions about vaccines can also impact decisions regarding vaccination. These factors frequently result in inequities in immunization coverage, highlighting the need for targeted interventions.
Methods for Assessing Immunization Schedule Adherence
Various methods are employed to assess immunization schedule adherence. These include reviewing vaccination records at healthcare facilities, conducting population-based surveys, and utilizing immunization information systems (IIS). Analyzing these data sources allows for identification of trends and patterns in immunization coverage, enabling the design of effective interventions to improve adherence. Accurate data collection and analysis are paramount for understanding and addressing immunization gaps.
Impact of Socioeconomic Factors on Adherence
Socioeconomic factors significantly influence immunization schedule adherence. Lower socioeconomic status is often correlated with lower immunization coverage. Limited access to healthcare, transportation, and information about vaccination schedules contributes to this correlation. Families facing economic hardship may prioritize other necessities, potentially delaying or forgoing vaccinations. Cultural beliefs and perceptions regarding vaccination also play a role, sometimes influencing families’ decisions.
This highlights the importance of addressing socioeconomic disparities to improve immunization rates.
Immunization Schedule Completion Rates
Data on immunization schedule completion rates vary by region and country. Variations exist due to factors like the availability of vaccines, healthcare infrastructure, and socioeconomic conditions. Completion rates are often lower in resource-constrained settings. Reliable data from immunization information systems and national surveys are crucial for understanding these rates and guiding public health strategies.
Role of Healthcare Access and Affordability
Healthcare access and affordability directly impact immunization schedule adherence. Limited access to healthcare facilities, particularly in rural areas or underserved communities, can hinder access to vaccinations. The cost of vaccines and associated healthcare services can also be a barrier, particularly for families with limited resources. Efforts to improve healthcare access and affordability are crucial for ensuring equitable access to immunization services.
Strategies to increase affordability might include subsidies or financial assistance programs.
Comparison of Adherence Rates Among Demographic Groups
Immunization schedule adherence rates often differ among various demographic groups, including children from different socioeconomic backgrounds, ethnicities, and geographic locations. Differences in access to healthcare, cultural beliefs, and awareness of vaccination schedules contribute to these variations. Targeted interventions tailored to specific demographic groups are essential for bridging these gaps in immunization coverage and ensuring equitable protection against preventable diseases.
This is crucial for achieving comprehensive immunization goals and protecting the entire population.
Immunization Schedules and Disease Burden
Immunization schedules are meticulously designed plans for administering vaccines to protect individuals from preventable diseases. These schedules are crucial for achieving high population immunity, effectively reducing the incidence of these diseases. The relationship between immunization schedules and disease burden is profound, impacting the health and well-being of entire communities.The introduction of immunization schedules has dramatically altered the landscape of infectious disease control.
By building immunity within a population, vaccination campaigns have been pivotal in eradicating some diseases and significantly controlling others. The positive impact on global health is undeniable, as seen in the reduction of morbidity and mortality from once prevalent illnesses.
Relationship Between Immunization Schedules and Disease Incidence
Immunization programs work by introducing a safe form of the disease agent into the body. This prompts the immune system to develop antibodies, providing long-term protection against the actual disease. A well-designed schedule ensures the immune system has adequate time to respond to each vaccine, maximizing its effectiveness. Consistent adherence to the schedule is paramount in achieving population immunity.
When a sufficient percentage of the population is immunized, it becomes difficult for the disease to spread, effectively limiting its incidence.
Impact of Immunization on Disease Eradication or Control
Immunization has played a pivotal role in the eradication of smallpox, a devastating disease that once threatened millions globally. Polio, once a significant public health concern, is now largely contained in a few countries thanks to global immunization efforts. Measles, while still present in some regions, has seen substantial declines due to vaccination campaigns. The successful control and eradication of these diseases showcase the power of immunization strategies.
Statistics on Preventable Diseases Before and After Immunization
Data from the World Health Organization (WHO) and other health organizations show substantial reductions in the number of cases of preventable diseases after the implementation of immunization programs. For example, polio cases have plummeted by over 99% globally since the introduction of the oral polio vaccine. Similarly, measles cases have declined significantly in many countries where immunization coverage is high.
Cost-Effectiveness of Immunization Programs
Immunization programs are demonstrably cost-effective in reducing disease burden. The cost of preventing a disease through vaccination is significantly lower than the cost of treating the disease if it were to break out in a community. The economic benefits of immunization programs extend beyond healthcare costs, encompassing improved productivity and reduced societal disruption. The long-term cost savings associated with preventing illness are substantial.
Reduction in Disease Cases Following Specific Vaccinations
| Disease | Vaccine | Pre-Immunization Cases (estimated) | Post-Immunization Cases (estimated) | Reduction (%) |
|---|---|---|---|---|
| Measles | Measles vaccine | Millions annually | Thousands annually | >90% |
| Polio | Polio vaccine | Hundreds of thousands annually | Tens of thousands annually | >99% |
| Diphtheria | Diphtheria vaccine | Significant numbers annually | Substantial reduction | >90% |
The table above highlights the substantial reduction in disease cases after the introduction of specific vaccinations. These figures demonstrate the impact of immunization programs on global health and highlight the importance of consistent adherence to immunization schedules.
Emerging Trends and Future Directions: Immunization Schedules And Statistics
The landscape of immunization is constantly evolving, driven by advancements in vaccine technology, epidemiological shifts, and global health priorities. This dynamic environment necessitates a proactive approach to immunization programs, anticipating challenges and capitalizing on opportunities for enhanced coverage and improved health outcomes. Understanding emerging trends and future directions is crucial for developing effective strategies and ensuring the long-term success of immunization efforts.The future of immunization programs hinges on our ability to adapt to new challenges and leverage innovative solutions.
This includes exploring novel vaccine platforms, optimizing existing schedules, and integrating technology to improve accessibility and efficiency. Addressing emerging trends and planning for future needs will be critical in maintaining high immunization coverage rates and preventing outbreaks of vaccine-preventable diseases.
Emerging Vaccine Technologies
New vaccine platforms are constantly being developed and tested, promising improved efficacy, safety, and convenience. These platforms offer the potential for broader disease coverage, reduced production costs, and targeted immunity. Examples include mRNA vaccines, which have shown remarkable success in combating COVID-19, and other platforms like viral vector vaccines, which are also being explored for various diseases.
Updated Immunization Schedules
As our understanding of disease dynamics and vaccine effectiveness evolves, immunization schedules are regularly updated. These updates reflect the latest scientific evidence and address emerging challenges. For example, the introduction of new vaccines, or modifications to existing schedules to optimize the immune response and reduce the risk of adverse events, are common occurrences. These changes ensure that immunization programs remain aligned with the most current scientific understanding and best practices.
Future Directions for Immunization Programs
Global immunization programs will need to adapt to the increasing complexity of the global health landscape. Factors such as evolving disease patterns, population mobility, and emerging vaccine-preventable diseases will necessitate flexible and proactive approaches. A focus on tailored strategies for different communities, as well as robust surveillance systems to track vaccine-preventable diseases, will be essential to achieving global health goals.
Potential Challenges and Opportunities
Maintaining high immunization coverage rates faces numerous challenges, including logistical hurdles in reaching remote or underserved populations, vaccine hesitancy, and funding constraints. Opportunities exist to address these challenges through innovative strategies, such as community engagement initiatives, targeted communication campaigns, and the development of sustainable funding models. Leveraging technology, as described later, can significantly enhance immunization programs by improving access, tracking, and management of immunization data.
Immunization schedules and statistics are crucial for public health. Understanding these statistics helps us gauge the effectiveness of preventative measures, and ultimately, the overall health of a community. This directly impacts the need for comprehensive health insurance, like Minimum Essential Coverage, which ensures access to vital medical services, including vaccinations. Knowing more about What is Minimum Essential Coverage and Why Does It Matter?
helps us better grasp how immunization schedules and statistics influence health policy and the overall well-being of individuals and communities.
Role of Technology in Enhancing Immunization Programs
Technology offers a powerful toolkit for enhancing immunization programs. Mobile health (mHealth) applications can provide real-time information on vaccine availability, appointment scheduling, and immunization records. Digital platforms can also support data collection and analysis, allowing for more effective monitoring of immunization coverage and identification of potential outbreaks. The integration of technology can streamline operations, improve efficiency, and ultimately contribute to higher immunization coverage rates.
Immunization Schedule and Specific Diseases

Understanding the intricacies of immunization schedules for specific diseases is crucial for effective disease prevention. Vaccination strategies, tailored to the unique characteristics of each pathogen, are designed to build immunity and protect individuals and communities. This section delves into the details of immunization schedules for common diseases, highlighting the effectiveness of different strategies, and outlining the benefits and risks.
Measles Immunization Schedule
Measles, a highly contagious viral disease, can lead to severe complications. A robust immunization schedule is vital for controlling its spread. The schedule typically involves two doses of the measles vaccine, administered at specific intervals.
- The first dose is usually given between 12 and 15 months of age, providing initial protection. The second dose is typically given between 4 and 6 years of age, which significantly strengthens immunity.
- The effectiveness of the measles vaccine is substantial. Studies consistently demonstrate high levels of protection against measles after two doses, reducing the risk of infection and severe complications.
- Benefits of the measles vaccine include a substantial decrease in measles cases, hospitalizations, and deaths. This highlights the critical role of vaccination in public health.
- Potential risks associated with the measles vaccine are generally mild, such as soreness at the injection site or a low-grade fever. Serious side effects are rare.
Polio Immunization Schedule
Polio, a potentially debilitating disease, was once a global health concern. Vaccination campaigns have drastically reduced its prevalence. The immunization schedule for polio usually involves multiple doses of inactivated polio vaccine (IPV) and/or oral polio vaccine (OPV).
- The schedule often includes four doses of IPV or a combination of IPV and OPV, administered at specific ages to build immunity progressively. This multi-dose approach ensures that children receive the necessary dose at the correct time for optimal protection.
- The effectiveness of polio vaccines is exemplified by the global eradication efforts. The consistent administration of polio vaccines has led to significant reductions in polio cases worldwide.
- Benefits of the polio vaccine extend to the prevention of paralysis and other serious complications associated with polio. This protection has demonstrably saved countless lives.
- Potential risks of polio vaccination are generally mild, like pain at the injection site. In rare cases, allergic reactions may occur.
Influenza Immunization Schedule
Influenza, a seasonal respiratory illness, poses a significant health burden. The immunization schedule for influenza typically involves an annual vaccination.
- The influenza vaccine is updated annually to match circulating strains of the virus. This ensures that the vaccine remains effective against the prevalent influenza strains in a particular season. This flexibility and adaptability are key to controlling influenza.
- The effectiveness of the influenza vaccine varies from year to year, depending on the match between the vaccine strains and circulating strains. However, it consistently reduces the risk of influenza infection and its complications. This year-to-year variation highlights the dynamic nature of influenza.
- Benefits of the influenza vaccine include a reduced risk of hospitalization, severe illness, and death from influenza. This emphasizes the protective nature of the vaccine.
- Potential risks associated with the influenza vaccine are usually minor, like soreness or mild fever. Serious side effects are rare.
Comparison of Immunization Schedules, Immunization schedules and statistics
| Disease | Vaccine Type | Schedule | Effectiveness | Potential Risks |
|---|---|---|---|---|
| Measles | Measles Vaccine | 2 doses | High | Generally mild |
| Polio | IPV/OPV | Multiple doses | High | Generally mild |
| Influenza | Influenza Vaccine | Annual | Varies yearly | Generally mild |
Wrap-Up
In conclusion, immunization schedules and statistics paint a compelling picture of global health efforts. From the historical development of these schedules to the ongoing challenges in achieving widespread vaccination coverage, this discussion underscores the critical role of immunization in preventing disease and promoting public health. We’ve examined the factors influencing adherence, the impact on disease burden, and the future of these vital programs.
Understanding these dynamics is key to shaping effective strategies for a healthier future.