Ehlers danlos syndrome overview – Ehlers-Danlos syndrome overview explores this complex group of connective tissue disorders. These conditions, often inherited, affect the body’s structure and function, impacting everything from skin elasticity to joint stability. This overview delves into the different types of EDS, their unique symptoms, and the challenges faced by those living with the condition. We’ll also explore the current understanding of diagnosis, treatment, and ongoing research.
The diversity of EDS types and symptoms is a key component. From hypermobile EDS to vascular EDS, each presents a unique set of challenges. Understanding the genetic basis and comparing symptoms across types provides crucial insight for individuals and healthcare professionals.
Introduction to Ehlers-Danlos Syndrome
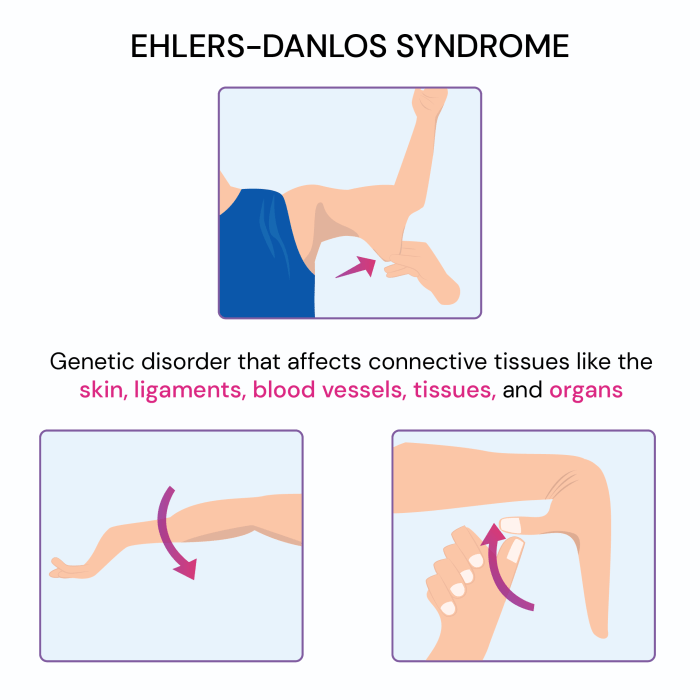
Ehlers-Danlos syndrome (EDS) is a group of inherited connective tissue disorders characterized by hypermobility of joints, skin fragility, and often, a range of other symptoms. These disorders affect the body’s connective tissues, which provide support and structure to various parts of the body, impacting everything from skin elasticity to joint stability. Understanding the diverse types of EDS is crucial for proper diagnosis and management of the condition.The genetic basis of EDS lies in mutations within genes responsible for producing proteins crucial for connective tissue function.
These proteins, like collagen and elastin, are vital components of tissues that provide strength, flexibility, and resilience. Variations in these genes can lead to a spectrum of symptoms, ranging from mild to severe, highlighting the complex interplay between genetics and phenotype.
Types of Ehlers-Danlos Syndrome
EDS encompasses several distinct types, each with its own set of characteristics and genetic underpinnings. Understanding these variations is vital for personalized treatment plans.
Genetic Basis of EDS
The genetic foundation of EDS involves mutations in various genes that encode proteins essential for connective tissue formation. These proteins play critical roles in maintaining the integrity and functionality of different tissues throughout the body. The specific genes implicated in each type of EDS can vary significantly.
Ehlers-Danlos syndrome (EDS) is a fascinating genetic disorder affecting connective tissues. It can cause a wide range of symptoms, and one often overlooked aspect is how it affects skeletal development. While some people wonder when their feet stop growing, for those with EDS, the answer isn’t always straightforward, and it can impact growth patterns in unexpected ways. Knowing more about typical foot growth patterns can help you understand the intricacies of EDS, and how individual cases may vary.
More information on when feet typically stop growing can be found here: when do feet stop growing. Ultimately, a deeper understanding of EDS requires a holistic approach, considering the range of potential impacts on physical development.
Comparison of EDS Types
| Type | Symptoms | Genetic Basis | Common Characteristics |
|---|---|---|---|
| Classical EDS | Hypermobile joints, skin hyperextensibility, easy bruising, and tissue fragility. Some individuals may also experience joint dislocations, scoliosis, and dental problems. | Mutations in the COL5A1 and COL5A2 genes, which encode proteins crucial for collagen type V synthesis. | Characterized by stretchy, fragile skin, easy bruising, and significant joint hypermobility. The severity of symptoms can vary greatly. |
| Hypermobile EDS (hEDS) | Joint hypermobility, often presenting with a range of symptoms, including chronic pain, fatigue, and autonomic dysfunction. Individuals with hEDS may experience frequent dislocations, headaches, and gastrointestinal issues. | Mutations in genes responsible for collagen production or related connective tissue components are often not identified, indicating a complex genetic basis that is still being researched. This lack of a specific genetic marker underscores the difficulty in diagnosing this particular type. | While joint hypermobility is a hallmark, the broader spectrum of symptoms, including chronic pain, fatigue, and autonomic dysfunction, distinguishes this type. |
| Vascular EDS | Fragile blood vessels, easy bruising, skin fragility, and potential for life-threatening complications like aneurysms and arterial tears. Individuals may experience unusual bleeding or bruising. | Mutations in the COL3A1 gene, which is responsible for collagen type III production. | Characterized by a heightened risk of blood vessel abnormalities, requiring careful monitoring and management to prevent life-threatening complications. |
| Kyphoscoliosis type | Kyphoscoliosis (abnormal curvature of the spine), joint hypermobility, and skin fragility. This type is often associated with other connective tissue disorders. | Mutations in genes involved in collagen synthesis or related processes. A precise genetic basis may not be identified in all cases. | Kyphoscoliosis is a defining feature, along with the common symptoms of joint hypermobility and skin fragility. |
Symptoms and Diagnosis
Understanding Ehlers-Danlos Syndrome (EDS) involves recognizing the wide range of symptoms and the often-complex diagnostic process. This isn’t a one-size-fits-all condition; the presentation varies significantly between individuals and even within families. Accurate diagnosis hinges on careful consideration of symptoms, a thorough medical history, and often, a multidisciplinary approach.
Common Symptoms
EDS manifests in a variety of ways, affecting multiple body systems. Recognizing these diverse symptoms is crucial for early diagnosis and appropriate management. The symptoms can range from mild to severe, impacting daily life in varying degrees.
- Musculoskeletal System: Joint hypermobility, characterized by excessive movement and range of motion in the joints, is a hallmark of many EDS types. This can lead to frequent dislocations, subluxations, and pain. Muscle weakness and fatigue are also common, sometimes contributing to difficulty with physical activities. Individuals may experience chronic pain, often described as aching or throbbing, and sometimes associated with trigger points or myofascial restrictions.
- Skin: Skin fragility is another defining feature of EDS. The skin may be unusually stretchy, and easily bruised or damaged. This can range from a mild tendency towards bruising to significant skin fragility, making even minor trauma lead to significant injuries. Individuals may also experience skin laxity, with loose or redundant skin folds.
- Gastrointestinal System: Digestive issues are frequently reported in individuals with EDS. These may include problems with motility (movement of food through the digestive tract), leading to bloating, constipation, or diarrhea. Chronic pain and inflammation within the gastrointestinal tract can also contribute to discomfort and digestive challenges.
- Cardiovascular System: Some types of EDS can affect the cardiovascular system, leading to conditions like aortic aneurysms or other vascular issues. The severity of these complications varies widely. Individuals with EDS may require ongoing monitoring of cardiovascular health.
- Neurological System: Neurological symptoms, such as headaches, dizziness, and balance problems, can be present in some individuals with EDS. These can stem from the interplay of joint hypermobility, pain, and potential autonomic nervous system dysfunction.
Diagnostic Criteria and Procedures
Diagnosing EDS requires a careful evaluation of the individual’s medical history, physical examination, and sometimes, genetic testing. There’s no single test for EDS, making a thorough assessment critical.
- Medical History: A comprehensive medical history, including details about family history of connective tissue disorders, personal symptoms, and past injuries, is essential. The history should include details about the onset and progression of symptoms, including the severity and frequency.
- Physical Examination: A physical examination focuses on assessing joint hypermobility, skin characteristics, and other relevant features. The examination may include range-of-motion assessments and evaluation of skin elasticity and fragility.
- Genetic Testing: In some cases, genetic testing can confirm a diagnosis of a specific type of EDS. This is especially useful when the clinical presentation is suggestive of a particular subtype or when family history strongly suggests a genetic link. Genetic testing is not always necessary and may not always be conclusive. The information from genetic testing should be interpreted within the context of the individual’s medical history and physical examination findings.
Importance of a Multidisciplinary Approach
Given the multifaceted nature of EDS, a multidisciplinary approach is often necessary for optimal diagnosis and management. This involves collaboration among various healthcare professionals.
- Collaboration with specialists: Collaboration between rheumatologists, geneticists, pain management specialists, physical therapists, and other healthcare professionals can provide a more comprehensive understanding of the individual’s needs and provide the most effective treatment plan. The expertise of multiple specialists is crucial in navigating the complexities of EDS.
Symptom Severity Table
| Symptom | Body System | Description | Severity Level |
|---|---|---|---|
| Joint Hypermobility | Musculoskeletal | Excessive range of motion in joints | Mild, Moderate, Severe |
| Skin Bruising | Skin | Easy bruising, tendency to bleed easily | Mild, Moderate, Severe |
| Gastrointestinal Issues | Gastrointestinal | Constipation, diarrhea, bloating | Mild, Moderate, Severe |
| Fatigue | Musculoskeletal | Chronic tiredness, lack of energy | Mild, Moderate, Severe |
Misdiagnosis Scenarios and Early Diagnosis
Misdiagnosis is unfortunately a concern in EDS cases, often due to the overlap of symptoms with other conditions. Early diagnosis is crucial for timely interventions and improved quality of life.
- Common Misdiagnoses: Conditions such as fibromyalgia, chronic fatigue syndrome, or other musculoskeletal disorders can be misdiagnosed in individuals with EDS. The presence of overlapping symptoms can make accurate diagnosis challenging.
- Importance of Early Diagnosis: Early diagnosis allows for prompt implementation of appropriate management strategies, including physical therapy, pain management, and potentially, genetic counseling. This leads to better outcomes in terms of long-term health and quality of life.
Impact on Daily Life: Ehlers Danlos Syndrome Overview
Living with Ehlers-Danlos Syndrome (EDS) significantly impacts daily life, requiring adjustments and accommodations across various aspects. The unpredictable nature of symptoms, from joint pain and hypermobility to fatigue and digestive issues, can create substantial challenges in managing everyday tasks and maintaining a fulfilling lifestyle. This section explores the multifaceted impact of EDS on daily activities, personal relationships, and overall well-being.
Challenges in Daily Activities
The chronic pain, fatigue, and physical limitations associated with EDS can make seemingly simple tasks feel overwhelming. Individuals may experience difficulty with basic movements like walking, standing, or even dressing themselves. This often leads to a reduction in physical activity, impacting overall health and potentially contributing to further complications. Maintaining personal hygiene, preparing meals, and performing household chores can also be demanding and require significant planning and support.
The unpredictable nature of symptoms necessitates flexibility and adaptability in daily routines, and often necessitates frequent breaks and rest periods.
Educational and Employment Challenges
EDS can present significant obstacles in both education and employment settings. Students may experience difficulties attending classes regularly, concentrating in lectures, and completing assignments due to pain, fatigue, and the need for frequent medical appointments. Similarly, individuals in the workforce may face challenges maintaining consistent employment due to unpredictable absences, reduced productivity, and the need for flexible work arrangements.
Finding accommodations that balance the demands of work or study with the needs of EDS is crucial for maintaining a sense of normalcy and independence. Examples of accommodations include flexible work hours, modified work tasks, and accessible work environments.
Social Interactions and Relationships
Maintaining social connections and relationships can be challenging for individuals with EDS. Fatigue, pain, and the need for frequent rest can limit social activities and make it difficult to participate in social gatherings or maintain close friendships. Understanding and acceptance from friends and family are crucial for managing the emotional and social aspects of living with EDS. Building a support system of understanding individuals and creating a safe and supportive social environment is vital.
Psychological and Emotional Impact
Living with a chronic illness like EDS can have a profound psychological and emotional toll. The unpredictability of symptoms, the limitations on physical activity, and the challenges in managing daily tasks can lead to feelings of frustration, anxiety, and depression. Experiencing pain, fatigue, and reduced physical ability can impact self-esteem and body image. The emotional burden of managing the condition can create stress and strain on personal relationships.
Seeking professional support from therapists or counselors can provide valuable coping mechanisms and strategies to manage emotional well-being.
Coping Strategies and Support Systems
Developing effective coping strategies is essential for managing the challenges of EDS. These strategies may include time management techniques, stress reduction methods, and strategies for pain management. Creating a supportive network of family, friends, and healthcare professionals is crucial for navigating the complexities of the condition. Utilizing support groups and online communities provides valuable avenues for connection and shared experiences.
Seeking professional guidance from therapists and counselors can help individuals develop coping mechanisms and strategies for managing emotional well-being.
Examples of Accommodations and Support Systems
Numerous accommodations and support systems are available to individuals with EDS. These may include assistive devices, modified work environments, and flexible educational plans. Support groups, online forums, and advocacy organizations can provide valuable resources and a sense of community. Financial assistance programs and disability benefits can provide financial support to individuals and families managing EDS. Understanding and implementing these supports can significantly improve the quality of life for those living with EDS.
Treatment and Management
Managing Ehlers-Danlos Syndrome (EDS) is a multifaceted process focusing on symptom relief and improving quality of life. A personalized approach is crucial, as EDS presents differently in each individual. Treatment often involves a combination of therapies, medications, and lifestyle adjustments. Holistic care acknowledges the interconnectedness of physical, emotional, and social well-being, creating a comprehensive strategy for managing the challenges associated with EDS.Effective management of EDS requires a strong partnership between the patient, healthcare providers, and support networks.
Understanding the unique needs of each individual with EDS and tailoring interventions to address those needs is paramount. A proactive and ongoing approach to treatment and management is vital to maximizing functional capacity and overall well-being.
Current Treatment Options
Current EDS treatments focus on managing symptoms rather than curing the underlying condition. This includes a wide range of strategies, such as physical therapy, occupational therapy, and medication. Regular medical checkups and monitoring are essential for early detection and management of potential complications.
Physical Therapy
Physical therapy plays a vital role in managing EDS. It helps improve joint stability, muscle strength, and flexibility, thereby reducing pain and improving mobility. Specific exercises and techniques, tailored to the individual’s needs, can enhance functional capacity and prevent further joint damage. A physical therapist can develop a personalized exercise program that addresses specific needs, such as strengthening weakened muscles or improving range of motion.
Occupational Therapy, Ehlers danlos syndrome overview
Occupational therapy focuses on adapting daily activities and environments to accommodate the limitations imposed by EDS. This may involve modifications to workspaces, home environments, or daily routines. Occupational therapists can also provide strategies for managing pain and fatigue, and teach coping mechanisms for everyday tasks. This can include assistive devices, ergonomic adjustments, and adaptive techniques for various activities.
Medications and Supplements
Several medications and supplements may help manage specific EDS symptoms. Pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and certain types of analgesics, can provide temporary relief from pain. Medications for anxiety or depression may be helpful if these conditions are present. While supplements may offer potential benefits, consulting with a doctor before taking any supplements is essential to avoid interactions with other medications or potential adverse effects.
Importance of Regular Medical Checkups and Monitoring
Regular medical checkups and monitoring are critical for individuals with EDS. This allows for early detection and management of potential complications, such as joint dislocations, cardiovascular issues, or digestive problems. Early intervention can significantly improve outcomes and prevent more severe conditions. Monitoring progress and adjusting treatment plans as needed is vital for managing the fluctuating nature of EDS symptoms.
Step-by-Step Guide for Managing Pain and Discomfort
Managing pain and discomfort related to EDS requires a structured approach. This involves recognizing triggers, developing coping mechanisms, and seeking support.
Understanding Ehlers-Danlos Syndrome (EDS) involves recognizing the diverse range of symptoms, from hypermobile joints to stretchy skin. Proper crutch positioning and sizing is crucial for managing EDS-related mobility limitations. Learning about the correct techniques for crutch usage can significantly improve daily function and prevent further injury. For detailed guidance on crutch positioning and sizing, check out this helpful resource: crutch positioning and sizing.
Ultimately, a holistic approach to managing EDS requires considering various support strategies, like correctly fitting crutches, for optimal well-being.
- Identify Pain Triggers: Keep a pain journal to note activities, foods, environmental factors, or other potential triggers that exacerbate pain. This helps to identify patterns and develop strategies to avoid or mitigate these triggers.
- Develop Coping Mechanisms: Learn relaxation techniques such as deep breathing exercises, mindfulness, or progressive muscle relaxation. These can help manage pain and stress. Consider incorporating stress-reducing activities, such as yoga, meditation, or spending time in nature. This is vital in controlling pain.
- Seek Support: Connect with support groups or online communities for individuals with EDS. Sharing experiences and coping strategies with others facing similar challenges can provide invaluable emotional support. Support networks are important for both emotional and practical support.
- Communicate with Healthcare Providers: Regularly communicate with healthcare providers about pain levels, medication effectiveness, and any changes in symptoms. This ensures that the treatment plan remains effective and addresses evolving needs.
Research and Future Directions
Unraveling the complexities of Ehlers-Danlos Syndrome (EDS) requires ongoing research to understand its diverse presentations, develop effective treatments, and ultimately improve the lives of those affected. Current research efforts are multifaceted, exploring genetic factors, physiological mechanisms, and potential therapeutic avenues. This exploration into the future of EDS management promises innovative solutions and a better understanding of this challenging condition.The quest for breakthroughs in EDS treatment is fueled by the dedication of researchers, clinicians, and patient advocates.
Ehlers-Danlos syndrome (EDS) is a fascinating but complex group of inherited connective tissue disorders. It often impacts multiple body systems, which can make managing symptoms challenging. Learning about new treatments like new high blood pressure drug tryvio for other conditions, like hypertension, is crucial for understanding how different medical advancements might affect overall well-being, even when addressing a seemingly unrelated health issue.
Ultimately, a holistic approach to managing EDS, incorporating the latest research and treatment options, is key.
A deep dive into the existing research landscape and potential future directions is crucial to inform and guide the pursuit of effective therapies. This knowledge can also facilitate personalized approaches to managing the symptoms and improving the overall quality of life for individuals with EDS.
Current Research Efforts
Research into EDS encompasses a broad range of approaches, including genetic studies to identify specific gene mutations associated with different EDS subtypes, and physiological investigations into the underlying mechanisms of connective tissue dysfunction. These efforts aim to enhance our understanding of the specific pathways affected in EDS and how these dysfunctions manifest as diverse symptoms. Further studies are examining the impact of environmental factors and lifestyle choices on symptom presentation and disease progression.
Potential New Treatments and Therapies
Several promising avenues for new treatments and therapies are being explored. These include targeted therapies that aim to address specific genetic defects or physiological imbalances, potentially ameliorating symptoms and improving overall health. For example, research is focusing on potential therapies that could mitigate joint pain, promote tissue repair, or improve autonomic nervous system regulation. Personalized medicine approaches tailored to individual genetic profiles and symptom presentations hold significant promise.
Clinicians are also exploring the use of non-pharmacological therapies like physical therapy and occupational therapy, tailored to each patient’s specific needs.
Areas Where More Research Is Needed
Despite significant progress, critical areas require further investigation. Developing standardized diagnostic criteria for various EDS subtypes is still a priority. Improving diagnostic tools, including genetic testing and non-invasive imaging techniques, is essential for timely and accurate diagnoses. Understanding the long-term effects of EDS on different organ systems is another crucial area. This includes better understanding of cardiovascular and neurological implications.
Additionally, research into the impact of psychological factors on the experience of EDS is needed, enabling comprehensive management strategies.
Importance of Patient Advocacy and Participation in Research
Patient advocacy plays a critical role in advancing research efforts and ensuring that research aligns with the needs of the EDS community. Direct input from individuals with EDS is essential in shaping research priorities, methodologies, and outcome measures. Participation in clinical trials and research studies is vital to gathering data, understanding disease progression, and evaluating the efficacy of new treatments.
This active engagement of the patient community is critical to accelerate the translation of research findings into tangible improvements in care and outcomes.
Potential Breakthroughs in Understanding and Treating EDS
Future breakthroughs in understanding and treating EDS could include the development of disease-modifying therapies. These therapies, if successful, could potentially slow or halt the progression of the disease, minimizing the long-term impact on affected individuals. The development of new diagnostic tools could lead to earlier and more accurate diagnoses, enabling timely interventions and better management strategies. The combination of these advancements, supported by continued research and patient engagement, holds the potential to reshape the future of EDS care and create a more hopeful outlook for individuals living with this complex condition.
Living with Ehlers-Danlos Syndrome
Navigating life with Ehlers-Danlos Syndrome (EDS) is a unique journey, filled with both challenges and triumphs. Living with EDS requires a multifaceted approach to managing symptoms, maintaining a positive outlook, and fostering a strong support system. Understanding the complexities of the condition and developing effective coping strategies are key to achieving a high quality of life.Individuals with EDS face a range of physical and emotional challenges.
These can include chronic pain, fatigue, joint instability, and limited mobility. Furthermore, the unpredictable nature of EDS symptoms can lead to anxiety and frustration. However, with the right resources and support, individuals with EDS can lead fulfilling lives.
Building a Supportive Network
A strong support network is crucial for individuals living with EDS. It provides emotional comfort, practical assistance, and shared experiences that can significantly impact well-being. The journey with EDS is often better navigated when surrounded by understanding individuals who can provide encouragement and practical support.
Role of Family, Friends, and Support Groups
Family and friends play a vital role in supporting individuals with EDS. Their understanding, patience, and willingness to learn about the condition are essential. Support groups offer a unique platform for connecting with others who understand the daily struggles and triumphs of living with EDS. Sharing experiences, finding solutions, and receiving encouragement from peers who understand the unique challenges is a vital part of the process.
This can be particularly helpful in addressing the emotional impact of the condition.
Communicating with Healthcare Professionals
Effective communication with healthcare professionals is paramount. Individuals with EDS should clearly articulate their symptoms, concerns, and treatment goals. Maintaining detailed records of symptoms, treatments, and responses is beneficial. This detailed information aids in diagnosis, treatment planning, and adjustments to therapies. Open communication facilitates a collaborative relationship between the patient and their healthcare team, ensuring optimal management of the condition.
Clear and concise communication helps to avoid misunderstandings and ensure that healthcare professionals fully understand the individual’s needs.
Self-Advocacy for Individuals with EDS
Self-advocacy is essential for individuals with EDS. This involves actively participating in their healthcare decisions, understanding their condition, and expressing their needs and preferences. Learning about EDS and related therapies empowers individuals to make informed choices about their care. Educating others about EDS is a vital part of self-advocacy. It helps to foster understanding and create a more supportive environment.
Maintaining a Positive Outlook and Quality of Life
Despite the challenges, maintaining a positive outlook is essential for individuals with EDS. This can involve setting realistic goals, celebrating small victories, and focusing on personal strengths. Finding healthy coping mechanisms, such as engaging in hobbies, connecting with nature, or pursuing creative outlets, can be beneficial. Establishing routines that support physical and emotional well-being can significantly enhance quality of life.
Prioritizing self-care, including adequate rest, nutrition, and social connections, can help to manage symptoms and maintain a positive perspective.
Wrap-Up
In conclusion, Ehlers-Danlos syndrome overview reveals a complex tapestry of challenges and adaptations. While diagnosis can be challenging, early intervention and supportive care are crucial for improving quality of life. The ongoing research into EDS offers hope for future advancements in treatment and understanding, making it vital to stay informed about this condition. Ultimately, fostering a supportive environment for individuals with EDS is paramount to their well-being.