Reverse walking in physical therapy is a powerful technique gaining traction for improving balance, gait, and strength. This approach challenges the typical forward motion, offering unique benefits for various patient populations. We’ll explore the biomechanics, benefits, and safety considerations, along with exercise progressions and modifications.
This comprehensive guide dives into the specifics of reverse walking, outlining its application in various physical therapy settings. We’ll discuss how this exercise impacts muscle activation, balance, and overall functional improvement, alongside the important factors of safety and assessment.
Introduction to Reverse Walking in Physical Therapy

Reverse walking, a seemingly simple activity, plays a crucial role in physical therapy. It’s not just about walking backward; it’s a carefully structured exercise that targets specific muscle groups, improves balance, and aids in the rehabilitation process for a variety of conditions. This exercise is often used in conjunction with other therapies to help patients regain lost function and mobility.Reverse walking in physical therapy is a controlled exercise, meticulously designed to challenge and strengthen specific muscle groups, often in a way that forward walking does not.
By reversing the movement pattern, therapists can focus on different muscle activation patterns and address specific functional deficits. This controlled environment allows for personalized adjustments and close monitoring, making it a valuable tool in rehabilitation programs.
Definition of Reverse Walking
Reverse walking is the act of walking backward. It’s a deliberate movement pattern, not simply a reversal of forward walking. The specific technique and control involved make it a distinct exercise with different therapeutic applications.
Purpose of Reverse Walking in Physical Therapy
Reverse walking exercises in physical therapy are used to enhance balance, coordination, and strength. By requiring the body to engage different muscle groups and adapt to a novel movement pattern, it helps improve proprioception (the body’s awareness of its position in space) and reaction time. The controlled environment allows therapists to assess and modify the exercise to suit individual needs and goals.
Reverse walking in physical therapy can be a surprisingly effective technique for improving balance and gait. It’s a great way to build strength and coordination, but sometimes it’s tough to explain to someone why it’s necessary. Just like when explaining skin conditions like vitiligo to others, explaining vitiligo to others requires patience and clear communication. Ultimately, though, understanding the process behind reverse walking, like understanding the specifics of any physical therapy, helps patients focus on the positive outcomes.
It’s all about a tailored approach to healing.
Common Conditions Where Reverse Walking is Used
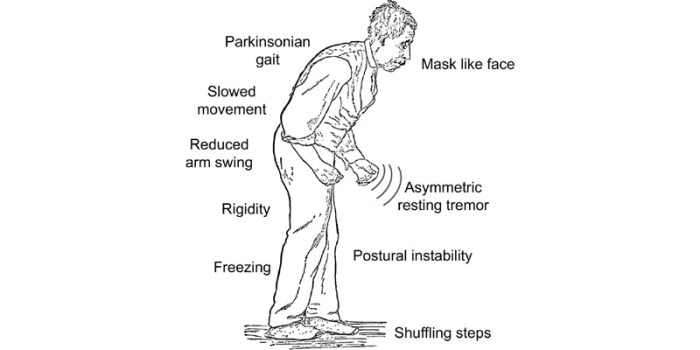
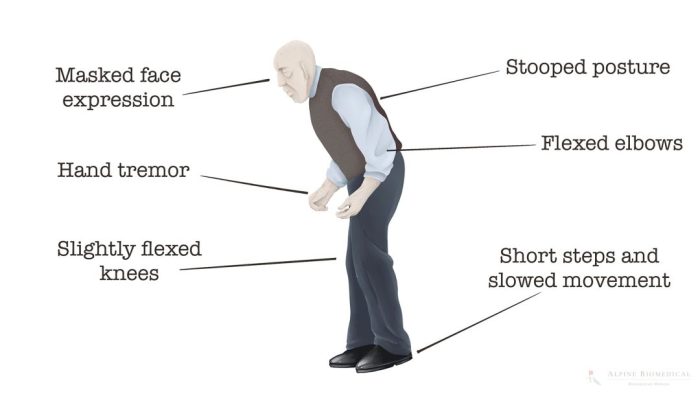
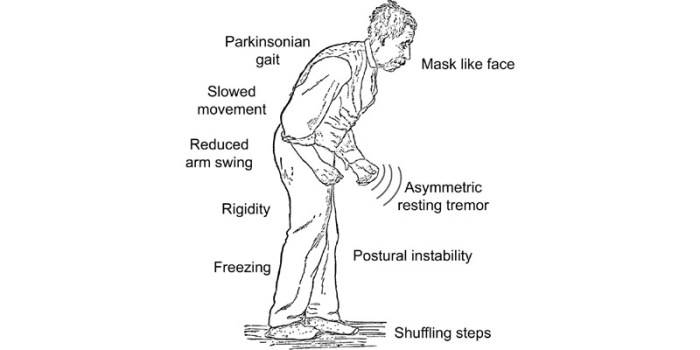
Reverse walking is often incorporated into rehabilitation programs for various conditions affecting balance, coordination, and lower body strength. These conditions include stroke, traumatic brain injury, multiple sclerosis, and neurological disorders that affect motor function. It’s also utilized for improving gait patterns after surgery or injury.
Stages of Reverse Walking Exercises
| Stage | Description | Key Movements | Therapeutic Benefits |
|---|---|---|---|
| Stage 1: Basic Reverse Steps | Initial phase focusing on establishing the proper backward gait pattern. | Maintaining a controlled and slow pace, ensuring proper posture and alignment. Small, deliberate steps with minimal arm swing. | Improves proprioception and balance. Builds foundational strength and stability in the lower extremities. |
| Stage 2: Controlled Reverse Walking | Progressing to longer strides and increasing the speed while maintaining stability. | Increasing step length and pace, while maintaining upright posture and balance. Gradual increase in arm swing (controlled). | Develops more advanced balance and coordination skills. Enhances endurance and strengthens postural muscles. |
| Stage 3: Advanced Reverse Walking | Incorporating turns and changes in direction to enhance agility. | Including turns, pivots, and changes in direction within the backward walking pattern. Maintaining speed and balance. | Improves agility, responsiveness, and dynamic balance. Develops neuromuscular control and reaction time. |
| Stage 4: Functional Reverse Walking | Integrating reverse walking into everyday tasks or activities. | Reverse walking in real-world scenarios such as navigating obstacles, stair climbing, or carrying objects. | Improves functional mobility, confidence, and independence. Translates therapy gains into everyday activities. |
Biomechanics of Reverse Walking
Reverse walking, a seemingly simple act, presents unique biomechanical challenges compared to forward walking. Understanding these differences is crucial for physical therapists working with patients recovering from injuries or neurological conditions. The altered loading patterns and muscle activation strategies demand a nuanced approach to rehabilitation.Reverse walking requires a significant reorganization of the body’s movement patterns. The interplay between muscle activation, joint angles, and ground reaction forces differs substantially from the established biomechanics of forward walking.
This necessitates a deeper understanding of the specific adaptations needed for effective reverse walking rehabilitation.
Comparison of Forward and Reverse Walking
Forward and reverse walking, while both utilizing gait cycles, exhibit fundamental differences in their biomechanical characteristics. The direction of progression significantly alters the distribution of forces and the recruitment of muscles. In forward walking, the body propels itself forward, relying on a specific sequence of muscle contractions. Reverse walking, conversely, necessitates a reversal of these forces and movements, demanding a distinct set of muscular actions to move the body backward.
Muscle Activation During Reverse Walking
The muscle activation patterns in reverse walking are distinct from those in forward walking. Muscles primarily responsible for forward propulsion, such as the gluteus maximus and hamstrings, experience altered roles and activation timings in reverse walking. Instead of pushing the body forward, these muscles now work to counteract the tendency to fall backward. Furthermore, muscles responsible for stabilizing the body, such as the core muscles and hip abductors, become even more crucial in reverse walking to maintain balance and control.
Muscle Activation Patterns
| Muscle Group | Forward Walking Activation | Reverse Walking Activation |
|---|---|---|
| Gluteus Maximus | Primary extensor of the hip, propelling the body forward | Significant activation to stabilize and counteract backward movement; may also be less prominent compared to forward walking |
| Hamstrings | Assist in hip extension and knee flexion during the swing phase | Assist in maintaining balance and controlling the backward movement of the leg, may experience higher activation in the early swing phase to compensate for the opposite movement. |
| Quadriceps Femoris | Primary extensor of the knee, crucial for maintaining forward momentum. | Less prominent compared to forward walking; primarily involved in controlling knee extension to maintain balance. |
| Gastrocnemius | Assists in plantarflexion, maintaining stability and propelling the body forward | Important for maintaining balance during the backward movement; plantarflexion occurs during the stance phase but is modified to stabilize against the backward movement. |
| Tibialis Anterior | Assists in dorsiflexion, contributing to a smooth stride and forward progression. | Crucial for controlling ankle movement to maintain stability during the backward movement. |
| Core Muscles | Crucial for trunk stability and maintaining posture during the entire gait cycle | Even more crucial for maintaining balance and posture; increased activation during the backward movement to counteract the tendency to lean forward. |
Benefits and Applications
Reverse walking, a seemingly simple exercise, holds significant potential for rehabilitation and improving overall physical function. It offers a unique challenge to the body, promoting balance, strength, and coordination in a controlled environment. This approach can be especially beneficial for patients recovering from injuries or conditions that affect their gait.The exercise’s effectiveness lies in its ability to engage multiple muscle groups, promoting functional strength and balance, crucial for everyday activities.
Furthermore, the controlled nature of reverse walking allows therapists to adapt the exercise to suit the specific needs and abilities of individual patients.
Benefits of Reverse Walking Exercises
Reverse walking provides a multifaceted approach to rehabilitation. It actively challenges the body’s balance mechanisms and strengthens crucial muscle groups, thereby improving stability and gait. The emphasis on controlled movement reduces the risk of falls and injuries, allowing patients to progress safely and effectively. Patients often experience a noticeable improvement in their confidence and ability to perform everyday tasks.
Role in Improving Balance and Gait
Reverse walking directly impacts balance and gait by requiring the body to compensate for the atypical movement pattern. This process enhances proprioception, the body’s awareness of its position in space. By practicing reverse walking, patients refine their strategies for maintaining balance, which can translate to improvements in their overall gait pattern during forward walking. Consistent practice strengthens the neural pathways responsible for coordinated movement.
Role in Strengthening Specific Muscle Groups
Reverse walking targets a wide array of muscle groups, contributing to overall functional strength. The exercise particularly strengthens muscles in the legs, core, and back, improving stability and reducing the risk of falls. This increased strength also enhances the ability to perform daily activities such as climbing stairs or rising from a chair. By working against gravity in an atypical manner, reverse walking strengthens postural muscles and deep core stabilisers.
Patient Populations Who Could Benefit
Reverse walking can be beneficial for a variety of patient populations, including individuals recovering from stroke, neurological conditions, or orthopedic injuries. The controlled environment of a therapy session allows for gradual progression and tailoring of the exercise to meet the individual’s specific needs. It can also be a valuable tool for older adults to maintain or improve their balance and mobility.
Reverse walking in physical therapy can be a surprisingly effective exercise, but it’s crucial to manage any pain that comes with it. Sometimes, you might need ibuprofen to ease the discomfort, but it’s essential to understand how much is too much. Knowing the safe dosage is key to avoiding potential side effects, and you can find helpful information on that front at how much ibuprofen is too much.
Remember to listen to your body and adjust your reverse walking routine accordingly, prioritizing pain management and recovery for optimal results.
Moreover, patients with cerebral palsy, multiple sclerosis, or Parkinson’s disease could benefit from reverse walking, given careful consideration and adaptation to their individual conditions.
Adapting Reverse Walking for Different Levels of Ability
The exercise’s versatility allows for adaptations to accommodate different levels of ability. Patients with limited mobility can begin with shorter distances or reduced speed, while those with greater capacity can gradually increase the intensity and duration of their training. The environment, support, and guidance provided by a physical therapist are crucial for a safe and effective progression. Furthermore, patients can use assistive devices, such as walkers or canes, to maintain stability and safety during reverse walking.
Potential Adaptations for Different Patient Needs
- Reduced Speed and Distance: Starting with short distances and slow speeds allows patients to gradually acclimate to the exercise without overwhelming them. This is particularly important for patients with limited mobility or balance issues.
- Assisted Walking: Using handrails, walkers, or other assistive devices can help maintain balance and safety, especially for patients with significant balance deficits. The level of assistance should be adjusted as the patient progresses.
- Varying Terrain: Practicing reverse walking on different surfaces, such as flat ground, inclines, or declines, can progressively challenge balance and coordination. The level of difficulty should be adjusted based on the patient’s capabilities.
- Resistance Training: Incorporating resistance bands or weights can enhance the strengthening effect of reverse walking, increasing the challenge and promoting functional strength for specific muscle groups.
- Focus on Balance: During reverse walking, focusing on maintaining balance and control is essential. Visual cues, such as stationary points, can be used to help patients maintain their balance, as well as improve proprioception.
Exercise Progressions and Modifications
Reverse walking, while beneficial, requires a structured approach to ensure safety and effectiveness. Progression should be tailored to each patient’s individual needs and abilities, building upon previous successes and accommodating limitations. This careful gradation minimizes risk of injury and maximizes therapeutic gains.
Exercise Progression Stages
Gradual progression is crucial in reverse walking exercises. Starting with simple movements and progressively increasing the complexity ensures patients build strength and confidence before tackling more challenging tasks. This approach allows for optimal adaptation and prevents frustration or discouragement.
| Stage | Description | Equipment | Therapeutic Goals |
|---|---|---|---|
| Stage 1: Initiation | Short, controlled steps backward, maintaining a stable stance. Focus on maintaining balance and proper posture. | None initially, but potentially a wall or railing for support. | Develop balance and proprioception in the reverse direction. Establish a safe starting point for the exercise. |
| Stage 2: Controlled Movement | Increasing the distance of reverse walking steps, maintaining a steady pace. Maintaining a neutral spine and avoiding excessive hip flexion or extension is important. | Potentially light ankle weights. | Enhance motor control and coordination in reverse walking. Improve strength and endurance in posterior chain muscles. |
| Stage 3: Increased Pace | Increasing the speed of reverse walking while maintaining proper form. Gradual increase in speed is essential to prevent falls or injuries. | None, or resistance bands for increased challenge. | Improve cardiovascular fitness and endurance. Develop dynamic balance and coordination. |
| Stage 4: Advanced Challenges | Adding variations such as reverse walking with arm movements, or stepping over obstacles. | Resistance bands, balance pads, cones for obstacles. | Increase functional capacity. Develop more complex motor patterns for functional activities. |
Modifications for Specific Impairments
Modifications are essential for accommodating patients with diverse impairments, ensuring they can safely participate in reverse walking exercises. Adapting the exercise ensures effectiveness while mitigating risk.
| Impairment | Modification | Explanation |
|---|---|---|
| Balance Issues | Perform reverse walking near a wall or support surface for added stability. Begin with shorter distances and gradually increase the steps. | Providing a stable environment reduces the risk of falls and allows the patient to focus on proper form. |
| Knee Pain | Use a cane or walker for support during reverse walking. Consider using a knee brace for added stability. | Minimizing stress on the knee joint through support structures. |
| Hip Weakness | Use resistance bands around the knees or ankles to increase the resistance and strengthen the hip muscles. Perform reverse walking with a slight bend in the knees to reduce the strain on the hips. | Utilizing resistance increases the challenge while focusing on hip strengthening and proper form. |
| Foot Drop | Use a foot drop brace to maintain proper foot position. Ensure the patient has appropriate footwear for support and stability. | Maintaining a functional foot position is critical to maintaining balance and avoiding falls. |
| Reduced Range of Motion | Use assistive devices to support the affected limb. Modify the exercise to avoid positions that exacerbate pain or stiffness. | Avoiding exacerbating the impairment is paramount for effective therapy. |
Safety Considerations and Precautions
Reverse walking, while beneficial for rehabilitation, necessitates careful consideration of safety protocols. Implementing these precautions minimizes the risk of injury and maximizes the effectiveness of the exercise program. A thorough understanding of potential risks and proactive strategies for prevention are crucial for both therapists and patients.Proper supervision and meticulous patient assessment are paramount to successful reverse walking. An individualized approach, tailored to the patient’s specific needs and limitations, is essential for optimizing safety and progress.
Importance of Proper Supervision
Thorough supervision is crucial to ensure patient safety and prevent potential injuries during reverse walking exercises. Qualified physical therapists or trained professionals should closely monitor patients, adjusting the exercise program as needed. Constant observation allows for immediate intervention in case of balance issues, pain, or discomfort. This ensures that the patient remains within their capabilities and avoids overexertion.
Patient Assessment and Evaluation
Pre-exercise assessments are vital for identifying potential risks and tailoring the reverse walking program. A comprehensive evaluation should include a thorough medical history, gait analysis, range of motion assessment, strength testing, and balance evaluations. These assessments help determine the patient’s baseline capabilities, identify any pre-existing conditions, and establish appropriate exercise progressions. Identifying and addressing potential issues like joint instability, muscle weakness, or balance problems proactively reduces the risk of injuries.
Potential Risks and Complications
Reverse walking, while generally safe, carries potential risks. These include falls, muscle strains, joint pain, and exacerbation of pre-existing conditions. Patients with conditions like osteoporosis, arthritis, or recent injuries are at a higher risk. A careful evaluation and gradual progression are crucial to mitigate these risks. For example, a patient with knee osteoarthritis might experience increased pain if the reverse walking exercises are too vigorous.
Preventing Common Injuries
Preventing injuries during reverse walking exercises involves several strategies. First, ensuring appropriate footwear is essential for proper support and balance. Secondly, ensuring the exercise environment is safe and free of obstacles is vital. Thirdly, a gradual increase in intensity and duration is recommended. This gradual progression allows the body to adapt to the new movement pattern and reduces the risk of overuse injuries.
Mitigation Strategies, Reverse walking in physical therapy
Several strategies can mitigate risks associated with reverse walking. Using assistive devices, such as canes or walkers, can provide additional support and stability. Modifying the exercise environment, like reducing the surface area, can decrease the risk of falls. Implementing proper warm-up and cool-down routines is essential to prepare the muscles and joints for the exercise and prevent muscle soreness.
Communication is key, encouraging patients to report any pain or discomfort promptly allows for immediate intervention.
Reverse walking in physical therapy can be a surprisingly effective exercise, especially for those with specific mobility challenges. While focusing on proper form is key, sometimes underlying health conditions can impact progress. For example, if you’re experiencing hypothyroidism, exploring options like using armour thyroid for hypothyroidism might be beneficial alongside your physical therapy routine. Ultimately, reverse walking, when approached thoughtfully, can lead to improved balance and overall physical well-being.
Assessment and Evaluation
Reverse walking, while beneficial, requires careful assessment to ensure patient safety and optimal progress. A thorough evaluation helps determine the appropriate exercise intensity, modifications, and overall program design for each individual. This process allows for personalized treatment plans, maximizing outcomes and minimizing risks.Understanding a patient’s readiness for reverse walking is crucial for successful rehabilitation. This involves evaluating various factors, from their physical capabilities to their cognitive understanding of the exercise.
A structured approach, combining objective measurements and subjective feedback, ensures a safe and effective rehabilitation journey.
Patient Readiness Assessment
A comprehensive assessment prior to introducing reverse walking exercises is paramount. This assessment should not be a cursory check but a detailed evaluation of the patient’s current physical and cognitive state. This will determine their suitability for the exercise, identifying any potential limitations or risks.
- Medical History Review: A detailed review of the patient’s medical history is essential. This includes any pre-existing conditions, recent surgeries, medications, and any known allergies. This ensures that reverse walking is appropriate and does not exacerbate underlying health issues. For example, a patient with a history of heart conditions might require closer monitoring during the exercise.
- Range of Motion Assessment: Assessing the patient’s range of motion (ROM) in the hips, knees, ankles, and spine is crucial. Limited ROM in any joint can significantly impact the ability to perform reverse walking. A thorough examination of the patient’s flexibility in these areas is important for successful exercise execution.
- Balance and Gait Analysis: Evaluating the patient’s balance and gait is fundamental. This involves observing their posture, stance, and walking pattern in a variety of settings, including flat surfaces and potentially uneven terrain. Identifying existing gait abnormalities, such as a tendency to lean, can be addressed through exercise progressions.
- Strength Assessment: Evaluating the patient’s lower extremity strength is vital. This includes assessing the strength of muscles involved in propulsion and balance during walking. A strength deficit in the lower limbs may necessitate modifications or a slower progression.
- Cognitive Functioning Evaluation: Assessing the patient’s cognitive ability to understand and follow instructions is critical. Clear communication and proper instruction are essential for patient compliance and safety during exercise.
Patient Assessment Checklist
A standardized checklist aids in ensuring a thorough assessment. This provides structure and helps track key data points for each patient.
| Assessment Item | Criteria | Evaluation |
|---|---|---|
| Medical History | Any pre-existing conditions, recent surgeries, medications, allergies | Reviewed and documented |
| Range of Motion (ROM) | Hip, knee, ankle, spine | Measured and recorded |
| Balance | Posture, stance, walking pattern on various surfaces | Observed and documented |
| Strength | Lower extremity muscles (e.g., quadriceps, hamstrings, glutes) | Evaluated using standardized tests (e.g., manual muscle testing) |
| Cognitive Function | Understanding instructions, following commands | Observed and documented |
Progress Evaluation Metrics
Tracking progress is crucial for adapting the exercise program and motivating the patient. Monitoring key metrics provides evidence of improvement.
- Gait Speed and Distance: Measuring the patient’s walking speed and distance covered in a set time frame allows for objective tracking of improvement in mobility. For example, a patient who initially walks 20 meters in 30 seconds might improve to 30 meters in 30 seconds over time.
- Balance Metrics: Using tools like the Berg Balance Scale or Timed Up and Go test, allows for objective quantification of balance improvement. Changes in these scores reflect progress in regaining balance control.
- Gait Analysis: Analyzing gait patterns before and after the intervention can provide detailed insights into improvements in stride length, cadence, and posture. Video recordings, supplemented with gait analysis software, are useful.
- Patient Reported Outcomes: Collecting patient feedback on their perceived ability to perform reverse walking, pain levels, and any other relevant factors, offers a crucial subjective perspective. This subjective information is vital in evaluating overall improvement.
Monitoring Exercise Effectiveness
Monitoring the effectiveness of reverse walking exercises requires a structured approach. Regular evaluation is key to ensuring the exercise program remains appropriate for the patient’s evolving needs.
- Regular Follow-up Appointments: Scheduling regular follow-up appointments allows for consistent monitoring of progress, adjustments to the exercise program, and identification of any emerging issues.
- Objective Data Collection: Collecting objective data (e.g., gait speed, balance scores) at each follow-up appointment provides quantifiable evidence of the exercise’s impact.
- Subjective Feedback: Encouraging patients to provide feedback on their experience with reverse walking exercises helps gauge their comfort level and identify any areas where modifications might be needed.
- Documentation and Analysis: Thoroughly documenting all assessment findings and progress notes facilitates analysis and adaptation of the rehabilitation plan as needed.
Equipment and Resources: Reverse Walking In Physical Therapy
Reverse walking, while a beneficial exercise, can be tailored and supported by various equipment and resources. Understanding the tools available can enhance the safety and effectiveness of the therapy process. Choosing the right equipment is crucial for optimizing patient outcomes.This section details essential equipment for reverse walking exercises, along with valuable supplementary resources. Knowledge of assistive devices can greatly improve the patient experience and therapeutic approach.
Equipment for Reverse Walking Exercises
Appropriate equipment can significantly impact the effectiveness and safety of reverse walking exercises. This includes ensuring proper support, stability, and guidance during the exercise.
- Walking Aids: Canes, walkers, and crutches are crucial for patients with reduced mobility or balance issues. These tools provide additional support, allowing for more controlled and confident reverse walking. The type of assistive device selected will depend on the individual’s specific needs and limitations. For example, a quad cane might be more appropriate for someone with hip or knee pain, while a walker could be better suited for someone with significant lower extremity weakness.
- Resistance Bands: These bands can be used to increase the difficulty of the reverse walking exercise, particularly for patients who are already able to perform reverse walking without assistance. Resistance bands can be strategically positioned to target specific muscle groups, enhancing the effectiveness of the exercise. For example, a resistance band placed around the ankles can increase the demand on the leg muscles, promoting strength and endurance.
- Balance Boards: These boards can be used to challenge the patient’s balance and coordination, making reverse walking more challenging. This type of exercise is beneficial for patients with a history of falls or balance issues. For example, a balance board can be incorporated into reverse walking exercises to challenge the stability of the movement, gradually increasing the difficulty over time.
- Adjustable Height Platforms: These platforms allow for varying degrees of elevation, useful for reverse walking exercises focused on strengthening or stretching specific muscle groups. For instance, by adjusting the height, the exercise can be modified to address different needs or progress to more advanced levels.
Additional Resources for Learning More
Several resources are available to expand knowledge about reverse walking in physical therapy. Staying updated with the latest research and techniques is crucial for providing optimal care.
- Professional Journals: Publications like the Journal of Physical Therapy Science and the Archives of Physical Medicine and Rehabilitation regularly publish research articles on various aspects of physical therapy, including reverse walking. These journals provide valuable insights into the latest research findings and best practices.
- Online Courses and Workshops: Numerous online platforms offer courses and workshops on physical therapy techniques, including reverse walking. These resources provide practical training and knowledge exchange opportunities.
- Conferences and Seminars: Attending conferences and seminars dedicated to physical therapy provides an opportunity to learn from leading experts in the field. These events often feature presentations and workshops on topics such as reverse walking, enhancing understanding and skills.
- Expert Consultations: Consulting with experienced physical therapists specializing in gait rehabilitation can provide personalized guidance and insights into reverse walking techniques for specific patient cases. This individualized approach is particularly important for complex or challenging cases.
Examples of Assistive Devices
Assistive devices play a vital role in supporting patients during reverse walking exercises.
- Walkers: Walkers provide substantial support and stability, enabling individuals with reduced mobility or balance issues to perform reverse walking with greater confidence. Different walker types exist, each with varying levels of support. The choice of walker will depend on the patient’s specific needs.
- Canes: Canes offer a lighter form of support than walkers, assisting with balance and reducing strain on specific joints during reverse walking. Single-point and quad canes provide different levels of support, aiding the patient in maintaining their balance while performing the exercise.
- Crutches: Crutches are primarily used for patients with upper body or shoulder impairments, offering support and assisting in weight-bearing during reverse walking exercises. They can be used to reduce stress on the affected limb, facilitating the exercise safely and effectively.
Last Recap

Reverse walking in physical therapy presents a valuable tool for rehabilitation, offering a nuanced approach to improving gait and balance. By understanding the biomechanics, benefits, and safety precautions, therapists and patients can effectively utilize this technique to achieve optimal outcomes. We’ve covered the key aspects, from initial assessments to advanced progressions, enabling a more comprehensive understanding of this method.