How to treat an impaled object is a critical skill to possess. This guide will walk you through the essential steps for initial assessment, stabilization, first aid, and transport, ensuring the best possible outcome for the injured person. From recognizing potential dangers to understanding specific scenarios, this comprehensive approach will empower you to handle this challenging situation safely and effectively.
The initial assessment is paramount. Quickly evaluating the situation, determining the type of object, and preventing further injury are crucial first steps. Ignoring these steps could lead to more serious complications. The key is to act calmly and decisively.
Initial Assessment and Safety
Assessing a situation where someone has an impaled object requires immediate, calm action. Panicking can lead to further harm. The priority is to ensure the safety of everyone involved and to prevent any additional injuries. This involves a careful evaluation of the situation, and importantly, not attempting any self-treatment.
Safe Assessment of the Situation
A crucial initial step is to ensure the scene is safe. Evaluate the immediate surroundings for potential hazards. Is there a risk of falling debris, or other dangers that could put you or the injured person at further risk? If the scene is unsafe, carefully move the person to a safer location, while maintaining the impaled object’s stability.
It is vital to keep the impaled object from moving further, which could cause additional injury. This careful approach helps maintain the stability of the impaled object, reducing the risk of further damage.
Importance of Not Removing the Object
Attempting to remove an impaled object yourself is extremely dangerous. This action could cause more damage to the person’s body, increasing blood loss and nerve damage. The impaled object may be stabilizing a wound, and any sudden movement could disrupt the delicate balance of the situation. The vital organs and blood vessels may be at risk. The best course of action is to stabilize the person and the object, and seek professional medical help.
Dealing with an impaled object? First, try to keep calm and assess the situation. Don’t try to pull it out yourself; it could worsen the injury. Seeking immediate medical attention is crucial. While researching how to best handle this, I stumbled across an interesting article about natural remedies for erectile dysfunction, like ashwagandha for erectile dysfunction here.
Ultimately, though, remembering the importance of immediate professional help is key when it comes to impaled objects.
Preventing Further Injury
Preventing further injury is paramount. This involves controlling any visible bleeding by applying direct pressure to the wound. Keep the person still and comfortable. Maintain their body temperature. Avoid giving them anything to eat or drink.
Ensure that the person is not moving around or talking excessively, as this can cause additional stress and potential injury. This includes preventing any movement that could potentially dislodge the impaled object or cause further damage.
Potential Impaled Object Types and Initial Responses
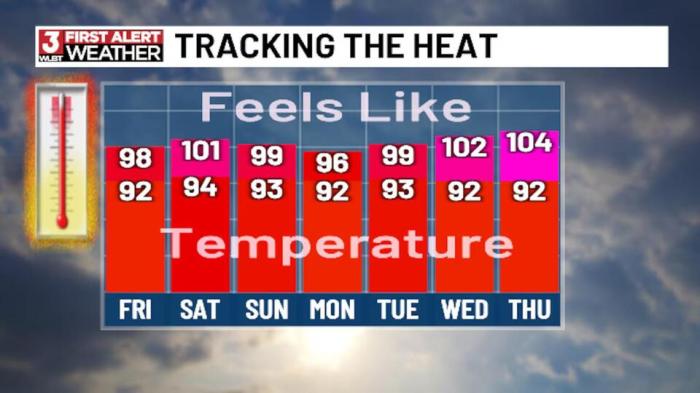
| Potential Impaled Object Types | Potential Dangers | Recommended Initial Responses |
|---|---|---|
| Wood | Possible deep penetration, potential for splinters, risk of infection | Immobilize the object, control bleeding, cover the wound loosely with a sterile dressing, seek immediate medical attention. |
| Metal | High risk of deep penetration, potential for broken bones or internal damage, potential for electrical shock if the metal is conductive | Immobilize the object, control bleeding, cover the wound loosely with a sterile dressing, seek immediate medical attention. Assess for electrical shock risks if appropriate. |
| Glass | Sharp edges, potential for deep cuts, risk of infection, possible eye injury if the object is close to the eye. | Immobilize the object, control bleeding, cover the wound loosely with a sterile dressing, seek immediate medical attention. Pay particular attention to any injuries around the eyes. |
Never attempt to pull out an impaled object yourself. This is extremely dangerous and could cause additional harm.
Stabilizing the Impaled Object
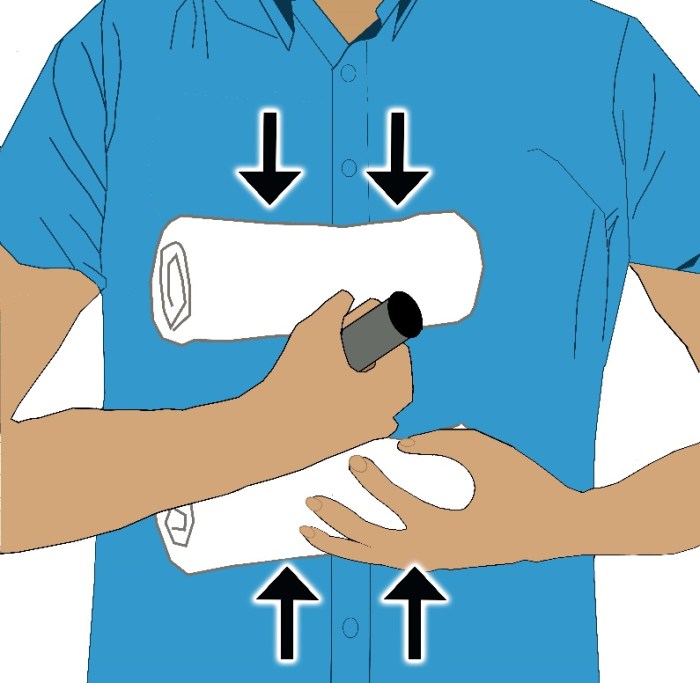
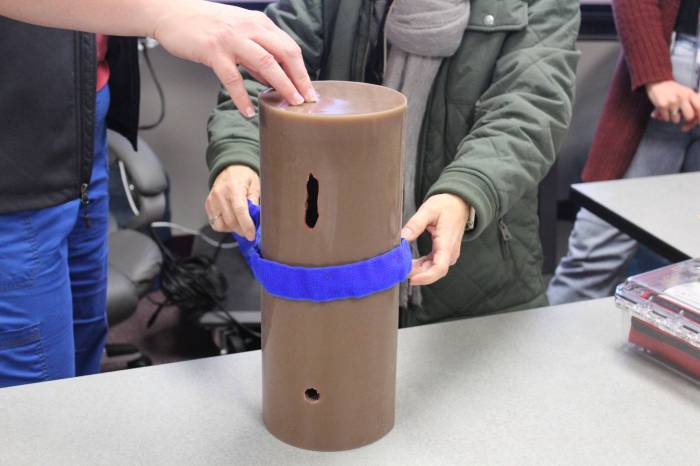
Once you’ve assessed the situation and ensured your safety, the next crucial step is stabilizing the impaled object. Moving the object could cause further injury to the victim. This process involves careful application of support and immobilization techniques to prevent any unintended movement of the object.
Methods for Stabilizing the Impaled Object
Stabilizing the impaled object involves creating a framework of support around the object without dislodging it. This approach aims to maintain the object’s position and prevent further harm to the underlying tissues. Different materials and methods can be employed depending on the available resources and the nature of the impaled object.
Using Readily Available Materials for Splinting
A variety of readily available materials can be used to create a makeshift splint or brace. The key is to create a stable framework that immobilizes the affected area and prevents the impaled object from shifting. Examples include sturdy sticks, cardboard, cloth, or even towels. These items can be fashioned into splints to support the area surrounding the impaled object, preventing further damage.
First aid for an impaled object involves careful stabilization, not removal. Before rushing to yank it out, consider whether almond milk is a good source of nutrients, which can be important for recovery. While you’re waiting for medical help, keeping the object stable is crucial to avoid further injury. Checking out is almond milk good for you might give you some insight into its nutritional value, but remember that proper medical attention is paramount when dealing with impaled objects.
Focus on keeping the injured area stable and preventing any more harm.
Immobilizing the Affected Area
Immobilizing the affected area is crucial to prevent any movement that could further injure the victim. This involves securing the impaled object and the surrounding area to prevent any unwanted shifting or movement. This is achieved through the application of bandages, dressings, or splints, ensuring that the affected area remains stable and protected. For example, a long stick impaled in the arm can be stabilized by wrapping a bandage around the arm, securing the stick in its place.
Examples of Immobilization Techniques
One technique involves using a sturdy stick or board as a splint. Place the stick along the affected limb, supporting the impaled object. Secure the splint in place with bandages or cloth, ensuring the object remains immobile. If the object is in the torso or neck, consider using a wide, soft material, such as a blanket, to support the area around the impaled object, followed by the use of cloth or bandages to stabilize it further.
Dealing with an impaled object? First, try to stabilize the object, preventing further movement. Don’t attempt to remove it yourself unless it’s a minor injury; a brain aneurysm headache, for example, could be a sign of a much more serious issue, and seeking immediate medical attention is critical. While you wait for help, keep the wound covered to prevent infection and control bleeding.
Remember, the correct procedure for treating an impaled object depends on the location and type of injury, so always prioritize professional medical assistance. how long does a brain aneurysm headache last is a question that needs immediate medical attention and shouldn’t be ignored. Ultimately, your safety and well-being hinge on proper medical handling of the situation.
This will prevent unnecessary movement and pain.
Table of Stabilization Methods
| Stabilization Method | Pros | Cons | Suitability for Impaled Object Types |
|---|---|---|---|
| Using a rigid stick as a splint | Simple, readily available, provides good support. | May not be suitable for all body regions or object types. | Long, relatively straight objects, such as sticks or metal rods. |
| Using a wide, soft material for support | Gentle support for sensitive areas like the neck or torso. | May not be as effective for stabilizing larger or irregularly shaped objects. | Blunt objects, irregular shapes. |
| Using bandages and dressings | Easy to apply, helps to contain bleeding and prevent infection. | May not be sufficient for large or irregularly shaped objects. | Smaller objects like arrows, knives, or glass shards. |
Immediate First Aid Measures
Controlling bleeding is crucial in managing an impaled object injury. Prompt and effective first aid can significantly reduce blood loss and improve the chances of a positive outcome. Understanding the different methods of controlling bleeding and knowing how to apply them correctly is vital for anyone encountering such a situation.Proper immediate action can help minimize the severity of the injury and complications.
A calm and systematic approach, following the established guidelines, is paramount in ensuring the best possible care for the injured person.
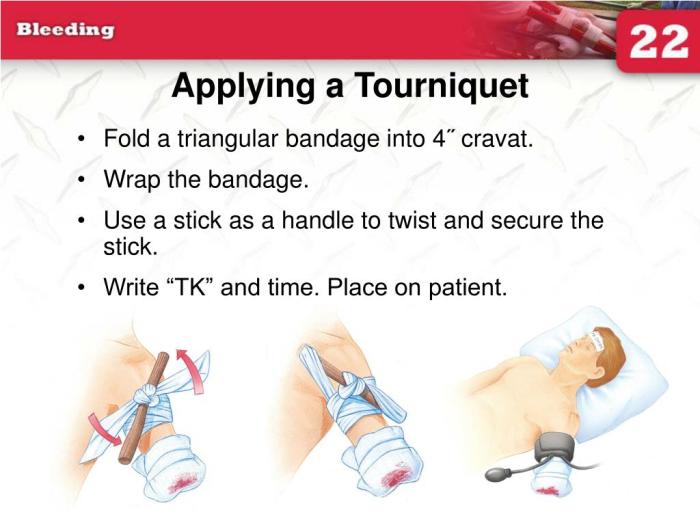
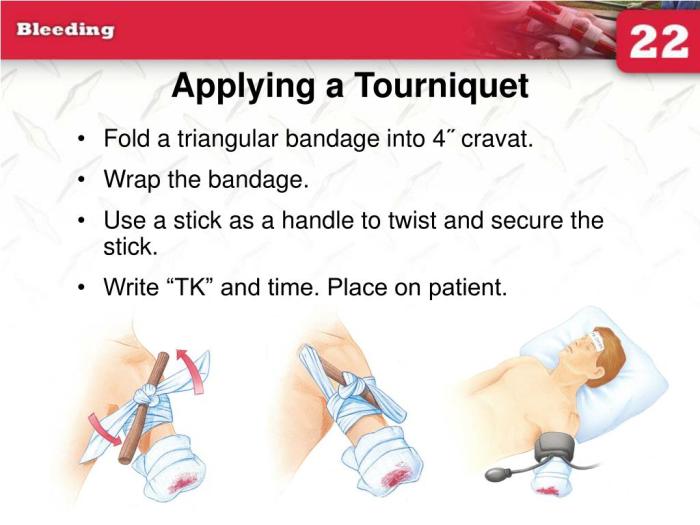
Controlling Bleeding
Effective bleeding control is essential in the initial stages of treating an impaled object injury. Uncontrolled bleeding can lead to shock, organ damage, and even death. The goal is to stop the flow of blood as quickly and safely as possible.
Applying Direct Pressure
Direct pressure is a fundamental technique for controlling bleeding. Applying firm, sustained pressure directly to the wound site is key. This helps to constrict blood vessels and reduce blood flow. A clean cloth or dressing should be used to apply the pressure. Avoid using excessive force, as this can cause further damage.
Elevating the Injured Area
Elevating the injured area above the heart helps to reduce blood flow to the wound. This is often done in conjunction with direct pressure. Elevating the injured limb or body part can significantly decrease blood loss, particularly if the impaled object is in an extremity. Care should be taken not to move the impaled object.
Essential First Aid Supplies
Having the right supplies readily available is crucial. A well-stocked first-aid kit can be the difference between a quick response and a delay in vital care.
- Clean cloths or gauze pads
- Sterile dressings
- Bandages (various sizes and types)
- Gloves (latex or nitrile)
- Scissors
- Tweezers
- Antiseptic wipes (optional)
Using Dressings and Bandages
Using the appropriate dressings and bandages is essential to effectively control bleeding and protect the wound. A clean, sterile dressing should be placed directly over the wound. Bandages are then used to secure the dressing and provide additional support. The type of bandage used will depend on the location and extent of the injury. Always prioritize the safety and well-being of the person receiving the first aid.
Comparison of Bleeding Control Methods
The effectiveness of various bleeding control methods varies depending on the specific situation.
| Method | Description | Effectiveness | Considerations |
|---|---|---|---|
| Direct Pressure | Applying firm pressure directly to the wound. | High | Requires consistent pressure and a clean dressing. |
| Elevation | Raising the injured area above the heart. | Moderate | Best used in conjunction with direct pressure. |
| Tourniquet | Tightly wrapping a material around the limb above the wound to cut off blood flow. | High (in extreme cases) | Should only be used as a last resort, as it can cause tissue damage if used incorrectly. Requires specific training. |
Transport and Medical Attention: How To Treat An Impaled Object
Getting a person with an impaled object to medical care safely and efficiently is paramount. Every second counts in these situations, and proper transport protocols minimize further harm and maximize the chances of a positive outcome. This section Artikels the crucial steps to ensure a safe and timely transfer to a medical facility.The primary goal in transporting a victim with an impaled object is to avoid unnecessary movement that could dislodge the object and cause further injury.
A controlled and methodical approach is essential. The safety of the victim and those assisting is equally important.
Safe Transport Procedures
Proper transport procedures are critical for minimizing risk. The key is to stabilize the impaled object and the victim’s condition to prevent additional injury during the transfer. Avoid unnecessary jostling or movement that could cause the object to shift or the victim to experience further pain. The following steps provide a comprehensive guide for safe transport.
- Assess the situation and surroundings for potential hazards. Ensure the environment is safe for both the victim and the rescuers.
- Maintain a calm and reassuring presence to reduce the victim’s anxiety and stress.
- Assess the victim’s breathing, circulation, and level of consciousness, continuously monitoring vital signs.
- Ensure the victim is positioned comfortably and safely to prevent further injury.
- Immobilize the victim if necessary, using appropriate splints or other supportive devices. Ensure the stabilization does not disrupt the impaled object.
- Protect the impaled object with padding to prevent movement or further damage. This prevents further injury.
Emergency Service Notification
Prompt notification of emergency services is crucial. Accurate and immediate communication is essential in these critical situations. This step can significantly impact the outcome of the incident.
- Contact emergency services (e.g., 911 or equivalent local number) immediately.
- Provide clear and concise information about the situation.
- Relay the exact location of the incident, including street addresses, landmarks, and any other details that will help emergency responders locate the scene quickly.
- Explain the nature of the injury, including the type of object and its location.
- Describe the victim’s condition and any visible injuries.
Key Information for Emergency Responders
Providing clear and concise information to emergency services is vital. This allows them to prepare appropriately for the situation and initiate appropriate procedures promptly.
- Type of Object: Describe the object precisely (e.g., metal rod, piece of wood, etc.) and its approximate size. This allows for appropriate handling and specialized equipment selection.
- Location of Impalement: Specify the exact body part where the object is lodged. This assists medical professionals in planning their approach and minimizing further damage.
- Victim’s Condition: Report the victim’s level of consciousness, breathing, and pulse. This information helps prioritize treatment and ensures appropriate measures are taken quickly.
- Time of Incident: Provide the approximate time the incident occurred. This information is crucial for determining the best course of action and the potential need for specialized care.
- Any other pertinent information: Include any other details that might help emergency responders. For instance, the cause of the impalement or any factors that might have influenced the victim’s condition. If you are aware of any medical conditions the victim may have, it is important to mention it.
Preventing Further Injury

Treating an impaled object requires meticulous attention to preventing further harm to the victim and the surrounding tissues. Maintaining stability and avoiding unnecessary movement is paramount. Improper handling can lead to severe complications, including nerve damage, internal bleeding, and even death. A systematic approach to stabilization and immediate first aid is crucial in minimizing these risks.
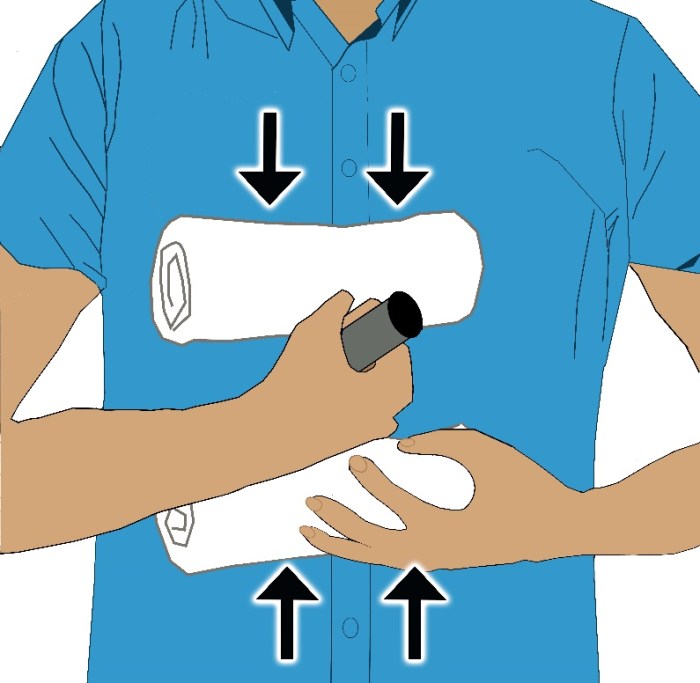
Maintaining Stability of the Impaled Object
Maintaining the stability of the impaled object is vital. Trying to remove it yourself can worsen the injury. Any attempt to dislodge the object before professional medical help arrives can cause further trauma to the victim. The object’s position should be stabilized using the methods described in the previous section. Avoid applying pressure directly on the impaled object, as this can force the object deeper into the body.
Instead, use firm, but gentle, supports to hold the object in place. A rigid structure such as a rolled-up towel or a board can be helpful.
Avoiding Further Damage to Surrounding Tissues
Preventing further damage to the surrounding tissues is crucial. Movement or pressure on the impaled area can cause further lacerations, bruising, and damage to blood vessels and nerves. It’s important to minimize movement and avoid any action that might push the object deeper into the body. Gently padding the area around the impaled object with sterile dressings or clean cloths can help to reduce friction and pressure.
The key is to maintain the object’s position and stabilize the affected area without applying pressure to the wound.
Preventing Shock and Other Potential Complications
Preventing shock is paramount. Severe injuries, such as those involving impaled objects, can lead to shock. Maintaining the victim’s body temperature, ensuring adequate breathing, and controlling bleeding are critical in preventing shock. Additional complications, such as infections, can arise if the wound is not properly treated. The victim should be kept comfortable and reassured.
Maintaining a calm and controlled environment is essential in reducing anxiety and potential complications.
What NOT to Do
Attempting to remove the impaled object yourself is extremely dangerous. This action can cause further damage and increase the risk of internal bleeding, nerve damage, or even death. Never try to pull or twist the object, as this could cause the object to rotate or move deeper into the body. Applying pressure directly to the object is also a critical mistake.
Instead, prioritize stabilization and seek professional medical help immediately.
Table of Potential Dangers of Improper Handling
| Potential Danger | Preventative Measure |
|---|---|
| Further tissue damage | Maintain stability of the impaled object. Minimize movement of the injured area. |
| Internal bleeding | Stabilize the object, control bleeding using direct pressure on the wound, but not on the impaled object. |
| Nerve damage | Avoid unnecessary movement of the object. Stabilize the area with supportive materials. |
| Infection | Keep the wound covered and sterile. Seek immediate medical attention. |
| Shock | Maintain the victim’s body temperature and breathing. Keep the victim calm and reassured. |
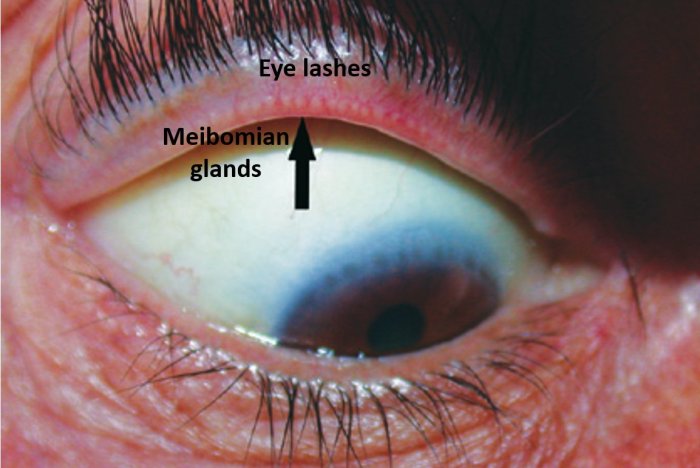
Types of Impaled Objects and Their Treatments
Understanding the type of impaled object is crucial for effective first aid. Different objects require specific stabilization techniques to prevent further injury and ensure proper transport to medical facilities. The nature of the object—whether sharp, blunt, or foreign—dictates the approach to handling the situation. Careful assessment and appropriate stabilization are paramount in minimizing harm.Knowing the material of the impaled object is equally important.
Different materials react differently to force, and some may be more likely to cause internal damage. This knowledge empowers you to make informed decisions about how to manage the situation, while understanding the object’s potential for harm.
Sharp Objects
Sharp objects, like knives or metal shards, pose a significant risk of deeper penetration and potential internal damage. Stabilization is critical to prevent further injury. A crucial aspect is to avoid directly manipulating the object, as this can worsen the situation. The object should be stabilized in its current position.
Blunt Objects, How to treat an impaled object
Blunt objects, such as pieces of wood or bone, often cause significant trauma to the surrounding tissues. The focus in these cases is on stabilizing the object and managing the associated soft tissue injuries. Significant force might have been involved, and there’s a high chance of associated fractures or other injuries. Therefore, proper immobilization is key to avoid exacerbating the damage.
Foreign Objects
Foreign objects, such as splinters or pieces of glass, require careful handling. The stabilization process should minimize further damage to the surrounding tissue and prevent the object from shifting. Factors like the material and size of the object greatly influence the approach to stabilization. Often, a gentle approach is necessary to avoid causing further harm.
Material Considerations
The material of the impaled object significantly affects stabilization techniques. For example, a wooden stick may be more easily stabilized with a supportive bandage compared to a sharp metal object. The potential for infection is also a consideration. A metal object might require special attention to prevent contamination, while a wooden object might require different considerations.
Importance of Understanding the Object’s Nature
Accurate assessment of the impaled object’s type, sharpness, and material is crucial for appropriate stabilization and transport. A wrong assessment can lead to complications, further injury, and even life-threatening outcomes. Misjudging the nature of the object can result in serious errors in handling the situation.
Handling Procedures
| Type of Impaled Object | Handling Procedures |
|---|---|
| Sharp Objects | Stabilize in place; avoid directly manipulating; consider using bulky dressings or splints to hold it steady |
| Blunt Objects | Stabilize in place, ensuring no further movement; use padding and supportive dressings to minimize pressure on surrounding tissue; immobilize the affected area |
| Foreign Objects | Stabilize in place; avoid removing unless it’s a life-threatening risk; if removal is necessary, use sterile instruments |
Potential Complications and Prognosis
Treating an impaled object involves navigating a delicate balance between immediate stabilization and long-term recovery. While the initial focus is on removing the object and preventing further injury, potential complications can arise from both the injury itself and the subsequent treatment. Understanding these potential complications, along with the importance of ongoing monitoring and follow-up care, is crucial for ensuring a positive prognosis.
A thorough understanding of these potential issues can help both the patient and medical professionals to anticipate and address potential problems.The impact of an impaled object extends beyond the immediate wound. The object’s trajectory, the tissues it penetrates, and the force of the impact can all contribute to a range of potential complications. The prognosis for recovery hinges on factors like the extent of tissue damage, the presence of infection, and the patient’s overall health.
Early intervention and meticulous care significantly improve the chances of a favorable outcome.
Potential Complications
A wide array of complications can arise from impaled objects, stemming from the initial trauma to the body’s systems. These range from the immediate to the long-term, impacting various aspects of health and well-being.
- Infection: Penetration of the skin and underlying tissues creates pathways for bacteria to enter and proliferate. Infection can range from localized abscesses to systemic sepsis. Prompt and appropriate antibiotic treatment is critical to control and prevent infection.
- Internal Bleeding: The impaled object can damage blood vessels, leading to internal bleeding. The severity of the bleeding depends on the size and location of the damaged vessels. This can be a life-threatening complication and requires prompt medical intervention.
- Nerve Damage: Penetration of nerves can result in varying degrees of nerve damage. This damage can cause temporary or permanent sensory loss, motor dysfunction, or pain. The specific type and severity of nerve damage depends on the location and extent of the injury.
- Organ Damage: Impalement can directly damage internal organs, such as the lungs, liver, spleen, or kidneys. The extent of organ damage varies depending on the location and force of the impact. Organ damage may require surgical intervention and prolonged recovery.
- Blood Vessel Thrombosis: Damage to blood vessels can lead to blood clots (thrombosis). These clots can block blood flow to vital organs and tissues, resulting in further complications. Prompt treatment is necessary to prevent or minimize the risk of blood clots.
- Fistula Formation: A fistula is an abnormal connection between two body parts. Impalement can create fistulas, causing drainage of bodily fluids or pus, which necessitates surgical correction.
Monitoring for Infection
Close monitoring is crucial to identify and treat infections early.
- Signs of Infection: Watch for increasing pain, swelling, redness, warmth, pus discharge, fever, chills, and a general decline in the patient’s overall condition.
- Frequency of Monitoring: The frequency of monitoring depends on the severity of the injury and the presence of any other complications. Regular check-ups and assessments are necessary to detect any emerging problems.
- Importance of Medical Attention: Any signs of infection should be reported to the treating physician immediately. Prompt medical attention is essential to prevent the infection from spreading and causing further complications.
Long-Term Effects and Prognosis
The long-term effects and prognosis of an impaled object injury depend on several factors. Early intervention and appropriate treatment are crucial to minimizing long-term complications.
- Functional Limitations: Nerve damage or other injuries can lead to long-term functional limitations. Rehabilitation may be necessary to regain lost function.
- Scarring: The impaled object injury may leave significant scarring. The extent of scarring depends on the depth and location of the injury. Scar management and treatment may be required.
- Psychological Impact: Severe injuries can have a significant psychological impact on the patient. Support and counseling may be necessary to help the patient cope with the emotional and psychological challenges.
Specific Cases and Scenarios
Treating an impaled object requires careful consideration of the location and type of object. A standardized approach, while crucial, must be adaptable to the unique circumstances of each case. The focus should always be on minimizing further harm and ensuring the best possible outcome for the victim. Different body areas present unique challenges and necessitate specialized care.The critical first step in managing an impaled object is to assess the situation and the patient’s overall condition.
Initial assessment focuses on the stability of the impaled object, the presence of life-threatening injuries, and any additional injuries. The specific treatment will then depend on the location of the impaled object and the potential complications.
Impaled Objects in the Chest
Chest injuries involving impaled objects are particularly serious due to the vital organs located in the area. Immediate stabilization of the object is paramount to prevent further damage to the heart, lungs, or major blood vessels. Carefully assess the stability of the object. Attempting to remove it yourself could worsen the situation. The priority is to control any bleeding and ensure adequate breathing.
A person with an impaled object in the chest should receive immediate medical attention.
Impaled Objects in the Abdomen
Impaled objects in the abdomen pose a significant threat to the internal organs. The risk of internal bleeding and damage to vital organs is high. Stabilization is crucial. Do not attempt to remove the object yourself. Maintain the patient’s airway and ensure adequate breathing.
The priority is to control bleeding and maintain the patient’s stability until professional medical help arrives. Immediate medical intervention is essential.
Impaled Objects in the Extremities
Impaled objects in the extremities, while potentially less life-threatening than injuries to vital organs, still require careful attention. Stabilize the object to prevent further injury. Control any bleeding using direct pressure. Ensure the limb is supported and not moved unnecessarily. Thorough assessment is critical to rule out additional damage.
Impaled Objects in the Head or Neck
Impaled objects in the head or neck are among the most serious types of injuries. Immediate stabilization is paramount to prevent further damage to the brain or spinal cord. Do not attempt to remove the object yourself. Keep the patient’s head and neck stable. The primary focus is on maintaining a clear airway and controlling bleeding.
These injuries necessitate immediate and specialized medical attention. A skilled medical professional is needed to assess the extent of the damage.
Treatment Considerations by Body Location
| Body Location | Treatment Considerations |
|---|---|
| Chest | Stabilize the object, control bleeding, ensure breathing, and seek immediate medical attention. |
| Abdomen | Stabilize the object, control bleeding, maintain airway, and seek immediate medical attention. |
| Extremities | Stabilize the object, control bleeding, support the limb, and seek medical attention. |
| Head/Neck | Stabilize the object, maintain airway, control bleeding, and seek immediate specialized medical attention. |
Prevention and Education
Impalement injuries, though often accidental, can be largely prevented through proactive safety measures and education. Understanding the potential hazards in various environments and activities, and adopting appropriate safety precautions, significantly reduces the risk of these types of injuries. This section Artikels preventive strategies and highlights specific activities and environments where impalement is a more significant concern.
Preventing Impalement Injuries
Preventing impalement injuries involves a multi-faceted approach focusing on awareness, preparation, and adherence to safety guidelines. This approach includes a strong emphasis on anticipating potential dangers and taking steps to mitigate them.
Safety Tips for Specific Activities
Several activities carry a higher risk of impalement. Awareness of these risks and adherence to safety precautions are crucial.
- Outdoor Activities: Activities like hiking, camping, and gardening can involve encounters with sharp objects. Wearing sturdy footwear, avoiding walking near fallen branches or debris, and being cautious when using tools like shovels or saws are important precautions. For example, always check your surroundings for potential hazards before working in a wooded area.
- Construction and Industrial Settings: Construction sites, factories, and workshops frequently use tools and equipment that can cause impalement injuries. Strict adherence to safety protocols, including wearing appropriate protective gear (e.g., safety glasses, gloves, and vests), and following established safety procedures, is critical in these environments.
- Recreational Activities: Sports like fishing, hunting, and playing with potentially sharp objects require particular attention to safety precautions. Using appropriate equipment and maintaining situational awareness when handling these items are essential. For instance, using appropriate hooks and tackle, as well as practicing caution when walking through wooded areas during hunting season, can help mitigate risk.
High-Risk Environments
Certain environments inherently pose a greater risk of impalement. Understanding these risks and implementing appropriate safety measures is paramount.
- Construction Sites: The presence of numerous sharp objects, heavy machinery, and potentially unstable structures increases the risk of impalement. Regular safety inspections, strict adherence to safety protocols, and proper training are essential for reducing hazards.
- Woodlands and Forests: Fallen branches, sharp tree limbs, and debris present a significant impalement risk, particularly during outdoor activities like hiking and camping. Careful navigation, awareness of surroundings, and avoiding contact with potential hazards are critical in these environments.
- Industrial Settings: The presence of heavy machinery, sharp tools, and other potential impalement hazards demands stringent safety protocols and proper protective gear to prevent injuries.
Importance of Safety Precautions
Safety precautions are crucial for preventing impalement injuries. Their importance stems from the potential for severe and lasting consequences from these types of injuries.
Safety Tips and Preventive Measures
| Activity/Environment | Safety Tips | Preventive Measures |
|---|---|---|
| Outdoor Activities | Wear sturdy footwear, avoid walking near debris, be cautious with tools | Regular inspections of equipment, clear paths, and appropriate clothing |
| Construction/Industrial Settings | Use protective gear, follow safety procedures, maintain equipment | Strict adherence to safety regulations, comprehensive training, and regular safety inspections |
| Recreational Activities | Use proper equipment, maintain situational awareness | Thorough equipment maintenance, clear guidelines, and safety briefings |
| Woodlands/Forests | Be aware of surroundings, avoid contact with hazards | Clear paths, regular trail maintenance, and appropriate footwear |
| Industrial Settings | Use protective gear, follow procedures | Regular safety inspections, training, and maintenance |
Conclusion
In conclusion, treating an impaled object requires a systematic approach. Knowing how to stabilize the object, control bleeding, and ensure safe transport is vital. This guide provides a framework for immediate action, empowering you to take the necessary steps to prevent further harm and ensure the best possible outcome. Remember, prompt and appropriate action can significantly impact the recovery process.
Seeking immediate medical attention is always recommended.