Can I keep working with fibromyalgia and CFS? This question is crucial for many, as these conditions can significantly impact daily life and work performance. This guide explores the complexities of maintaining employment while living with fibromyalgia (FM) and chronic fatigue syndrome (CFS), providing insights into understanding these conditions, exploring work options, managing symptoms, and understanding legal rights.
We’ll also delve into practical strategies for success, illustrated with real-life examples.
Fibromyalgia and CFS often present overlapping symptoms, including chronic pain, fatigue, sleep disturbances, and cognitive difficulties. These conditions can make it challenging to maintain consistent work routines, but with the right strategies and accommodations, many individuals can continue their careers while effectively managing their symptoms.
Understanding Fibromyalgia and CFS

Navigating the complexities of fibromyalgia (FM) and chronic fatigue syndrome (CFS) often feels like walking through a dense fog. These conditions, while distinct, frequently overlap in their symptoms, creating a unique challenge for those living with them. This exploration delves into the nature of these conditions, their impact on daily life, and the support strategies available in the workplace.Fibromyalgia and CFS are chronic conditions characterized by a constellation of symptoms that can significantly affect a person’s ability to function.
Figuring out if you can keep working with fibromyalgia and CFS can be tough. One common symptom that can significantly impact daily life is digestive issues, like diarrhea. Finding effective relief, whether from over-the-counter options or prescription medications, is crucial for maintaining a routine. For a comprehensive look at diarrhea relief otc and prescription medications, check out this helpful resource: diarrhea relief otc and prescription medications.
Ultimately, managing these symptoms is key to maintaining your ability to work and live a fulfilling life with these conditions.
The key to understanding them lies in recognizing the multifaceted nature of their impact, from physical discomfort to cognitive impairment. The interplay of these symptoms makes it crucial to approach their management with a holistic perspective.
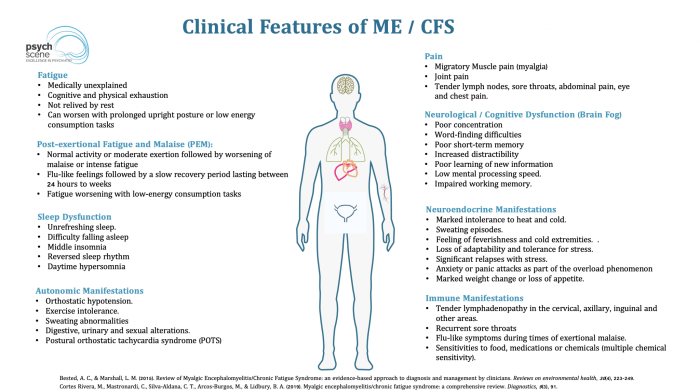
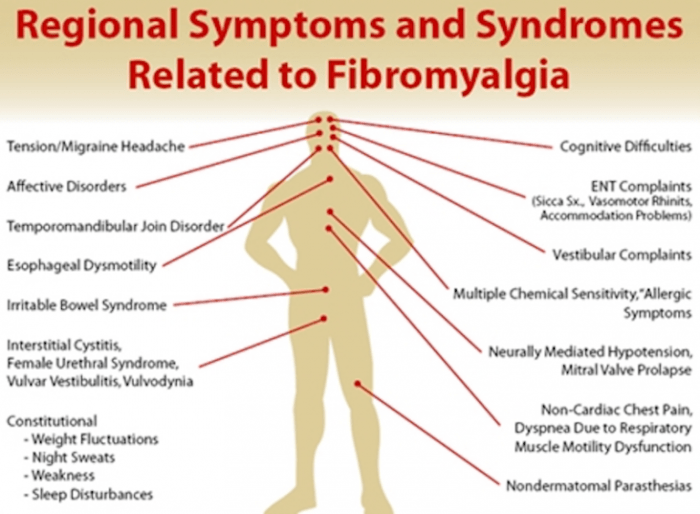
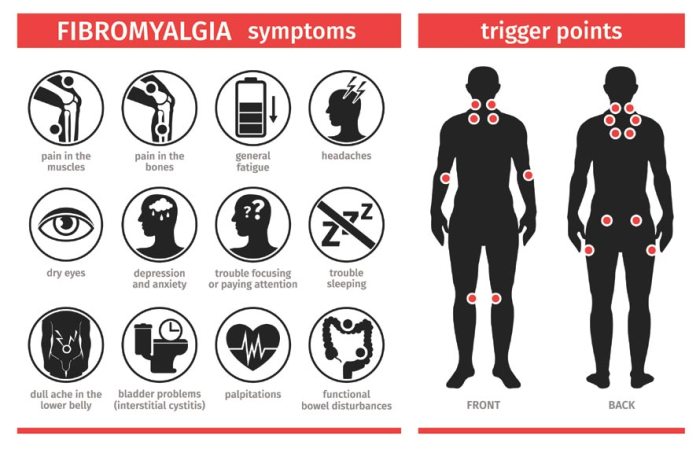
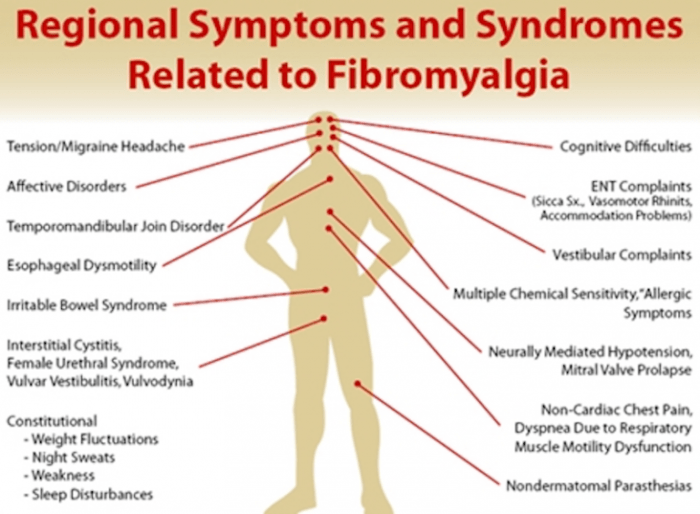
Symptoms and Overlap
Fibromyalgia and CFS share several symptoms, making diagnosis and management challenging. These overlapping symptoms often include widespread pain, fatigue, sleep disturbances, and cognitive difficulties. While the underlying mechanisms aren’t fully understood, research suggests that these conditions may involve a complex interplay of factors, including genetic predisposition, environmental triggers, and the body’s immune response.
Impact on Daily Activities and Work Performance
The pervasive nature of fibromyalgia and CFS symptoms profoundly affects daily activities. Simple tasks that most people take for granted, like grocery shopping, cleaning, or even engaging in social activities, can become monumental challenges. Similarly, work performance can suffer due to fatigue, pain, and cognitive difficulties. Concentrating, completing tasks, and maintaining productivity can become exceedingly difficult. This can lead to missed deadlines, reduced output, and even job loss in severe cases.
Common Workplace Challenges, Can i keep working with fibromyalgia and cfs
Individuals with fibromyalgia and CFS often encounter unique challenges in the workplace. These challenges frequently stem from the unpredictable nature of symptoms and the need for accommodations to manage them effectively. Common workplace difficulties include:
- Sustaining concentration and focus: Fluctuating energy levels and cognitive difficulties can make it challenging to remain focused on tasks and maintain productivity throughout the workday.
- Maintaining consistent work output: The unpredictable nature of symptoms often leads to fluctuations in energy and ability to perform tasks, potentially impacting productivity.
- Managing pain and fatigue: The persistent pain and fatigue associated with these conditions can make it challenging to perform tasks requiring physical or mental exertion, requiring appropriate accommodations.
- Difficulty with communication and social interaction: Cognitive difficulties and fatigue can impair communication skills, leading to misunderstandings or social isolation.
Work Accommodations
A range of accommodations can be implemented to help individuals with fibromyalgia and CFS manage their symptoms and maintain their employment. These accommodations can be tailored to the specific needs of the individual and the nature of their job. Some examples include:
- Flexible work schedules: Adjusting work hours to accommodate fluctuating energy levels and pain episodes.
- Ergonomic adjustments: Modifying workspaces to minimize physical strain and pain, such as adjusting seating, lighting, or workstation setup.
- Reduced workload: Adjusting responsibilities to align with fluctuating energy levels and cognitive capabilities.
- Access to supportive resources: Providing access to resources like a quiet workspace, frequent breaks, or assistive technology.
Table: Fibromyalgia and CFS Conditions
| Condition | Symptoms | Potential Work Impacts |
|---|---|---|
| Fibromyalgia | Widespread pain, fatigue, sleep disturbances, cognitive difficulties, mood changes | Reduced productivity, difficulty concentrating, missed deadlines, absenteeism |
| Chronic Fatigue Syndrome | Extreme fatigue, muscle pain, headaches, cognitive impairment, sleep disturbances | Inability to maintain work pace, difficulty with communication, reduced job satisfaction, potential job loss |
Exploring Work Options

Navigating the world of work with fibromyalgia and chronic fatigue syndrome (CFS) can feel daunting. However, understanding the various work arrangements available and tailoring your approach to your specific needs can significantly improve your quality of life and maintain your career. This section delves into the possibilities, highlighting options that can help you balance your professional responsibilities with your health conditions.Remote work, flexible schedules, and modified job tasks can all play a vital role in managing symptoms and maintaining a fulfilling career.
By exploring these possibilities, individuals with FM and CFS can often find solutions that work for them, enabling them to continue contributing to the workplace while prioritizing their health.
Remote Work Options
Remote work offers a unique opportunity for individuals with FM and CFS to manage their symptoms. The flexibility of working from home allows for greater control over the environment, reducing potential triggers and stressors.
- Advantages: Reduced commute stress, greater control over the work environment (temperature, lighting, noise levels), and potential for increased flexibility in scheduling.
- Disadvantages: Potential for increased isolation, difficulty separating work and personal life, and the need for reliable internet and technology infrastructure.
Flexible Work Schedules
Flexible work schedules, including compressed workweeks and flexible hours, can provide a vital balance between work and personal needs. They allow for better symptom management by providing more control over daily routines.
- Compressed Workweeks: Working a full week’s hours in fewer days, potentially reducing travel and overall time spent in the workplace.
- Flexible Hours: Adjusting start and end times to fit individual needs, allowing for periods of rest or symptom management during the workday.
Modified Job Tasks and Responsibilities
Adapting job tasks and responsibilities is crucial for maintaining productivity and well-being. This may involve adjusting the complexity of tasks, the amount of time spent on specific tasks, or changing the work environment to accommodate needs.
- Examples: Decreasing the workload, delegating tasks, focusing on projects that allow for shorter work periods, and taking frequent breaks to avoid fatigue.
Work Model Suitability Table
The table below provides a general overview of various work models and their potential suitability for managing symptoms associated with FM and CFS. It’s important to note that this is a general guideline and individual experiences may vary.
| Work Model | Potential Advantages | Potential Disadvantages | Suitability for FM/CFS (High/Medium/Low) |
|---|---|---|---|
| Remote Work | Reduced commute, controlled environment | Potential isolation, blurred work/life balance | High |
| Compressed Workweek | Reduced travel time, potential for better scheduling | Requires advanced planning, potentially impacting team dynamics | Medium |
| Flexible Hours | Increased autonomy, better personal management | Potential difficulty in maintaining consistent team communication | Medium-High |
| Modified Job Tasks | Reduced workload, greater control over responsibilities | May require adjustment of expectations, communication with management | High |
Managing Symptoms at Work
Working with fibromyalgia and CFS can be challenging, but it’s possible to manage symptoms and maintain a fulfilling work life. Effective strategies are crucial for navigating the daily demands of employment while addressing the unique needs of these conditions. This section explores practical methods for symptom management in the workplace, including pain, fatigue, and other related issues.Successfully navigating the workplace with fibromyalgia and CFS requires proactive strategies for symptom management.
These strategies involve understanding your own body’s limitations, communicating effectively with your employer, and establishing a work routine that accommodates your specific needs. By prioritizing tasks, pacing yourself, and effectively delegating, you can maintain productivity and well-being.
Strategies for Managing Pain
Effective pain management in the workplace involves proactive measures. Chronic pain associated with these conditions can significantly impact work performance. Implementing strategies for managing pain at work allows for improved focus and productivity. This includes employing techniques like heat or cold therapy, gentle stretching, and taking breaks throughout the workday to avoid prolonged periods of inactivity. Regular breaks help to prevent pain from escalating.
Strategies for Managing Fatigue
Fatigue is a frequent and significant symptom for individuals with fibromyalgia and CFS. Fatigue management strategies are essential to maintain work productivity. Employing pacing techniques, like scheduling tasks and activities, and prioritizing tasks, can be instrumental in managing energy levels. This involves recognizing your energy levels throughout the day and adjusting your workload accordingly. Prioritizing urgent tasks helps maintain focus and productivity.
Strategies for Pacing and Prioritizing Tasks
Pacing oneself is crucial for maintaining work productivity while managing symptoms. Developing a system for prioritizing tasks is important for managing energy levels. This involves creating a daily schedule that considers energy levels and tasks. Prioritizing tasks based on urgency and importance ensures that the most critical tasks are completed first. It’s vital to avoid overexertion and incorporate rest periods into the schedule.
Figuring out if you can keep working with fibromyalgia and CFS can be tricky. It really depends on your specific symptoms and how they impact your daily life. Understanding how long immunity lasts after a COVID booster shot, like in immunity duration after covid booster , can help you make informed decisions about your health and work life balance.
Ultimately, prioritizing your well-being and seeking professional guidance is key to navigating these challenges successfully.
Time Management and Task Delegation
Time management techniques are essential for individuals with fibromyalgia and CFS. Time management involves organizing tasks, scheduling work, and delegating tasks when possible. Delegating tasks effectively can reduce workload and allow for better symptom management. Prioritizing and breaking down tasks into smaller, manageable steps can enhance efficiency and reduce feelings of overwhelm. This also helps to maintain focus and concentration.
Communication with Employers
Effective communication with employers is crucial for managing symptoms at work. Open and honest communication about your needs and limitations is vital. Providing your employer with a clear understanding of your condition allows them to provide the necessary support. This may involve discussing flexible work arrangements, adjusted deadlines, or specific accommodations to support your health needs. Seeking support from human resources or a workplace support group can also be beneficial.
Summary Table of Strategies for Symptom Management at Work
| Symptom | Strategies | Practical Tips |
|---|---|---|
| Pain | Heat/cold therapy, stretching, regular breaks | Use a heating pad, take short walks, stretch regularly. |
| Fatigue | Pacing, prioritizing, scheduling | Create a daily schedule, break tasks into smaller parts, take frequent short breaks. |
| General | Time management, task delegation, communication | Use a planner, delegate tasks when possible, discuss needs with employer. |
Legal Rights and Workplace Accommodations
Navigating the complexities of fibromyalgia (FM) and chronic fatigue syndrome (CFS) in the workplace can be challenging. Understanding your legal rights and how to effectively communicate your needs to your employer is crucial for maintaining employment and well-being. This section delves into the legal protections available to individuals with FM and CFS, focusing on the Americans with Disabilities Act (ADA) and the practical steps for requesting and securing workplace accommodations.
Legal Protections Under the Americans with Disabilities Act (ADA)
The Americans with Disabilities Act (ADA) is a landmark piece of legislation that prohibits discrimination against individuals with disabilities in employment. This legislation ensures that qualified individuals with FM and CFS are not denied opportunities or subjected to unfair treatment in the workplace. The ADA recognizes FM and CFS as disabilities, provided they substantially limit one or more major life activities.
This means that if your FM or CFS significantly impacts your ability to perform essential job functions, you may be eligible for reasonable accommodations.
Understanding Reasonable Accommodations
Reasonable accommodations are adjustments or modifications to the work environment or job duties that allow an individual with a disability to perform the essential functions of their job. These accommodations aim to level the playing field, ensuring equal opportunity for individuals with FM and CFS. Examples of reasonable accommodations include flexible work schedules, modified work tasks, assistive technologies, and adjustments to the work environment.
Requesting and Obtaining Accommodations
The process for requesting and obtaining accommodations involves open communication and collaboration between the employee and the employer. A crucial step is documenting the impact of your condition on your job performance. This documentation can include medical records, self-reported symptom diaries, and notes from healthcare professionals. It is essential to provide specific examples of how your condition affects your ability to perform certain tasks or attend work consistently.
Importance of Clear Communication
Maintaining open and honest communication with your employer is paramount. Clearly articulate your needs and the specific accommodations you require. Provide concrete examples of how the accommodations will help you perform your job duties effectively. This clear communication fosters a collaborative environment and increases the likelihood of a positive outcome.
Figuring out if you can keep working with fibromyalgia and CFS can be tough. It really depends on the severity of your symptoms and the specific demands of your job. Learning about the intricate workings of your digestive system, like the fascinating facts about your colon facts about your colon , might seem unrelated, but understanding your body’s overall function is key to managing these conditions.
Ultimately, discussing your specific situation with your doctor and exploring possible accommodations at work is crucial to finding a sustainable work-life balance.
Example Scenarios
- An employee with FM experiences debilitating fatigue in the afternoon. A reasonable accommodation might be adjusted work hours or the opportunity to take short breaks throughout the day.
- A worker with CFS experiences heightened sensitivity to certain sounds and lighting in the workplace. An accommodation could be relocating to a quieter space or adjusting lighting in their work area.
- An individual with FM experiences pain that makes sitting for long periods difficult. A reasonable accommodation could be providing a standing desk or the ability to take breaks more frequently to stretch and move around.
Documentation and Support
Thorough documentation of your condition and its impact on your work is crucial. This documentation should include medical records, symptom diaries, and any other relevant information that illustrates the need for accommodation. Seek support from disability advocates or legal professionals if needed. They can provide guidance and support throughout the accommodation process.
Strategies for Success
Finding employment while living with fibromyalgia (FM) and chronic fatigue syndrome (CFS) requires a unique approach. It’s not about ignoring symptoms or sacrificing well-being, but rather about strategically managing them and adapting work environments. Successful employment for individuals with these conditions often hinges on understanding personal limitations, building resilience, and seeking support.This journey demands a multifaceted approach. Successful individuals prioritize self-advocacy, setting achievable goals, and seeking professional guidance.
The focus shifts from a fixed definition of “success” to a flexible, personalized one that accommodates symptoms and well-being. Adapting to workplace challenges, while also maintaining personal well-being, is crucial.
Success Stories and Personal Experiences
Many individuals with FM and CFS have not only maintained employment but have thrived. Their stories highlight the power of proactive strategies. For instance, a software engineer with FM discovered that working from home and using adaptive technology significantly improved her productivity. Similarly, a teacher with CFS found that a flexible schedule and a supportive administration allowed her to manage her symptoms effectively.
These examples underscore the potential for success when individuals take an active role in their career paths.
Importance of Self-Advocacy and Realistic Goals
Self-advocacy is key to navigating the workplace with FM and CFS. This involves clearly communicating needs and limitations to employers. It’s not about demanding special treatment, but about openly discussing accommodations and strategies for managing symptoms. Establishing realistic goals, broken down into manageable steps, is also crucial. Instead of aiming for a demanding workload immediately, focus on demonstrating consistent productivity within a comfortable capacity.
Gradually increasing responsibilities, with careful monitoring of symptom impact, will contribute to long-term success.
Seeking Professional Support and Guidance
Seeking professional support is invaluable. A doctor, therapist, or counselor can provide personalized strategies for symptom management and emotional well-being. A coach specializing in chronic illness can help develop strategies for self-management, time management, and navigating workplace challenges. This support system can provide vital guidance in adjusting expectations and setting realistic work goals.
Strategies for Building Resilience and Coping with Challenges
Building resilience is paramount. Techniques like mindfulness, meditation, and stress-reduction exercises can help manage the emotional toll of chronic illness. Establishing a routine, prioritizing self-care, and creating a supportive network of friends and family can enhance overall well-being. Learning to say “no” to tasks that exacerbate symptoms is a crucial aspect of self-care.
Key Strategies for Workplace Success
- Open Communication with Employers: Clearly articulate your needs and limitations, focusing on practical accommodations rather than special treatment. Maintain open dialogue about your health condition and its impact on work.
- Establish a Routine: A structured daily routine can improve predictability and stability, helping to manage symptoms. This includes prioritizing rest and downtime.
- Time Management Techniques: Employ strategies to manage workload effectively, including task prioritization and timeboxing. Breaking down tasks into smaller, more manageable segments can significantly reduce symptom exacerbation.
- Symptom Tracking and Awareness: Maintain a log of symptoms, triggers, and responses to various activities. This awareness allows for proactive adjustments in daily activities and workload to avoid symptom escalation.
- Prioritize Self-Care: Regular exercise, a balanced diet, and sufficient sleep are essential for managing symptoms. Make self-care a priority, not an afterthought.
- Adaptive Technology: Explore assistive technologies that can support productivity and efficiency, such as ergonomic equipment, software for task management, or voice-activated tools.
Illustrative Case Studies: Can I Keep Working With Fibromyalgia And Cfs
Navigating the complexities of work with fibromyalgia (FM) and chronic fatigue syndrome (CFS) can be challenging, but it’s absolutely possible with the right support and strategies. These case studies highlight real-world scenarios and successful approaches to help you understand how individuals with FM and CFS have overcome obstacles and thrived in their professional lives. The key is proactive communication, understanding accommodations, and a willingness to advocate for yourself.Successful management of work-related challenges requires understanding the nuances of each individual’s condition and their specific workplace environment.
Factors like the nature of the job, company culture, and available resources all play a role in how effectively accommodations are implemented. These case studies illustrate how individuals with FM and CFS can thrive with the right approach.
Case Study 1: The Adaptable Accountant
Sarah, a highly organized accountant, experienced increasing fatigue and pain over time. Her work involved long hours, complex spreadsheets, and frequent meetings. She started experiencing noticeable symptoms like muscle aches and extreme exhaustion, impacting her ability to concentrate and meet deadlines. She proactively communicated with her employer, detailing her condition and seeking accommodations. These included adjusted work hours, a flexible work schedule, and ergonomic adjustments to her workstation.
Sarah also utilized a noise-canceling headset and a standing desk to manage her symptoms. Her employer, recognizing the value of her skills and commitment, was receptive to her requests. The result was a more sustainable work environment, allowing Sarah to continue contributing effectively to the team while managing her health needs.
Case Study 2: The Creative Teacher
Mark, a passionate art teacher, found that his creative work became increasingly difficult as his CFS worsened. The physical demands of lesson preparation, classroom management, and art projects were overwhelming. He communicated his situation to the school administration, emphasizing the need for adjusted responsibilities. Instead of reducing his overall teaching load, Mark suggested a focus on less physically demanding activities, like curriculum design and mentoring younger teachers.
This approach enabled him to maintain his role while significantly reducing the physical strain. He was supported with access to a quiet space for rest breaks and modifications to his teaching schedule. The result was a successful and fulfilling work experience for Mark and a more flexible approach for the school.
Case Study 3: The Tech Support Specialist
Emily, a skilled tech support specialist, found her job increasingly taxing as her FM progressed. The constant need for focus, problem-solving, and troubleshooting was difficult to maintain. She approached her manager to discuss possible accommodations. She requested a flexible work arrangement with specific breaks, allowing her to work in shorter bursts with more frequent rest periods. The company implemented a system where Emily could work remotely on days when in-person work was particularly challenging.
The arrangement allowed her to manage her workload more effectively and maintain her professional contributions. Emily’s proactive communication and the company’s understanding of her needs led to a positive outcome.
Case Study 4: The Customer Service Representative
David, a dedicated customer service representative, struggled with his job as his FM worsened. The constant interactions with customers, maintaining composure, and adhering to strict performance standards became progressively difficult. He discussed his condition with his supervisor and sought accommodations to alleviate these issues. He proposed adjusted work hours, prioritizing less demanding tasks, and utilizing a noise-canceling headset in the office.
His employer agreed to a modified workload, allowing David to focus on high-priority tasks and reduce interactions that were too strenuous. The modified schedule enabled David to maintain his employment while minimizing the impact of his symptoms.
Last Recap
In conclusion, maintaining employment with fibromyalgia and CFS is achievable with careful planning, proactive communication, and understanding of legal rights. The key is to find a work environment and strategies that support your unique needs. By understanding your condition, exploring flexible work options, developing effective symptom management techniques, and advocating for your rights, you can navigate the challenges and build a successful career.
Remember to seek professional support and guidance throughout the process.