What side effects can I expect after LASIK? This comprehensive guide dives into the potential short-term and long-term effects of laser eye surgery. From the initial recovery period to possible complications, we’ll explore the factors influencing outcomes and strategies for managing any issues that may arise. Understanding the risks and benefits of LASIK is crucial for informed decision-making.
LASIK, a popular vision correction procedure, involves reshaping the cornea to improve eyesight. While generally safe and effective, potential side effects exist, varying in severity and duration. This detailed exploration will help you navigate the complexities of LASIK recovery and make well-informed choices about your eye health.
Introduction to LASIK Side Effects
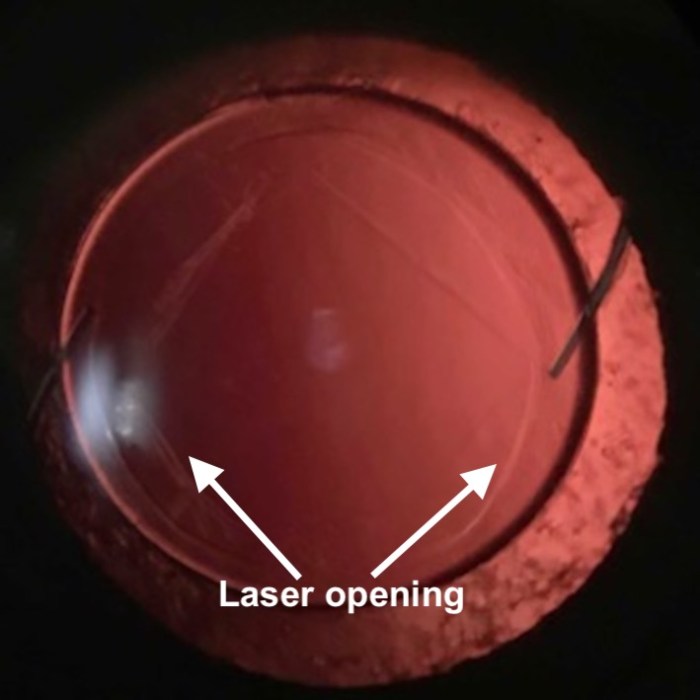
LASIK, or Laser-Assisted In Situ Keratomileusis, is a common refractive surgery procedure designed to correct nearsightedness, farsightedness, and astigmatism. It involves reshaping the cornea, the clear front part of the eye, using a laser to improve the eye’s focusing ability. This precise reshaping allows individuals to potentially reduce or eliminate their dependence on eyeglasses or contact lenses.The LASIK procedure typically involves several steps.
First, a small flap of corneal tissue is created. Then, the laser precisely removes corneal tissue to adjust its shape. Finally, the flap is repositioned to its original position. The procedure aims to precisely reshape the cornea to better focus light onto the retina, thereby improving vision. Variations in procedure types and techniques exist, each with its own nuances in the recovery process.
Types of LASIK Procedures
Different LASIK procedures are available, each with potential variations in the laser used, the flap creation method, and the amount of corneal tissue removed. The choice of procedure depends on individual eye characteristics and the specific correction needed. Understanding the nuances of these variations is important for anticipating potential side effects.
Potential Risks and Benefits of LASIK
LASIK, like any surgical procedure, carries potential risks and benefits. The benefits include improved vision, potentially eliminating the need for eyeglasses or contact lenses, and an overall enhancement of lifestyle. However, there are potential side effects that can range from mild to more severe, impacting the recovery period and potentially the long-term visual outcome.
Comparison of LASIK Procedure Types
| Procedure Type | Potential Benefits | Potential Risks | Recovery Time |
|---|---|---|---|
| Standard LASIK | Improved vision, reduced dependence on glasses/contacts, enhanced lifestyle | Dry eye, glare, halos, astigmatism, fluctuating vision, infection, flap complications | Typically 1-2 weeks, with full recovery within several months |
| Custom LASIK | Potential for more precise vision correction, potentially reducing the need for additional procedures | Similar to standard LASIK, but with potential for more pronounced side effects if not carefully performed | Similar to standard LASIK, though some individual experiences may vary |
| Epi-LASIK | Preserves the corneal epithelium, which can potentially reduce the risk of some side effects | Longer recovery time, potential for dry eye, and potentially higher risk of flap complications | Typically 2-4 weeks, with full recovery within several months |
| SMILE (Small Incision Lenticule Extraction) | Minimally invasive, potentially faster recovery, less risk of flap-related complications | Potential for dry eye, glare, halos, and fluctuating vision. Potential for complications like infection or irregular astigmatism. | Generally faster recovery compared to LASIK, with full recovery typically within a few weeks. |
Common Short-Term Side Effects
LASIK, while a transformative procedure, can bring about a range of temporary side effects. Understanding these common post-operative symptoms empowers patients to proactively manage them and ensures a smoother recovery journey. This section delves into the most frequent short-term effects, their causes, duration, and management strategies.
Common Symptoms and Their Causes
Many patients experience temporary discomfort following LASIK surgery. These symptoms, while often mild and temporary, are a natural response to the surgical procedure and the healing process. The most common causes include the incisions made during the procedure, the subsequent inflammation, and the body’s natural healing response. Dry eyes, for example, are a result of the disruption of the tear film and the subsequent reduction in tear production.
Duration of Short-Term Effects
The duration of these short-term side effects varies considerably, depending on the individual and the specific issue. Some symptoms, such as mild discomfort and blurry vision, may persist for a few days or weeks. Others, like dry eyes, might linger for a month or two. A doctor’s guidance on expected recovery times and individual symptom duration is crucial.
Severity of Short-Term Effects
| Symptom | Description | Severity Level (1-5, 1 being mildest) |
|---|---|---|
| Mild Eye Discomfort | Slight ache or pressure in the eyes | 2 |
| Blurry Vision | Reduced clarity of vision | 3 |
| Dry Eyes | Feeling of dryness, irritation, or foreign body sensation | 2-3 |
| Photophobia | Sensitivity to light | 2-4 |
| Eye Pain | Moderate to severe pain in the eyes | 4-5 |
This table offers a general guide to the severity of common short-term side effects. The severity levels are subjective and may vary between individuals. The severity of each effect should be assessed and monitored by an ophthalmologist.
Strategies for Managing Short-Term Effects
Managing these short-term effects involves a combination of prescribed eye drops, lifestyle adjustments, and, in some cases, over-the-counter pain relievers. Following your surgeon’s post-operative instructions precisely is vital. Taking regular breaks, maintaining proper hydration, and using prescribed eye drops as directed are essential strategies for mitigating discomfort.
List of Common Short-Term Effects and Duration
- Eye Discomfort: This may include a slight ache, pressure, or burning sensation. The discomfort usually subsides within a few days.
- Blurred Vision: Patients may experience blurry vision that gradually improves over a week or two.
- Dry Eyes: Dry eyes, characterized by dryness, irritation, and a foreign body sensation, often persist for a few weeks or even a month. This is a common complaint, and appropriate eye drops can help alleviate this.
- Photophobia: Sensitivity to light, or photophobia, can last for a few days or a couple of weeks. Protective eyewear might be needed during this time.
- Slight Eye Pain: Mild pain, often described as a dull ache, is a common occurrence and typically resolves within a few days. Using prescribed eye drops as directed is important.
Potential Long-Term Side Effects
While LASIK is generally a safe and effective procedure, potential long-term complications can arise. Understanding these possibilities is crucial for informed decision-making. This section delves into the potential long-term complications associated with LASIK, providing insight into their causes, likelihood, and variations across different surgical techniques.The long-term effects of LASIK can vary significantly from person to person. Factors such as individual eye health, the specific LASIK procedure, and post-operative care all contribute to the potential for complications.
It’s essential to remember that while these complications are possible, they don’t necessarily mean they will occur. Open communication with your eye surgeon about potential risks is vital.
Dry Eye Syndrome
Dry eye syndrome is a common post-LASIK complication. The procedure can alter the tear film’s production and distribution, leading to dryness, irritation, and discomfort. This condition often presents as a persistent feeling of dryness, itching, or a gritty sensation in the eyes.
Blurry Vision
Blurred vision, though typically temporary after LASIK, can sometimes persist or worsen over time. This can result from issues with the corneal flap or irregularities in the corneal surface post-surgery. Some individuals might experience blurry vision in certain lighting conditions or after extended periods of focusing on a task.
Post-LASIK, some temporary side effects like blurry vision and eye dryness are common. While I’m not a doctor, I’ve heard that similar discomfort can sometimes be related to underlying heart health issues, such as those detectable through coronary artery calcium scans. Thankfully, these are usually mild and short-lived. The good news is, most people experience a significant improvement in vision after the initial healing period.
Refractive Error Changes
Refractive errors like myopia (nearsightedness), hyperopia (farsightedness), and astigmatism can sometimes recur or change in severity after LASIK. These changes are often subtle, but they can necessitate further corrective procedures, such as additional LASIK surgery or the use of glasses or contact lenses. The reasons for this can vary from residual irregularities in the cornea to natural changes in the eye’s shape over time.
Potential Complications Related to Different LASIK Procedures
The specific LASIK procedure employed can influence the likelihood of experiencing certain long-term complications. For example, different techniques for creating the corneal flap or the use of different lasers might lead to varying outcomes.
Likelihood of Long-Term Complications
The likelihood of experiencing long-term side effects from LASIK varies depending on the individual and the procedure. Unfortunately, precise figures for these probabilities are difficult to provide. This is due to the wide range of factors that can influence the outcome, including the patient’s specific circumstances, the surgeon’s expertise, and the choice of surgical technique.
Table Comparing Likelihood of Long-Term Complications Across Different LASIK Procedures
| Long-Term Complication | Likelihood (Approximate)
|
Likelihood (Approximate)
|
|---|---|---|
| Dry Eye | Moderate | Moderate |
| Blurry Vision | Low | Very Low |
| Refractive Error Changes | Low | Very Low |
Note: This table provides a general comparison. Specific likelihoods can vary greatly depending on individual factors and surgical technique. Consult with an ophthalmologist for personalized information.
Factors Influencing Side Effects
LASIK, while a highly effective procedure, isn’t without potential side effects. Understanding the factors that can influence the likelihood and severity of these outcomes is crucial for both patients and surgeons. These factors range from pre-existing eye conditions to lifestyle choices and even the surgeon’s experience. This section delves into these influential aspects to provide a more comprehensive picture of the LASIK journey.Factors like patient health, age, lifestyle, surgeon skill, and even demographics play significant roles in shaping the LASIK experience.
A thorough understanding of these factors can help patients and surgeons anticipate potential issues and tailor the procedure to individual needs.
Patient Health Conditions
Pre-existing eye conditions significantly impact LASIK outcomes. Conditions like dry eye syndrome, corneal diseases, and glaucoma can either increase the risk of side effects or complicate the recovery process. For example, a patient with a history of severe dry eye may experience more pronounced post-operative discomfort and a slower healing time. Furthermore, certain medical conditions, such as diabetes, can affect the healing process.
It’s crucial for patients to disclose all pre-existing conditions to their surgeon to allow for personalized strategies and risk assessment.
Age and Lifestyle Choices
Age and lifestyle choices can also influence the success and safety of LASIK. Younger patients generally exhibit quicker healing times and greater adaptability to changes in vision. Conversely, older patients may experience slower recovery periods and a slightly increased risk of certain side effects. Lifestyle choices, including smoking, excessive alcohol consumption, and poor sleep habits, can also affect the healing process and overall outcome.
A patient’s commitment to a healthy lifestyle post-surgery can dramatically impact their recovery.
Surgeon Experience and Skill
The surgeon’s experience and skill level play a pivotal role in the outcome of LASIK. Experienced surgeons with a proven track record of successful procedures are more likely to deliver optimal results with fewer complications. Surgical techniques, the precision of the laser, and the surgeon’s ability to adapt to individual patient needs all contribute to the overall success of the procedure.
Choosing a qualified and experienced surgeon is a crucial decision for a positive LASIK experience.
So, you’re considering LASIK? While it’s generally a safe procedure, some temporary side effects are common, like blurry vision or dry eyes. Interestingly, maintaining good overall health, including adequate vitamin D intake, might play a role in the healing process. Knowing the differences between vitamin D2 and vitamin D3 could be beneficial for your recovery. For a deeper dive into the specifics of vitamin D2 versus vitamin D3, check out this resource: vitamin d two vs d three.
Ultimately, proper post-LASIK care, including following your eye doctor’s instructions, will significantly impact your recovery and minimize any lingering side effects.
Impact on Different Demographics
Different patient demographics may experience varying degrees of side effects. For instance, patients with certain ethnic backgrounds or those with specific eye shapes might be more prone to certain types of complications. Understanding these potential variations is essential for both the patient and the surgeon. Careful consideration of the individual needs and characteristics of each patient is key.
Impact of Various Factors on Side Effects
| Factor | Potential Influence on Side Effects | Examples |
|---|---|---|
| Pre-existing eye conditions (e.g., dry eye, glaucoma) | Increased risk of complications, prolonged recovery, or less favorable outcomes. | A patient with severe dry eye may experience more post-operative discomfort. |
| Age | Younger patients generally recover faster; older patients might experience slower healing. | A 20-year-old will likely recover quicker than a 50-year-old. |
| Lifestyle choices (e.g., smoking, alcohol, sleep) | May hinder the healing process and increase the risk of complications. | Smoking can impede the healing process. |
| Surgeon experience | Experienced surgeons are associated with lower complication rates. | Surgeons with extensive experience and proven track records. |
| Patient demographics (e.g., ethnicity, eye shape) | May influence the potential for certain side effects. | Variations in eye shape can impact the procedure’s success. |
Management and Treatment of Side Effects

Navigating the post-LASIK journey often involves managing various side effects. Understanding how to handle these issues, from mild discomfort to more serious concerns, is crucial for a smooth recovery and optimal visual outcomes. This section will provide practical strategies for managing both short-term and long-term side effects, outlining when professional medical attention is warranted.Successfully managing post-LASIK side effects involves a proactive approach.
Early intervention and adherence to post-operative instructions are vital for a positive outcome. This proactive strategy will ensure that you’re equipped to handle any potential challenges and achieve a successful vision restoration.
Strategies for Managing Common Short-Term Side Effects
Short-term side effects, often experienced in the days following LASIK, typically resolve on their own. Implementing effective management strategies can expedite the recovery process and minimize discomfort.
- Eye Drops: Following prescribed regimens for eye drops is essential. These drops help reduce inflammation, lubricate the eyes, and prevent infection. Examples include artificial tears, steroid eye drops, and antibiotic eye drops. The specific type and frequency of drops will vary depending on the individual’s needs and the severity of the side effects.
- Pain Management: Mild discomfort, such as eye pain or itching, can be managed with over-the-counter pain relievers like acetaminophen. However, consult your ophthalmologist if pain is severe or persistent. Applying cool compresses to the affected area can also provide relief.
- Rest and Avoiding Strenuous Activities: Giving your eyes ample rest and avoiding strenuous activities is crucial. This includes limiting activities that could strain your eyes, such as prolonged screen time or intense physical exertion.
- Protecting Your Eyes: Avoid rubbing your eyes, and wear protective eyewear when outdoors to shield them from dust and debris. This is particularly important in the initial recovery phase.
Methods for Addressing Long-Term Side Effects
While most LASIK side effects are temporary, some long-term issues can arise. Addressing these requires a more nuanced approach, often involving further medical intervention.
- Dry Eye Syndrome: If dry eye syndrome persists or worsens, your ophthalmologist may prescribe different types of eye drops, such as punctal plugs, or recommend other therapies, including humidifiers or lifestyle adjustments.
- Astigmatism or Blurred Vision: In some cases, astigmatism or persistent blurred vision can be addressed with a touch-up LASIK procedure or other corrective measures. It is crucial to schedule follow-up appointments to assess the effectiveness of the treatment.
- Persistent Pain or Discomfort: If persistent pain or discomfort continues despite initial management strategies, it’s crucial to seek medical attention immediately. This is essential to rule out any underlying issues and determine the most appropriate course of action.
When to Seek Medical Attention
Recognizing when to seek medical attention is critical for managing potential complications. Prompt intervention can prevent the worsening of side effects.
- Severe Pain or Increased Sensitivity to Light: If you experience intense pain, increased sensitivity to light, or a sudden change in vision, consult your ophthalmologist immediately. These symptoms could indicate a more serious problem requiring immediate attention.
- Vision Deterioration: Any significant deterioration in vision, including persistent blurring or double vision, should prompt a prompt visit to your ophthalmologist.
- Signs of Infection: Symptoms such as redness, swelling, excessive tearing, or discharge from the eyes could signal an infection. Prompt medical attention is crucial in these situations.
Available Treatments for Specific Side Effects
Various treatments are available to address specific LASIK side effects.
| Side Effect | Potential Treatments |
|---|---|
| Dry Eye | Prescription eye drops, punctal plugs, humidifiers, lifestyle modifications |
| Persistent Blurred Vision | Retreatment, or other vision correction procedures |
| Infection | Antibiotic eye drops, oral antibiotics |
Post-Operative Care
Adhering to post-operative care instructions is essential for a smooth recovery.
- Follow-up Appointments: Regular follow-up appointments are crucial for monitoring your recovery and addressing any concerns.
- Hygiene Practices: Maintaining good hygiene practices, such as avoiding touching your eyes and washing your hands frequently, is vital.
- Medication Adherence: Strictly follow the prescribed medication regimen to manage inflammation and prevent infection.
Flowchart for Managing Side Effects
This flowchart illustrates the steps to take if side effects arise:[Diagram of a flowchart illustrating the steps to take if side effects arise. The flowchart should include steps such as assessing the severity of the side effect, contacting the ophthalmologist, following prescribed treatments, and scheduling follow-up appointments. The flowchart should be visually clear and easy to understand. The flowchart should also clearly indicate when to seek emergency medical attention.]
Illustrative Cases of Side Effects
LASIK, while a highly effective procedure, can sometimes result in unexpected side effects. Understanding these potential complications is crucial for both patients and surgeons. This section delves into real-world examples of side effects, highlighting the initial symptoms, treatment approaches, and ultimate outcomes. These case studies aim to provide a realistic perspective on the recovery process and the management of LASIK complications.
Case Study: Persistent Dry Eye
Persistent dry eye is a common post-LASIK complaint. Patients often experience a gritty or sandy sensation in their eyes, along with increased tearing and discomfort. The discomfort can significantly impact daily activities, especially those requiring prolonged periods of screen time.A patient named Sarah, following her LASIK procedure, reported persistent dry eye symptoms. Initially, she used over-the-counter lubricating eye drops, but the discomfort persisted.
So, you’re considering LASIK? It’s a pretty cool procedure, but what about potential side effects? Well, temporary blurry vision, dry eyes, and even some discomfort are common. But, hey, maybe you could burn off some of those recovery jitters with some unusual ways to burn calories! Check out some creative ideas on how to stay active and healthy while you recover here.
Ultimately, though, remember that the specifics of post-LASIK side effects vary from person to person, so it’s always best to talk to your doctor.
Her ophthalmologist then prescribed a combination of artificial tears and a punctal plug, a small device inserted into the tear duct to reduce tear evaporation. The punctal plug proved effective, and Sarah’s dry eye symptoms gradually subsided within a few months.
Case Study: Astigmatism Recurrence
Post-LASIK, some patients may experience a recurrence of astigmatism, an imperfection in the eye’s shape that causes blurred vision. This recurrence can manifest as a gradual or sudden change in vision quality.One patient, David, experienced a slight increase in astigmatism after his LASIK procedure. His initial vision improvement was noticeable, but over several months, he began experiencing a progressive blurring of vision.
David consulted his ophthalmologist, who performed a comprehensive eye exam and determined the need for a corrective lens procedure to address the recurred astigmatism. Following the additional procedure, David regained clear vision and experienced long-term stability.
Case Study: Rare Corneal Scarring
Although uncommon, corneal scarring can sometimes occur after LASIK. This condition may present as persistent blurry vision, pain, and light sensitivity. Early diagnosis and appropriate intervention are crucial for preventing vision loss.A patient, Emily, experienced a rare case of corneal scarring after LASIK. Initial symptoms included persistent blurry vision, discomfort, and increased sensitivity to light. The ophthalmologist immediately initiated a course of topical medications and closely monitored Emily’s eye condition.
Fortunately, with careful management and follow-up care, the scarring resolved, and Emily’s vision gradually improved.
Table of Case Studies Demonstrating Various LASIK Side Effects
| Patient | Side Effect | Initial Symptoms | Treatment | Resolution/Management |
|---|---|---|---|---|
| Sarah | Persistent Dry Eye | Gritty, sandy sensation; increased tearing | Artificial tears, punctal plug | Symptoms subsided within months |
| David | Astigmatism Recurrence | Gradual blurring of vision | Corrective lens procedure | Regained clear vision |
| Emily | Corneal Scarring | Blurry vision, discomfort, light sensitivity | Topical medications, close monitoring | Scarring resolved, vision improved |
Comparison with Other Vision Correction Procedures: What Side Effects Can I Expect After Lasik
Choosing the right vision correction procedure can be daunting, as each method comes with its own set of potential benefits and drawbacks. Understanding the nuances of different techniques, like LASIK, PRK, and LASEK, is crucial for making an informed decision. This comparison delves into the potential side effects, recovery times, and overall advantages and disadvantages of each procedure.
LASIK vs. PRK vs. LASEK: A Side-by-Side Look
LASIK, PRK, and LASEK are all refractive surgical procedures designed to improve vision. However, they differ significantly in their approach, which translates to variations in potential side effects and recovery times. Understanding these differences can help you decide which procedure is most appropriate for your individual needs.
Similarities and Differences in Potential Side Effects
While all three procedures aim to reshape the cornea, the method of doing so varies. This difference in approach leads to variations in the types and severity of potential side effects. For instance, LASIK involves a flap creation, which might lead to some flap-related complications. PRK, on the other hand, removes the surface layer of the cornea directly, potentially causing more discomfort during the healing process.
LASEK uses an epithelial shield, potentially reducing some of the pain associated with PRK.
Recovery Time Considerations
The recovery period for each procedure also differs significantly. LASIK typically involves a quicker recovery compared to PRK and LASEK. The timeframe for complete recovery and achieving optimal vision varies, depending on the individual and the procedure. PRK generally requires a longer healing period than LASIK, and LASEK often falls somewhere in between. Patients should expect some degree of discomfort and potential visual disturbances during the recovery period.
Advantages and Disadvantages Table
| Procedure | Potential Side Effects (Summary) | Recovery Time (General Estimate) | Advantages | Disadvantages |
|---|---|---|---|---|
| LASIK | Dry eye, glare, halos, fluctuating vision, flap complications | Generally quicker (few days to weeks) | Faster recovery, potentially less discomfort during healing | Risk of flap complications, slightly higher risk of dry eye |
| PRK | Significant pain and discomfort during healing, potential for infection, blurred vision, dry eye | Longer recovery (several weeks) | Potential for better long-term vision outcomes in some cases | More intense pain and discomfort, longer recovery period |
| LASEK | Less pain than PRK, some risk of infection, dry eye, blurry vision, halos | Intermediate recovery time (several weeks) | Less intense pain than PRK, potentially quicker recovery than PRK | Still requires a healing period, risk of infection |
Important Note: This table is for general guidance only. Individual experiences and outcomes may vary. Consult with a qualified ophthalmologist for a personalized assessment and to discuss the best course of action for your specific needs.
Prevention Strategies

Minimizing the risk of LASIK side effects is paramount. Proactive steps, from meticulous pre-operative preparation to vigilant post-operative care, significantly influence the likelihood and severity of complications. A proactive approach, coupled with a well-informed decision about choosing an experienced surgeon, dramatically enhances the chances of a smooth recovery and optimal vision outcomes.
Selecting a Qualified Surgeon
Choosing an experienced and qualified LASIK surgeon is crucial. Researching a surgeon’s credentials, experience, and track record is essential. Look for surgeons with board certifications, extensive experience performing LASIK procedures, and a proven history of positive patient outcomes. A surgeon’s familiarity with the specific technology used in the procedure is also critical. Consult with multiple surgeons, discuss your concerns, and select the professional who best aligns with your needs and expectations.
Reviews from other patients can also offer valuable insights.
Maintaining Good Eye Health
Prioritizing good eye health before and after LASIK surgery is essential. Maintaining a healthy lifestyle with a balanced diet, regular exercise, and sufficient sleep can contribute to a quicker recovery and better outcomes. Proper hydration, reducing exposure to irritants like smoke and allergens, and avoiding eye rubbing are crucial. Consistent eye examinations, even after surgery, are vital for early detection and treatment of any potential issues.
Managing underlying eye conditions, such as dry eye, before and after surgery, is a critical aspect of pre and post-operative care.
Pre- and Post-Operative Care Checklist, What side effects can i expect after lasik
Adherence to pre- and post-operative instructions is critical for a successful recovery. This includes diligently following the surgeon’s pre-operative guidelines regarding medications, eye drops, and lifestyle adjustments. Strict adherence to post-operative care instructions, such as the use of prescribed eye drops, avoiding strenuous activities, and attending follow-up appointments, are equally important. A thorough understanding and meticulous adherence to these instructions can significantly minimize the risk of complications.
- Pre-operative Care: This involves abstaining from certain medications, maintaining good hydration, and ensuring a comprehensive eye examination to identify any pre-existing conditions.
- Post-operative Care: This includes using prescribed eye drops meticulously, protecting the eyes from dust and irritants, and avoiding strenuous activities as directed by the surgeon.
Stress Management
Stress and anxiety can negatively impact the healing process. Employing stress-reduction techniques like meditation, yoga, or deep breathing exercises can significantly contribute to a smoother recovery. Adequate rest and a positive mindset are essential for optimal healing. Identifying and managing stress triggers before and after surgery can be a significant factor in a successful recovery.
- Techniques for Stress Management: Employing stress-reducing techniques like meditation, yoga, or deep breathing exercises can promote a smoother recovery.
- Importance of a Positive Mindset: A positive and proactive approach to the procedure can facilitate a better healing process and minimize stress and anxiety.
Preventative Measures Checklist
This checklist Artikels proactive measures to reduce LASIK side effects:
| Category | Action |
|---|---|
| Pre-operative |
|
| Post-operative |
|
| Lifestyle |
|
Closing Summary
In conclusion, LASIK, while a remarkable procedure, carries potential side effects that vary significantly between individuals. Understanding the possible short-term and long-term complications, along with factors influencing them, empowers you to make informed decisions and choose the best course of action. Careful consideration of these aspects, alongside the expertise of a qualified surgeon, will significantly enhance your chances of a successful and satisfying LASIK experience.