Bug bite on eyelid: A frustrating and sometimes painful experience. This comprehensive guide delves into the intricacies of identifying, treating, and preventing these irritating bites around the delicate eye area. We’ll explore the various insects that might be the culprit, how to differentiate between a simple bite and more serious reactions, and what first-aid steps to take at home.
Understanding the potential causes and knowing when to seek medical attention are crucial aspects of effectively managing a bug bite on the eyelid.
From pinpointing the specific insect to navigating the steps for effective home remedies, this guide covers all the essential information to help you better understand and handle bug bites on your eyelid. Learn to recognize the tell-tale signs and symptoms, differentiate them from other skin conditions, and take the necessary precautions to avoid future incidents.
Identifying the Issue
A bug bite on the eyelid, while often a minor inconvenience, can sometimes be a sign of something more serious. Understanding the characteristics of these bites, as well as distinguishing them from other skin conditions, is crucial for proper self-care and, when necessary, seeking professional medical advice. This section will delve into the various aspects of eyelid bug bites, offering detailed descriptions, comparisons, and examples to aid in identification.Eyelid bug bites often manifest with distinctive features.
Identifying these characteristics is important for differentiating them from other skin irritations. A precise understanding of these features, combined with knowledge of potential underlying causes, can lead to effective self-management and, when required, prompt medical intervention.
That pesky bug bite on my eyelid is driving me crazy! It’s so itchy and swollen. I’ve been doing some research on natural remedies, and I came across an interesting article about whether garlic can help lower blood pressure. Does garlic lower blood pressure ? While I’m not sure if it’ll help my eyelid situation, it’s certainly a fascinating topic.
I’m hoping some cool compresses and maybe a little bit of time will soothe this irritating bug bite.
Typical Characteristics of a Bug Bite on the Eyelid
Bug bites on the eyelids typically present as small, raised bumps or welts. The size can vary, ranging from a few millimeters to a centimeter or more in diameter. The shape is often round or oval, but can also appear irregular. Coloration can range from red to pinkish-red, and in some cases, a slight discoloration or darkening might occur.
Associated symptoms can include itching, swelling, and mild to moderate pain. The severity of these symptoms varies greatly depending on the individual and the type of insect.
That annoying bug bite on my eyelid is driving me crazy! It’s itchy and swollen, and honestly, I’m starting to wonder if it’s related to anything more serious. Sometimes, when you have a fever, there are worries about potential brain damage, which is why I’m curious about do fevers cause brain damage. But for now, I’m just going to focus on soothing this eyelid irritation.
Hopefully, a cool compress will do the trick!
Differences Between Bug Bites and Other Skin Conditions
It’s crucial to distinguish bug bites from other skin conditions that may mimic their appearance. Allergic reactions, for instance, can manifest as hives or welts on the eyelid, potentially accompanied by other symptoms like difficulty breathing or a rapid heartbeat. Infections, such as bacterial or viral infections, can also cause swelling and redness, often accompanied by pus or other discharge.
A thorough understanding of the specific symptoms and their progression is key to differentiating between these conditions. A doctor can provide accurate diagnoses.
Types of Insects and Their Bites
Several insects can bite around the eyes. Mosquitoes, for example, typically leave small, itchy red bumps. Flies, including houseflies, can also bite, often causing a localized reaction with redness and mild swelling. Bed bugs may cause a more significant reaction, marked by multiple bites in a clustered pattern and severe itching. Fleas can cause similar reactions, often in a clustered pattern, while also potentially causing more widespread discomfort.
The specific symptoms will depend on the type of insect.
Common Locations on the Eyelid
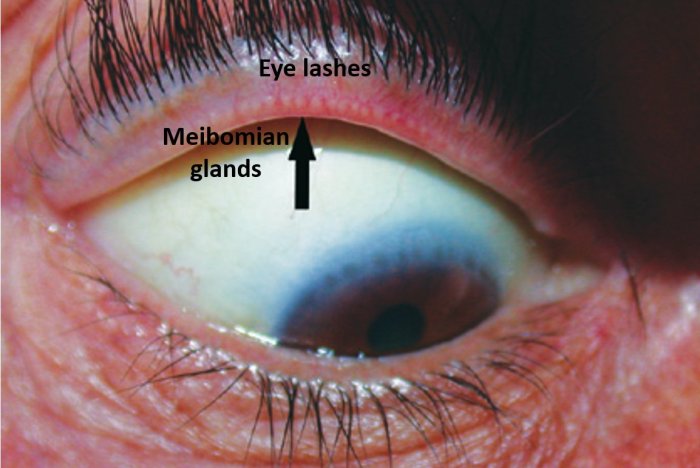
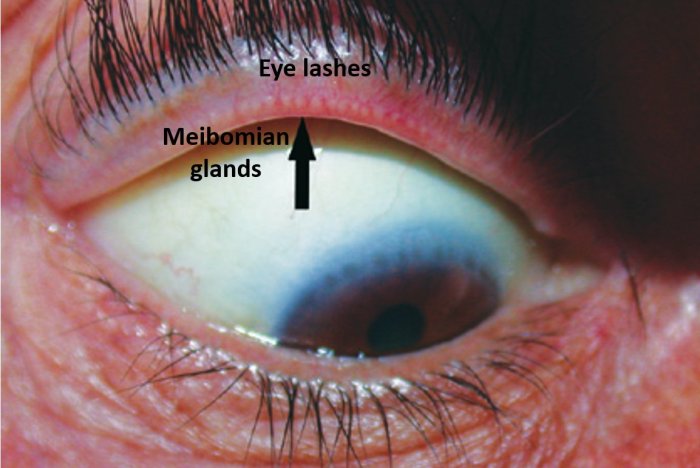
Bug bites on the eyelid are often found near the eyelashes, along the crease of the eyelid, or on the skin surrounding the eye. The proximity to the delicate skin around the eye necessitates careful consideration and management to avoid further irritation or discomfort.
Comparison of Insect Bites
| Insect | Typical Appearance | Common Associated Symptoms |
|---|---|---|
| Mosquito | Small, red, itchy bump | Itching, slight swelling |
| Fly | Small, red, raised bump | Mild itching, localized redness |
| Bed Bug | Multiple small red bites, often in a line | Intense itching, potential for skin irritation, welts |
| Fleas | Multiple small red bites, often in a cluster | Itching, potential for skin irritation, welts |
Potential Causes
A bug bite on the eyelid, though often seemingly minor, can have various underlying causes. Understanding these factors is crucial for effective treatment and preventing complications. Proper identification of the culprit is vital for appropriate management and avoidance of potentially serious reactions.
Common Insects and Their Biting Habits
Many insects are known to bite humans. Some of the most common culprits include mosquitoes, bed bugs, fleas, and ants. While these insects can bite anywhere on the body, the eyelid’s delicate skin and proximity to the eye make it a potential target. Mosquito bites are particularly common, often resulting in a red, itchy bump. Bed bugs, while less likely to target the eyelid directly, can sometimes cause localized reactions.
Fleas, primarily a concern for pets, can sometimes bite humans, potentially causing a reaction on the eyelid.
Role of Allergies in Insect Bites
Allergies play a significant role in the severity of reactions to insect bites. A person with an allergy to insect venom or saliva may experience a more pronounced and potentially dangerous reaction compared to someone without an allergy. Symptoms can range from mild swelling and itching to more severe reactions, such as hives, difficulty breathing, or anaphylaxis. In such cases, prompt medical attention is crucial.
Potential for Secondary Infections
A bug bite on the eyelid, if scratched or left untreated, can increase the risk of secondary infections. Bacteria on the skin can enter the bite wound, leading to inflammation, pain, and potential complications. The close proximity of the eye increases the risk of spreading infection to the surrounding tissues, which can cause serious damage to the eye.
Careful hygiene and avoiding scratching are essential to prevent such infections.
Distinguishing Simple Bites from Serious Conditions
It is important to distinguish between a simple bug bite and more serious conditions such as an allergic reaction or infection. A simple bug bite typically presents as a small, red, itchy bump. Allergic reactions can manifest as widespread hives, swelling, and difficulty breathing. Infections may show signs of increased redness, swelling, pus formation, or persistent pain.
Any deviation from a simple bug bite warrants prompt medical evaluation.
Summary Table of Potential Causes
| Potential Cause | Typical Characteristics |
|---|---|
| Simple bug bite (e.g., mosquito, flea) | Small, red, itchy bump; localized swelling; mild discomfort |
| Allergic reaction to insect bite | Widespread hives; significant swelling; difficulty breathing; itching; possible anaphylaxis (severe allergic reaction) |
| Secondary infection | Increased redness; pus formation; persistent pain; significant swelling around the bite site; fever |
| Other conditions (e.g., eczema, dermatitis) | Symptoms may be similar to bug bites, but may exhibit other features like scaling, dryness, or patterns; may occur without a clear bite mark |
First Aid and Home Remedies
A bug bite on the eyelid can be incredibly irritating and uncomfortable. Prompt and appropriate first aid can significantly reduce the severity and duration of symptoms. Understanding how to treat these bites effectively is crucial for minimizing discomfort and preventing complications.Effective first aid for a suspected bug bite on the eyelid involves a multi-faceted approach. This includes immediate actions to manage the initial reaction, application of soothing remedies, and precautions to prevent further irritation.
Applying these strategies will help alleviate pain, reduce swelling, and encourage faster healing.
Step-by-Step Procedure for Treating a Suspected Bug Bite
This step-by-step guide Artikels the process for managing a bug bite on the eyelid:
- Immediately wash the affected area gently with mild soap and water. This helps remove any potential irritants or contaminants from the bite site.
- Apply a cold compress to the eyelid. This helps reduce swelling and pain. Hold the compress against the area for 10-15 minutes at a time, repeating as needed. The compress should not be overly cold to avoid causing further discomfort.
- Avoid scratching the affected area. Scratching can introduce bacteria and further irritate the skin, potentially leading to infection.
- If the itching persists, consider using an over-the-counter antihistamine cream or oral medication. Consult a doctor if symptoms worsen or do not improve.
- Monitor the area for any signs of infection, such as increased redness, swelling, pus, or fever. If these symptoms appear, seek medical attention immediately.
Comparison of Home Remedies
Different home remedies can offer varying degrees of relief for bug bite symptoms.Cold compresses are a widely used and effective home remedy for reducing swelling and pain. The application of a cold compress provides immediate relief by constricting blood vessels, thus decreasing the blood flow to the area and reducing inflammation.Over-the-counter antihistamines can help alleviate itching and other allergic reactions.
These medications work by blocking the effects of histamine, a chemical released by the body in response to an allergic reaction. Antihistamines can be applied topically as creams or taken orally.A simple comparison of these two remedies highlights their individual benefits:
| Remedy | Benefits | Limitations |
|---|---|---|
| Cold Compress | Immediate pain relief, reduces swelling | Limited effect on itching, may not address underlying allergy |
| Over-the-counter Antihistamine | Effective against itching, allergic reactions | May not provide immediate pain relief, requires time for medication to take effect |
Importance of Avoiding Scratching
Scratching a bug bite on the eyelid can lead to significant complications. Scratching introduces bacteria into the open wound, potentially leading to infection and further irritation. This can prolong healing and increase the risk of complications. It is crucial to resist the urge to scratch, as this can worsen the condition.
That annoying bug bite on my eyelid is driving me crazy! It’s itchy and swollen, and honestly, I’m starting to wonder if it’s affecting my TMJ. I’ve been doing some research and stumbled upon a great exercise program for TMJ and TMD pain that might help alleviate some of the discomfort. Maybe incorporating some of the exercises from this program exercise program for tmd and tmj pain could help with the pressure in my jaw.
I’ll definitely be trying a few of these to see if they help ease the pressure around my jaw and, hopefully, reduce the irritation from the bug bite. Fingers crossed!
Soothing Home Remedies Ingredients
A variety of ingredients can be used to create soothing home remedies for bug bites. Some effective ingredients include:
- Aloe vera gel: Known for its soothing and anti-inflammatory properties. The gel can be applied directly to the affected area to reduce itching and swelling.
- Baking soda paste: A paste made with baking soda and water can help neutralize the acids produced by the body’s reaction to the bite.
- Cucumber slices: The cooling effect of cucumber slices can help soothe the irritated skin and reduce inflammation.
- Oatmeal: Oatmeal baths or compresses can help reduce itching and inflammation. Oatmeal can be a soothing ingredient for a variety of skin irritations.
Proper Application of Cold Compresses
Applying a cold compress correctly is essential for maximizing its effectiveness in reducing swelling and pain.
- Use a clean cloth or a cold compress, such as a reusable gel pack.
- Wrap the compress in a clean cloth to avoid direct contact with the skin.
- Apply the compress to the affected area for 10-15 minutes at a time.
- Remove the compress and allow the skin to rest for a few minutes before reapplying.
- Repeat the process as needed.
When to Seek Medical Attention
A bug bite on the eyelid, while often manageable with home remedies, can sometimes indicate a more serious issue. Knowing when to seek medical attention is crucial to ensure prompt and effective treatment, preventing potential complications. This section will Artikel the situations where immediate medical care is necessary, the symptoms that signal a serious reaction, and the importance of professional medical advice.
Serious Reactions and Symptoms Requiring Immediate Medical Attention
Recognizing the signs of a severe allergic reaction or infection is paramount. Delayed treatment can lead to complications, including vision problems or permanent scarring. Prompt medical attention is vital in such cases.
Symptoms Warranting Immediate Medical Attention
Certain symptoms necessitate immediate medical attention. These include severe swelling, intense pain, redness spreading beyond the bite site, difficulty opening the eye, blurred vision, or signs of an infection, such as pus or a thick discharge. These symptoms often signal a more serious reaction requiring medical intervention.
Table of Symptoms Requiring Immediate Medical Attention
| Symptom | Description |
|---|---|
| Severe Swelling | Significant puffiness around the eye, making it difficult to open or see clearly. |
| Intense Pain | Pain that is significantly worse than expected for a bug bite, throbbing, or sharp. |
| Redness Spreading Beyond Bite Site | Redness expanding outward from the bite, involving more of the eyelid or surrounding skin. |
| Difficulty Opening the Eye | Inability to open the eye fully due to swelling or pain. |
| Blurred Vision | Loss of clarity or sharpness in vision. |
| Signs of Infection (Pus or Thick Discharge) | Presence of pus, thick yellow or green discharge, or a noticeable drainage from the bite site. |
| Hives or Rash | Appearance of itchy welts or a widespread rash beyond the immediate bite area. |
| Difficulty Breathing or Dizziness | Respiratory distress or lightheadedness, possibly indicating a systemic allergic reaction. |
Potential Complications of Untreated Bug Bites on the Eyelid
Untreated bug bites on the eyelid can lead to various complications. These can include persistent swelling, infection, scarring, and, in rare cases, vision impairment. The severity of these complications often correlates with the severity of the initial reaction and the delay in seeking professional medical advice. It is crucial to address any concerning symptoms promptly to minimize the risk of these complications.
Prevention Strategies

Protecting your delicate eye area from pesky bug bites is crucial for maintaining comfort and avoiding potential complications. Proactive measures can significantly reduce your risk of encountering these unwelcome encounters. By understanding the habits and breeding grounds of insects, and employing effective preventative strategies, you can minimize the chances of a bug bite on your eyelid.
Measures to Prevent Bug Bites Around the Eyes
Preventing bug bites around the eyes involves a multi-faceted approach. A combination of personal habits and environmental modifications can significantly decrease the likelihood of these encounters.
- Apply insect repellent: Use a repellent containing DEET or picaridin, applied liberally to exposed skin, following the product instructions. Ensure the repellent is safe for use around the eyes, as some products may irritate sensitive skin. Re-apply as needed, especially after sweating or swimming.
- Wear protective clothing: Opt for long sleeves and pants when spending time outdoors, especially during peak biting hours. Light-colored clothing can make it easier to spot insects before they land on your skin.
- Eliminate insect breeding grounds: Regularly empty standing water around your home, such as flowerpots, birdbaths, and clogged gutters. These stagnant water sources are prime breeding grounds for mosquitoes and other biting insects.
- Check for bugs near your face: Before entering an area known for insects, or when spending time outdoors, routinely inspect your face for any crawling insects. This simple step can prevent a bite before it occurs.
Importance of Protective Clothing
Protecting your skin with appropriate clothing, especially when spending time outdoors, significantly reduces your exposure to insect bites. The use of protective clothing acts as a physical barrier, preventing insects from accessing your skin.
- Long sleeves and pants: These items of clothing provide a physical barrier, shielding exposed skin from insects. This is particularly important when spending time in wooded areas or near bodies of water.
- Light-colored clothing: Light-colored clothing makes it easier to spot insects on your skin, allowing you to take action before they bite.
- Hats and head coverings: Head coverings, like hats or bandanas, can provide extra protection for your face and scalp, further reducing the risk of bites.
Methods to Eliminate Insect Breeding Grounds
Maintaining a clean and sanitary environment around your home helps disrupt the life cycle of insects and minimize their presence. By eliminating potential breeding grounds, you decrease the likelihood of encountering insects.
- Empty standing water: Regularly empty any standing water sources around your home, such as flower pots, pet dishes, and discarded containers. Mosquitoes and other insects breed in stagnant water. This simple step can significantly reduce the local insect population.
- Maintain gutters and drains: Ensure that gutters and drains are clear of debris, preventing water from accumulating. Clogged gutters can lead to water pooling, providing a breeding ground for insects.
- Trim vegetation: Keep vegetation around your home trimmed and well-maintained. This reduces hiding places and breeding grounds for insects.
Insect Repellent Comparison, Bug bite on eyelid
Various insect repellents are available, each with its own active ingredients and effectiveness. The effectiveness of a repellent often depends on the specific insect and the environment.
| Repellent | Active Ingredient | Effectiveness | Considerations |
|---|---|---|---|
| DEET | N,N-Diethyl-meta-toluamide | Generally effective against a wide range of insects | Can be irritating to skin for some individuals. |
| Picaridin | Picaridin | Generally effective against a wide range of insects | Generally considered less irritating than DEET. |
| Oil of lemon eucalyptus | Oil of lemon eucalyptus | Effective against mosquitoes, but may not be as effective against other insects | Not recommended for use on children under 3 years old. |
Regular Bug Checks Near the Face
Regularly checking your face for insects, especially in areas prone to insect activity, is a crucial preventative measure.
- Routine inspections: Before entering an area known for insects, or when spending time outdoors, check your face for insects.
- Increased vigilance: Pay close attention to areas where insects tend to gather, such as around your hair, ears, and neck. Early detection and removal are essential to prevent bites.
Final Conclusion: Bug Bite On Eyelid
In conclusion, dealing with a bug bite on the eyelid can be tricky, but understanding the potential causes, symptoms, and treatment options is key. This guide has provided a thorough overview, from identifying the culprit to applying effective first aid and knowing when professional help is needed. Remember, prevention is crucial. By taking the necessary precautions and knowing how to react quickly, you can minimize discomfort and ensure a speedy recovery.