Treatments for essential thrombocythemia are multifaceted, encompassing a range of pharmacological and non-pharmacological interventions tailored to individual patient needs. This in-depth exploration covers everything from the basics of essential thrombocythemia (ET) to emerging treatments and long-term management strategies. Understanding the nuances of ET and its various treatment approaches is crucial for patients and healthcare providers alike.
Essential thrombocythemia, characterized by abnormally high platelet counts, requires careful management to prevent potential complications. This guide delves into the different treatment modalities, examining their mechanisms of action, potential side effects, and effectiveness across diverse patient populations. We will also discuss crucial aspects like monitoring during treatment, long-term management, and the role of emerging therapies.
Overview of Essential Thrombocythemia (ET)
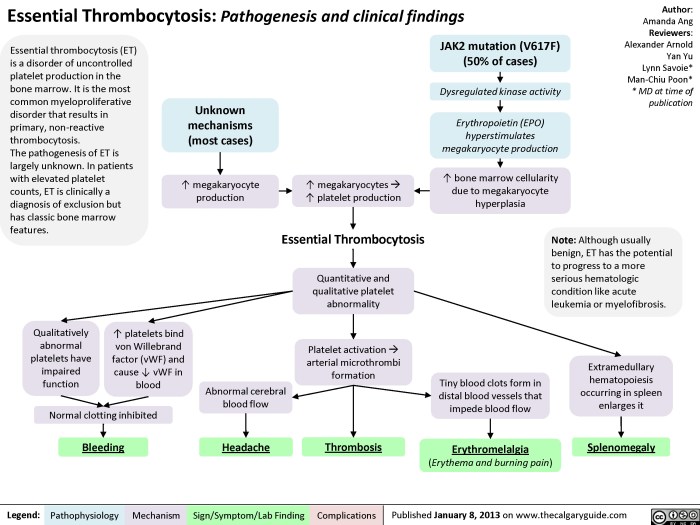
Essential thrombocythemia (ET) is a chronic myeloproliferative neoplasm characterized by a sustained increase in the number of platelets in the blood. It’s a relatively rare condition, often diagnosed in middle-aged adults, and requires careful management to prevent potentially serious complications. Understanding its features, symptoms, diagnosis, and risk factors is crucial for effective patient care.This condition arises from a genetic abnormality in the bone marrow, leading to an uncontrolled production of platelets.
This overproduction can disrupt normal blood function, increasing the risk of blood clots and bleeding episodes. While often manageable with appropriate treatment, ET necessitates long-term monitoring and potentially life-long management to minimize complications.
Key Features and Characteristics of ET
Essential thrombocythemia is fundamentally characterized by elevated platelet counts. This is the primary and defining feature, distinguishing it from other blood disorders. Other crucial characteristics include the presence of megakaryocyte hyperplasia (increased production of platelet-producing cells in the bone marrow), and the absence of significant changes in other blood cell lines (red blood cells and white blood cells).
Understanding these features helps in differentiating ET from similar conditions.
Typical Symptoms and Signs
The symptoms of ET can vary significantly among individuals. Some patients experience no noticeable symptoms, while others report a range of signs and symptoms. Commonly reported symptoms include headaches, dizziness, visual disturbances, fatigue, and a tendency toward bleeding or bruising. Other potential symptoms include pain in the hands and feet (especially at night), and in some cases, an increased risk of blood clots leading to symptoms like chest pain, shortness of breath, or stroke.
It’s crucial to note that not all individuals will exhibit these symptoms, and the severity can fluctuate.
Treating essential thrombocythemia often involves managing the high platelet count. While the specifics vary, some treatments focus on reducing platelet production. Interestingly, understanding the intricate anatomy of the frontal bone, as explored in this helpful resource on frontal bone anatomy function and treatment , can sometimes provide insights into other bone marrow-related conditions. Ultimately, the best approach to essential thrombocythemia treatment depends on individual patient factors.
Diagnostic Criteria and Procedures
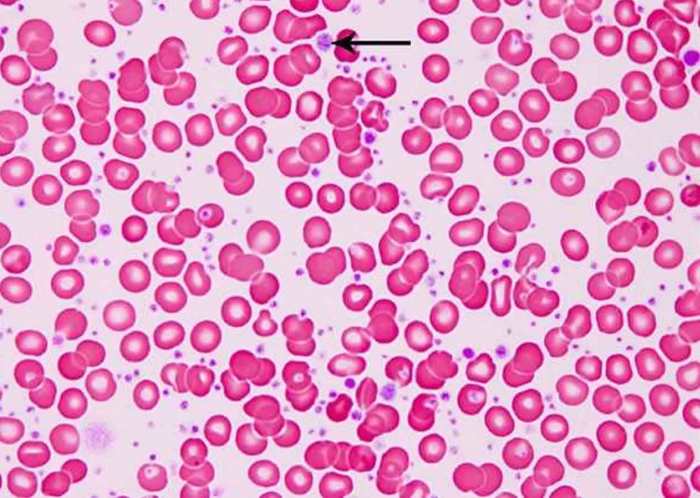
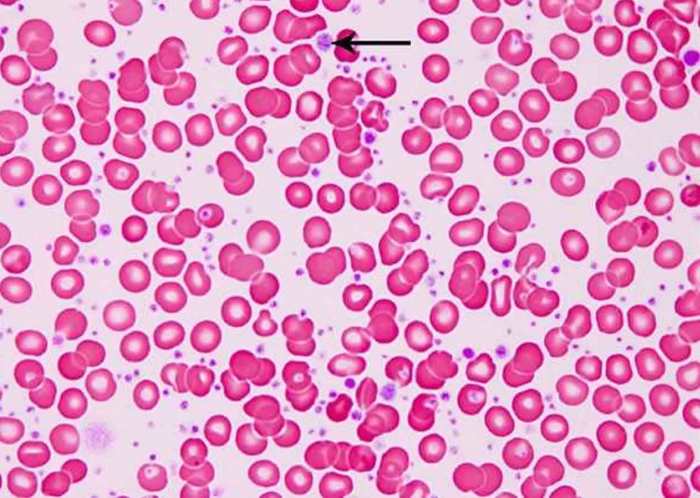
Diagnosis of ET relies on a combination of clinical evaluation, blood tests, and bone marrow examination. A complete blood count (CBC) is typically the first step, revealing an elevated platelet count. Further investigations may include a peripheral blood smear analysis, looking for specific platelet morphology characteristics, and a bone marrow biopsy to assess the cellularity and identify megakaryocyte hyperplasia.
Specific genetic testing, such as for JAK2 mutations, is also frequently performed to aid in the diagnosis and understanding of the disease’s underlying mechanisms. The presence of these characteristics helps to distinguish ET from other conditions with similar symptoms.
Common Risk Factors or Predisposing Conditions
While the precise cause of ET remains largely unknown, several factors are associated with an increased risk of developing the condition. Age is a significant factor, with most cases diagnosed in middle-aged adults. Family history of ET or other myeloproliferative neoplasms can also be a contributing factor. Additionally, exposure to certain environmental factors, although not definitively established, may potentially play a role in the development of ET.
It’s essential to consult with healthcare professionals for personalized advice on risk factors and preventive measures.
Treatment Approaches for ET: Treatments For Essential Thrombocythemia
Essential thrombocythemia (ET) necessitates a multifaceted approach to treatment, aiming to reduce the risk of thrombotic events while minimizing the potential for adverse effects. A personalized treatment plan is crucial, taking into account individual patient characteristics, disease severity, and risk factors. This involves careful monitoring and adjustments based on the patient’s response.Effective management of ET involves a combination of pharmacological and non-pharmacological strategies, tailored to each patient’s specific needs.
The goal is to strike a balance between controlling platelet counts and preventing complications, all while maintaining a good quality of life. Treatment choices are not arbitrary; they are based on evidence and expert consensus.
Pharmacological Treatments
Pharmacological interventions are a cornerstone of ET management. These therapies aim to reduce platelet counts and minimize the risk of thrombosis.
- Low-dose aspirin: A common first-line treatment for ET. It acts by inhibiting platelet aggregation, reducing the risk of blood clots. Benefits include reduced risk of thrombotic events, but side effects such as gastrointestinal distress are possible. Effectiveness varies depending on individual patient response and adherence to treatment.
- Cytoreductive agents: These drugs, such as hydroxyurea, interferon-alpha, and anagrelide, suppress the production of platelets in the bone marrow. Hydroxyurea is frequently used due to its proven effectiveness in reducing platelet counts and lowering the risk of thrombosis. Interferon-alpha can be effective, but side effects, including flu-like symptoms, are more common. Anagrelide, while potentially useful, can have side effects such as heart palpitations and headaches.
Essential thrombocythemia, a blood disorder, often requires careful treatment strategies. While some conventional therapies exist, exploring alternative approaches like those detailed in the article on biologics for eczema mechanisms options considerations might offer valuable insights into managing similar inflammatory processes. Ultimately, effective treatments for essential thrombocythemia depend on a thorough understanding of the individual’s condition and a tailored approach.
The choice of cytoreductive agent depends on patient factors, including comorbidities and individual preferences.
- Other medications: Other medications, such as thrombopoietin receptor agonists (TRAs), may be used in specific cases. TRAs, such as romiplostim and eltrombopag, directly target the production of platelets, offering a targeted approach for some patients. They often come with specific side effects, such as increased risk of blood clots or other adverse effects. These treatments are generally reserved for cases where other treatments are ineffective or poorly tolerated.
Non-Pharmacological Treatments
Non-pharmacological interventions play a supporting role in ET management.
- Lifestyle modifications: A healthy lifestyle, including a balanced diet, regular exercise, and maintaining a healthy weight, can contribute to overall health and potentially reduce the risk of complications. This can include strategies to manage blood pressure and cholesterol levels.
- Avoidance of risk factors: Identifying and avoiding factors that increase the risk of thrombosis is crucial. This includes smoking cessation, minimizing stress, and careful management of any existing medical conditions that may increase the risk of blood clots. Examples include careful attention to blood pressure, blood sugar, and any other medical conditions that may contribute to increased risk.
Treatment Comparison and Effectiveness
The effectiveness of various treatments can vary across different patient populations. Factors such as age, comorbidities, and the severity of ET can influence treatment responses. Patients with a higher risk profile might require more aggressive treatment strategies, while those with a lower risk might benefit from a more conservative approach.
| Treatment Modality | Potential Side Effects |
|---|---|
| Low-dose aspirin | Gastrointestinal distress, allergic reactions |
| Hydroxyurea | Bone marrow suppression, skin reactions, increased risk of infections |
| Interferon-alpha | Flu-like symptoms, fatigue, depression, hair loss |
| Anagrelide | Heart palpitations, headaches, nausea, vomiting |
| TRAs | Increased risk of blood clots, other adverse effects |
Pharmacological Treatments
Essential thrombocythemia (ET) treatment often involves a combination of strategies, with pharmacological interventions playing a crucial role. These medications aim to reduce platelet counts, prevent complications like thrombosis, and manage symptoms. Understanding the mechanisms of action, potential side effects, and monitoring parameters is essential for safe and effective patient care.
Mechanisms of Action of Commonly Used Medications
Different medications target various pathways involved in platelet production and function. Some drugs inhibit the production of platelets, while others influence their activation and aggregation. Understanding these mechanisms is vital for appreciating the drug’s efficacy and potential risks.
Classes of Medications and Their Dosages
Several classes of medications are used in ET treatment, each with its own mechanism of action, dosages, and potential side effects.
- Anticoagulants: Anticoagulants, such as aspirin, aim to prevent blood clots. Aspirin, in a low-dose regimen (typically 81 mg daily), inhibits platelet aggregation. Warfarin and heparin are also used in certain cases, but their use is typically more complex, requiring close monitoring of the INR (International Normalized Ratio) and careful consideration of individual patient needs.
- Platelet Aggregation Inhibitors: These drugs, including clopidogrel (Plavix) and ticlopidine, interfere with the ability of platelets to stick together, reducing the risk of thrombosis. Dosages vary depending on the specific drug and patient response, but generally, the initial dosage is followed by a maintenance dose. Monitoring of complete blood counts (CBCs) and signs of bleeding is crucial.
- Cytoreductive Agents: Drugs like hydroxyurea, busulfan, and anagrelide are used to reduce platelet production in the bone marrow. Hydroxyurea, for example, is frequently prescribed to reduce platelet counts in patients with ET. The dosage of hydroxyurea is often adjusted based on individual patient response and tolerance. Anagrelide is another commonly used cytoreductive agent that primarily targets the production of platelets in the bone marrow.
Monitoring of complete blood counts (CBCs), liver function tests (LFTs), and other relevant parameters is vital to ensure safety and efficacy.
Potential Side Effects of Pharmacological Interventions
Every medication has the potential for side effects, and it’s essential to be aware of these potential adverse reactions. These can range from mild discomfort to more serious complications.
- Anticoagulants: Side effects of aspirin can include gastrointestinal upset, such as nausea, heartburn, or ulcers. Warfarin can cause bleeding, skin necrosis, and interactions with other medications. Heparin can lead to heparin-induced thrombocytopenia (HIT), a potentially life-threatening condition.
- Platelet Aggregation Inhibitors: Side effects of clopidogrel and ticlopidine can include bleeding, gastrointestinal issues, and skin reactions. Careful monitoring of platelet counts and signs of bleeding is critical.
- Cytoreductive Agents: Side effects of hydroxyurea can include nausea, vomiting, fatigue, and bone marrow suppression, leading to anemia and infections. Anagrelide can cause cardiac issues, such as palpitations or arrhythmias, and can also affect the bone marrow, leading to anemia. Busulfan has significant side effects, including bone marrow suppression and potential long-term toxicity.
Monitoring Parameters During Treatment
Regular monitoring of certain parameters is essential to ensure the safety and efficacy of treatment. This allows for timely adjustments in medication dosages or treatment strategies, if needed.
- Complete Blood Counts (CBCs): CBCs are essential for monitoring platelet counts, red blood cell counts, and white blood cell counts. This helps assess the effectiveness of treatment and detect potential side effects.
- Liver Function Tests (LFTs): LFTs are crucial for monitoring the health of the liver, which can be affected by some medications used in ET treatment. This helps detect potential liver damage.
- Renal Function Tests: Renal function tests are important to monitor the health of the kidneys, which can be affected by some medications. This helps prevent potential kidney damage.
- Signs and Symptoms: Careful observation of patient symptoms, including bleeding, bruising, fatigue, or fever, is essential. Any changes should be promptly reported to the healthcare provider.
Non-Pharmacological Interventions
Essential thrombocythemia (ET) management extends beyond medication. Integrating non-pharmacological strategies can significantly enhance overall well-being and potentially mitigate some symptoms. These approaches often complement pharmacological treatments, promoting a holistic approach to care.
Lifestyle Modifications for Symptom Management
Lifestyle adjustments play a vital role in managing ET symptoms. Adopting healthy habits can improve overall health, which is particularly important for individuals with ET, who may experience heightened risks associated with the condition. These modifications can potentially reduce the risk of thrombotic events and alleviate associated symptoms.
Dietary Recommendations
A balanced diet is crucial for managing ET. Dietary choices can influence platelet counts and overall cardiovascular health, both of which are important considerations for ET patients.
- Prioritize a diet rich in fruits, vegetables, and whole grains. These foods are excellent sources of essential vitamins, minerals, and fiber, promoting overall health and potentially supporting blood vessel health.
- Limit intake of processed foods, saturated fats, and excessive sugar. These dietary components can negatively impact cardiovascular health, a concern in ET management.
- Ensure adequate hydration by drinking plenty of water throughout the day. Hydration is vital for various bodily functions, and staying well-hydrated can support overall health.
Exercise Regimens
Regular physical activity is beneficial for individuals with ET. Exercise can contribute to maintaining a healthy weight, improving cardiovascular function, and potentially reducing platelet counts.
- Engage in moderate-intensity aerobic exercises like brisk walking, swimming, or cycling for at least 30 minutes most days of the week. These exercises can enhance cardiovascular health and potentially support blood flow.
- Incorporate strength training exercises two to three times per week. Strength training can help maintain muscle mass and improve overall strength and endurance.
- Consult with a healthcare professional before starting any new exercise regimen. This is particularly important for individuals with ET to ensure the chosen activities are appropriate and safe for their specific condition.
Stress Management Techniques
Chronic stress can exacerbate various health conditions, including ET. Implementing stress management techniques can be crucial in managing symptoms and overall well-being.
- Practice relaxation techniques such as deep breathing exercises, meditation, or yoga. These practices can help calm the mind and body, potentially reducing stress levels.
- Engage in activities that promote relaxation and enjoyment, such as spending time in nature, pursuing hobbies, or engaging in social activities. These activities can provide a sense of well-being and reduce stress.
- Seek professional support when needed. A therapist or counselor can provide guidance and support in developing effective stress management strategies.
Comparative Effectiveness of Lifestyle Adjustments
| Lifestyle Adjustment | Potential Benefits in Alleviating Symptoms | Considerations |
|---|---|---|
| Balanced Diet | Improved cardiovascular health, potential modulation of platelet counts | Requires careful planning and monitoring of food choices |
| Regular Exercise | Weight management, improved cardiovascular function, potential platelet count reduction | Requires gradual progression and appropriate intensity levels |
| Stress Management | Reduced anxiety and stress levels, potential impact on symptom severity | Individualized approaches are essential, and professional guidance may be beneficial |
Treatment Considerations for Specific Patient Populations
Essential thrombocythemia (ET) requires tailored treatment strategies to address the unique needs of different patient groups. Factors like age, pregnancy status, presence of comorbidities, and the individual’s overall health significantly impact the choice and intensity of treatment. Understanding these nuances is crucial for optimizing outcomes and minimizing potential risks.
Treating Pregnant Women with ET
Pregnancy presents a complex scenario for ET management. The condition’s impact on both the mother and the fetus must be carefully considered. Maintaining adequate platelet counts while minimizing potential harm to the developing baby is paramount. Generally, treatment aims to balance the risks of uncontrolled ET with the potential complications of pregnancy.
- Careful monitoring is essential during pregnancy. Frequent blood tests to assess platelet counts and other relevant markers are crucial for early detection of any changes.
- Treatment approaches during pregnancy typically focus on reducing platelet counts to a safe level, but often with less aggressive therapies than in non-pregnant patients. This may involve lower doses of hydroxyurea or other medications. The specific choice and dosage will depend on the individual patient’s circumstances and the stage of the pregnancy.
- Close collaboration between hematologists and obstetricians is vital for ensuring the best possible outcomes for both mother and child.
Treating Children and Adolescents with ET
The treatment of ET in children and adolescents presents unique challenges. The long-term effects of treatment on growth and development need careful consideration. Furthermore, the impact of the disease on the child’s quality of life must be taken into account.
- Children and adolescents often respond differently to therapies than adults. Therefore, careful monitoring of the treatment’s effects on their growth and development is critical.
- The goal is to control the disease while minimizing potential side effects. Lower doses of certain medications, such as hydroxyurea, may be used to achieve therapeutic goals.
- Close communication with the child and their family is vital to ensure their understanding of the treatment plan and their participation in the decision-making process.
Managing ET in Elderly Patients
Elderly patients with ET may have underlying health conditions that influence treatment decisions. Their overall health status and the potential for drug interactions must be considered when selecting the most appropriate therapy. Treatment strategies should prioritize safety and minimize adverse effects.
- Careful assessment of the elderly patient’s overall health status and concurrent medical conditions is paramount.
- Treatment options are often adjusted to minimize potential drug interactions or adverse effects. Lower doses or alternative medications may be considered.
- Close monitoring of the elderly patient’s response to treatment is essential. Regular check-ups and adjustments to the treatment plan are vital.
Managing ET in Patients with Comorbidities
Patients with ET may have co-existing medical conditions (comorbidities). These conditions may influence treatment choices and require careful consideration of potential drug interactions and adverse effects. The overall well-being of the patient must be prioritized.
- Careful evaluation of the patient’s comorbidities is essential to determine the best course of action.
- Treatment strategies are often tailored to minimize the risk of interactions between ET therapies and other medications the patient may be taking for their comorbidities.
- Close collaboration between the hematologist and other specialists managing the patient’s comorbidities is essential for optimal management.
Monitoring and Management During Treatment
Navigating essential thrombocythemia (ET) treatment requires careful monitoring to ensure effectiveness and minimize potential side effects. This phase of care is crucial for maintaining patient well-being and achieving long-term control of the condition. Close collaboration between patients, their healthcare providers, and support networks is paramount for success.
Key Monitoring Parameters
Effective treatment monitoring hinges on assessing several key parameters. These parameters provide insights into treatment efficacy and potential adverse reactions. Blood counts, including platelet counts, are essential for evaluating the impact of therapy on platelet levels. Monitoring for potential complications, such as blood clots or bleeding, is also critical. Careful attention to symptoms reported by the patient, such as headaches, dizziness, or visual disturbances, is essential.
Liver and kidney function tests help assess the impact of treatment on these vital organs. Finally, regular assessment of the patient’s overall health and well-being ensures that treatment is tailored to their specific needs.
Frequency and Types of Monitoring Procedures, Treatments for essential thrombocythemia
Regular follow-up appointments are crucial for effective monitoring. The frequency and types of monitoring procedures vary depending on individual factors, such as the specific treatment regimen and the patient’s response to therapy. A typical monitoring schedule might involve blood tests every 2-4 weeks during the initial treatment phase, gradually reducing to monthly or quarterly checks as the patient’s condition stabilizes.
The table below illustrates a possible monitoring schedule.
| Monitoring Parameter | Frequency (Initial Phase) | Frequency (Stable Phase) | Types of Tests |
|---|---|---|---|
| Complete Blood Count (CBC) | Every 2-4 weeks | Monthly | Platelet count, red blood cell count, white blood cell count, hemoglobin, hematocrit |
| Platelet Count | Every 2-4 weeks | Monthly | Specific measurement of platelets in the blood |
| Liver Function Tests (LFTs) | Every 4 weeks | Quarterly | Alanine aminotransferase (ALT), Aspartate aminotransferase (AST), Bilirubin, Alkaline phosphatase |
| Kidney Function Tests (KFTs) | Every 4 weeks | Quarterly | Creatinine, Blood Urea Nitrogen (BUN) |
| Symptoms and General Health | Weekly | Monthly | Patient reported symptoms, physical examination, overall health assessment |
Adjusting Treatment Strategies
Treatment strategies should be adjusted based on the patient’s response to therapy and any side effects experienced. If platelet counts are not adequately controlled, the dosage or type of medication might need to be modified. For example, if a patient experiences significant side effects like nausea or fatigue, adjusting the treatment regimen or exploring alternative medications could be necessary.
Regular communication with the healthcare provider is crucial for timely adjustments. The treatment plan is not static; it evolves based on patient response and ongoing monitoring.
Essential thrombocythemia, a condition marked by high platelet counts, requires careful management. While various treatments are available, focusing on overall well-being is key. For instance, some explore natural remedies like incorporating apple cider vinegar into their daily routines, potentially for skin health benefits. Learning about the purported benefits of apple cider vinegar skin benefits can be an interesting avenue of exploration, though it’s crucial to remember that these are not substitutes for standard medical treatments.
Ultimately, the best course of action is to discuss options with a healthcare professional to determine the most suitable treatment plan for your specific case of essential thrombocythemia.
Importance of Regular Follow-up Appointments and Communication
Regular follow-up appointments are critical for monitoring treatment effectiveness and managing any adverse reactions. During these appointments, patients should actively communicate their symptoms and any concerns. Open communication between patients and healthcare providers is essential for ensuring the best possible outcome. For instance, if a patient notices a new symptom, they should report it promptly. Early detection of potential problems can prevent complications and allow for timely intervention.
This proactive approach underscores the partnership between the patient and healthcare team in managing ET.
Long-Term Management and Prognosis
Essential thrombocythemia (ET) requires ongoing monitoring and management to prevent serious complications. Long-term strategies focus on minimizing risks and ensuring a good quality of life for individuals affected by this condition. Understanding the potential complications and the associated prognosis is crucial for both patients and healthcare providers.
Long-Term Management Strategies
Effective long-term management of ET involves a multifaceted approach. Regular blood tests, including platelet counts, are essential to monitor disease activity and adjust treatment as needed. Patients should maintain close communication with their healthcare team, reporting any new symptoms or changes in their condition. Adherence to prescribed medications, if applicable, is critical for maintaining disease control. This may include ongoing use of medications like aspirin or other antiplatelet agents.
Additionally, lifestyle modifications, such as a healthy diet and regular exercise, are often recommended to support overall health and well-being.
Potential Complications of ET and Treatment
ET itself and its treatments can lead to various complications. Thrombosis, or blood clots, is a significant concern, potentially affecting blood vessels in the legs, lungs, or brain. The risk of bleeding, although less common, can also arise, particularly if antiplatelet medications are used. Carefully managed treatment regimens, alongside regular monitoring, help mitigate these risks.
Prognosis and Survival Rates
The prognosis for ET varies among individuals. While the disease itself isn’t typically life-threatening, the risk of thrombosis significantly impacts long-term outcomes. Survival rates for patients with ET are generally good, especially with early diagnosis and appropriate treatment. However, the specific survival rate depends on factors such as the individual’s age, overall health, and the severity of the condition.
For example, patients diagnosed at a younger age with a lower risk of complications often have a much more positive prognosis compared to those with pre-existing health conditions or a more aggressive form of the disease. Data on survival rates can be found in comprehensive medical literature.
Strategies for Maintaining Quality of Life
Living with ET requires strategies to maintain a positive quality of life. Regular communication with the healthcare team, active participation in treatment decisions, and support from family and friends are vital. Educational resources and support groups can provide valuable information and emotional support for individuals with ET. Moreover, lifestyle adjustments, such as a balanced diet and regular exercise, can help patients feel healthier and more energetic.
A strong support network and proactive management of the disease are key to maintaining a high quality of life.
Emerging Treatments and Research
Essential thrombocythemia (ET) research is constantly evolving, with promising new therapies and ongoing clinical trials exploring innovative approaches. These advancements aim to improve treatment outcomes and potentially reduce the long-term risks associated with the disease. Understanding these emerging therapies is crucial for patients and healthcare professionals alike.
Emerging Therapeutic Strategies
Several experimental treatments for ET are being investigated, moving beyond the established pharmacological interventions. These novel strategies often target specific molecular pathways implicated in the development and progression of ET. Immunotherapies, for example, are showing potential in modulating the immune system’s role in the disease.
Immunotherapies
Immunotherapeutic approaches are being explored as a potential treatment for ET. These strategies leverage the body’s own immune system to target and eliminate abnormal cells, potentially reducing platelet counts and mitigating the risks associated with thrombotic events. Preliminary studies suggest the possibility of modulating the immune response to control the disease, although more research is needed.
Targeted Therapies
Targeted therapies are another promising area of research. These treatments specifically target abnormal cellular pathways, aiming to block the mechanisms driving the overproduction of platelets in ET. Examples include drugs that inhibit specific kinases or signaling molecules. These approaches may prove effective in controlling platelet counts and reducing the risk of complications.
Clinical Trials and Research Studies
Numerous clinical trials are underway to evaluate the safety and efficacy of these emerging treatments. These trials often involve patients with ET who have not responded adequately to standard therapies or those at high risk for complications. Participating in clinical trials is often an important option for patients seeking innovative treatment approaches.
Potential Benefits and Risks of Emerging Therapies
Emerging therapies for ET hold the potential to offer improved treatment outcomes, particularly for patients who do not respond well to standard treatments. However, potential risks associated with these therapies must be carefully evaluated. Side effects may vary depending on the specific treatment and individual patient characteristics. Thorough risk-benefit analyses are crucial in deciding the best course of action for each patient.
Summary of Current Research Efforts
| Research Area | Potential Benefits | Potential Risks | Implications |
|---|---|---|---|
| Immunotherapies | Potentially modulating the immune system to control ET, reducing platelet counts. | Potential immune-related side effects, need for careful monitoring. | Could offer a new avenue for treatment in cases unresponsive to standard therapies. |
| Targeted Therapies | Precise targeting of abnormal cellular pathways, potentially controlling platelet production. | Potential for specific side effects related to the targeted pathway. | Could offer more personalized treatment options, reducing the risk of complications. |
Conclusion
In conclusion, treatments for essential thrombocythemia involve a comprehensive approach that considers the individual needs and circumstances of each patient. While pharmacological interventions remain central, non-pharmacological strategies, including lifestyle modifications and stress management, play a crucial supportive role. Regular monitoring and ongoing communication with healthcare providers are essential for optimizing treatment outcomes and ensuring the best possible long-term prognosis.
This guide provides a comprehensive overview of the current landscape of treatments, but the evolving nature of medical research warrants continued learning and adaptation.