Uses types and risks of benzodiazepines – Benzodiazepines: Uses, Types, and Risks sets the stage for a detailed exploration of these medications. This in-depth look will cover everything from their chemical makeup and mechanism of action to their various applications, potential dangers, and long-term considerations. We’ll analyze different types, examining their potency, duration, and common uses. Understanding the potential risks is crucial, so we’ll delve into side effects, dependence, and interactions with other medications.
This comprehensive guide aims to equip you with the knowledge to make informed decisions about benzodiazepines.
This discussion will explore the spectrum of conditions where benzodiazepines are prescribed, the rationale behind their use, and examples of specific drugs used for various conditions. We will also consider dosage ranges and administration schedules. Understanding the different types of benzodiazepines and their chemical structures is vital. Their pharmacokinetic profiles and receptor interactions will be examined. We’ll then move on to the crucial risks and side effects, including the potential for dependence and withdrawal symptoms.
The various potential interactions and contraindications will be discussed, emphasizing the importance of careful monitoring for patients taking these medications.
Introduction to Benzodiazepines

Benzodiazepines are a class of psychoactive drugs commonly used to treat anxiety, insomnia, and seizures. They exert their effects by modulating the activity of the central nervous system. Understanding their diverse chemical structures, mechanisms of action, and varied clinical applications is crucial for both healthcare professionals and individuals seeking information about these medications.Benzodiazepines are characterized by a specific chemical structure that allows them to interact with receptors in the brain, influencing neurotransmission.
This interaction typically results in a calming effect, reducing anxiety and promoting relaxation.
Benzodiazepine Chemical Structure and Mechanism of Action
Benzodiazepines possess a unique chemical structure consisting of a benzene ring fused to a diazepine ring. This specific molecular configuration is crucial for their interaction with the GABA A receptor complex in the brain. The GABA A receptor is a target for many central nervous system drugs. Benzodiazepines bind to a specific site on the GABA A receptor, enhancing the inhibitory effects of GABA, the primary inhibitory neurotransmitter in the brain.
This leads to increased chloride ion influx into neurons, hyperpolarizing them and ultimately reducing neuronal excitability.
Classes of Benzodiazepines
Benzodiazepines are further categorized into different classes based on their pharmacological properties. These classes, though sharing a fundamental mechanism, exhibit variations in potency, duration of action, and clinical applications.
- Short-acting benzodiazepines, such as triazolam and midazolam, are often prescribed for short-term anxiety or insomnia. Their rapid onset and shorter duration of action make them suitable for situations where a rapid effect is desired, but their use should be limited to a short period due to the risk of dependence.
- Intermediate-acting benzodiazepines, including alprazolam and lorazepam, offer a balance between efficacy and duration. They are commonly used for a range of anxiety disorders and are often prescribed for a longer period than short-acting ones, but the duration should still be limited and monitored closely.
- Long-acting benzodiazepines, such as diazepam and clonazepam, are generally reserved for conditions requiring sustained relief. They are effective in managing chronic anxiety, but their extended duration of action can pose a higher risk of dependence, and the risk is further amplified when combined with other substances.
Comparison of Benzodiazepine Classes
The table below summarizes the key differences between the classes of benzodiazepines based on potency, duration of action, and typical uses.
| Class | Common Names | Potency | Duration of Action | Typical Uses |
|---|---|---|---|---|
| Short-acting | Triazolam, Midazolam | Moderate | Short | Anxiety, insomnia, pre-operative sedation |
| Intermediate-acting | Alprazolam, Lorazepam | Moderate | Intermediate | Anxiety, panic disorder, insomnia |
| Long-acting | Diazepam, Clonazepam | High | Long | Muscle spasms, seizures, anxiety, insomnia |
Routes of Administration
Benzodiazepines can be administered through various routes, each with its own advantages and disadvantages. The choice of route depends on the specific clinical situation and the desired onset and duration of action.
| Route | Description | Typical Use |
|---|---|---|
| Oral | Swallowed in pill or liquid form | Most common route for long-term or acute anxiety, insomnia |
| Intravenous (IV) | Administered directly into a vein | Rapid onset, used in emergency situations, pre-operative sedation, and acute agitation |
| Intramuscular (IM) | Administered directly into a muscle | Rapid onset, useful in situations where IV access is not readily available, such as in emergencies. |
Uses of Benzodiazepines
Benzodiazepines are a class of medications known for their anxiolytic (anxiety-reducing) properties. However, their use extends beyond managing anxiety, encompassing a range of other medical conditions where their sedative and muscle relaxant effects prove beneficial. Understanding their various applications, along with the rationale behind their prescription, is crucial for responsible use and minimizing potential risks.Benzodiazepines are commonly prescribed for a variety of medical conditions, where their ability to reduce anxiety, induce sedation, and relax muscles can significantly improve patient well-being.
The rationale behind their use often stems from the need to manage symptoms effectively, particularly when other treatments have proven insufficient or less tolerable.
Anxiety Disorders
Benzodiazepines are frequently prescribed to manage acute and chronic anxiety disorders. Their rapid onset of action allows for immediate symptom relief, making them helpful in situations like panic attacks or severe anxiety episodes. This rapid relief can be crucial in preventing escalation of symptoms and allowing the patient to cope more effectively. Alprazolam (Xanax) and lorazepam (Ativan) are common choices for managing anxiety disorders.
Typical dosage ranges vary depending on the severity of the condition and the individual patient response, but generally, they start with low doses and are titrated up as needed, under strict medical supervision.
Insomnia
Benzodiazepines can be prescribed for insomnia, particularly short-term use. Their sedative effects can promote relaxation and sleep onset. However, their use for insomnia should be approached cautiously, as prolonged use can lead to dependence and withdrawal symptoms. Temazepam and flurazepam are examples of benzodiazepines used for insomnia. Dosage ranges and administration schedules are tailored to individual needs, with typical doses ranging from 5 to 30 mg, taken at bedtime.
Benzodiazepines, while sometimes prescribed for anxiety, have various uses, types, and potential risks. For instance, they can be helpful in managing muscle spasms, but long-term use can lead to dependence. Understanding the connection between chronic inflammatory skin conditions like hidradenitis suppurative and potential impacts of COVID-19 is also crucial hidradenitis suppurative and covid 19. Ultimately, a thorough discussion with a healthcare professional about the risks and benefits is essential when considering any medication, especially benzodiazepines.
It is crucial to adhere to the prescribed schedule to maximize efficacy and minimize risks.
Muscle Spasms and Pain
Benzodiazepines can be helpful in managing muscle spasms and pain associated with various conditions, such as multiple sclerosis, spinal cord injuries, or chronic pain syndromes. Their muscle relaxant properties can provide relief from spasms and associated discomfort. Diazepam (Valium) is often prescribed for these conditions. Dosage and administration are typically determined by the severity of the condition and individual patient tolerance.
Benzodiazepines, while sometimes prescribed for anxiety or insomnia, have various uses and types, each with potential risks. Understanding these risks is crucial. For example, if you’re experiencing diarrhea, consider exploring over-the-counter and prescription options like those found in diarrhea relief otc and prescription medications. However, it’s important to remember that self-treating with benzodiazepines can be dangerous and should only be done under a doctor’s supervision.
Different types of benzodiazepines carry varying degrees of risk, so always consult a medical professional for personalized advice.
Treatment regimens may involve adjusting the dose and frequency as needed.
Seizure Disorders
In certain seizure disorders, benzodiazepines can be used to control or prevent seizures. Their anticonvulsant effects can help manage seizure activity, particularly in acute situations. Clonazepam (Klonopin) is a commonly used benzodiazepine for this purpose. Dosage and administration schedules are crucial to effectively manage seizures and should be strictly adhered to under medical supervision.
Table: Common Uses of Benzodiazepines
| Condition | Commonly Prescribed Benzodiazepine(s) |
|---|---|
| Anxiety Disorders | Alprazolam (Xanax), Lorazepam (Ativan) |
| Insomnia | Temazepam, Flurazepam |
| Muscle Spasms/Pain | Diazepam (Valium) |
| Seizure Disorders | Clonazepam (Klonopin) |
Types of Benzodiazepines
Benzodiazepines, a class of central nervous system depressants, are categorized into various subtypes based on their chemical structures and resulting pharmacodynamic properties. Understanding these differences is crucial for prescribing the most appropriate medication and managing potential risks. This section delves into the diverse types of benzodiazepines, examining their structural variations, pharmacokinetic profiles, receptor interactions, and the relationship between their chemical structures and effects.The diverse chemical structures of benzodiazepines lead to varying effects on the body.
Some are better suited for short-term anxiety relief, while others might be more effective for sleep disorders. Knowing these distinctions allows for a more targeted approach to treatment, enhancing patient outcomes.
Chemical Structures and Properties
Benzodiazepines share a core chemical structure, but variations in substituents lead to differences in their properties. These variations significantly impact their metabolism, duration of action, and overall pharmacological effects. The substituents attached to the core structure dictate the drug’s interaction with specific receptors in the brain, affecting its effectiveness and potential side effects.
Pharmacokinetic Profiles
The pharmacokinetic profiles of different benzodiazepines vary, affecting their absorption, distribution, metabolism, and elimination rates. These variations directly impact the duration of their action and the potential for side effects like sedation or cognitive impairment. For example, shorter-acting benzodiazepines might be preferable for treating acute anxiety episodes, while longer-acting ones might be more suitable for managing chronic conditions.
Benzodiazepines, like Xanax and Valium, have various uses, but also carry potential risks. They’re often prescribed for anxiety and sleep disorders, but long-term use can lead to dependence. Interestingly, a skin condition sometimes associated with COVID-19 is a rash, which can present in various ways. Learning more about the different types of rashes and their causes, like those seen in covid rash in adults , is crucial.
Understanding the potential for side effects and interactions is key when considering these medications.
Receptor Interactions
Benzodiazepines exert their effects by interacting with specific receptors in the central nervous system. The primary target is the GABA A receptor complex. These receptors play a crucial role in regulating neuronal excitability, and benzodiazepines enhance the inhibitory effects of GABA, leading to reduced neuronal activity. The precise binding site and the degree of interaction with GABA A receptors vary among different benzodiazepine types, influencing their effects.
Relationship Between Structure and Pharmacodynamic Effects, Uses types and risks of benzodiazepines
The relationship between the chemical structure and pharmacodynamic effects of benzodiazepines is complex but significant. Substituent modifications alter the affinity of the drug for the GABA A receptor, influencing its potency, duration of action, and overall effect on the central nervous system. For instance, variations in the substituents can affect the drug’s lipid solubility, influencing its distribution and subsequent action within the body.
Table of Benzodiazepines
| Type | Chemical Name | Common Brand Names |
|---|---|---|
| Short-acting | Alprazolam | Xanax |
| Short-acting | Lorazepam | Ativan |
| Intermediate-acting | Diazepam | Valium |
| Intermediate-acting | Clonazepam | Klonopin |
| Long-acting | Temazepam | Restoril |
| Long-acting | Flurazepam | Dalmane |
Risks and Side Effects: Uses Types And Risks Of Benzodiazepines
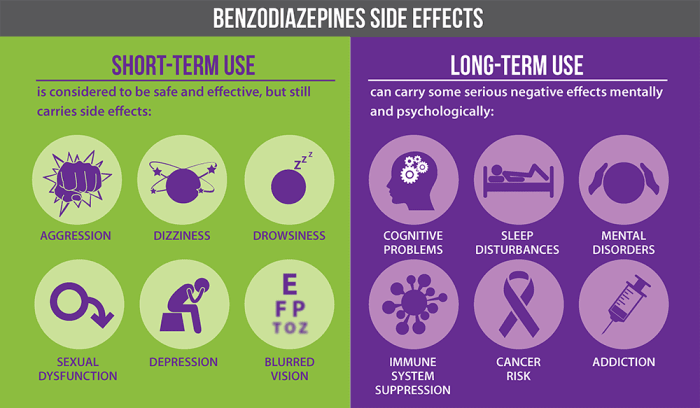
Benzodiazepines, while effective for managing anxiety and other conditions, carry potential risks and side effects that users should be aware of. Understanding these risks is crucial for responsible use and ensures that patients can make informed decisions about their treatment plans. Careful monitoring and adherence to prescribed dosages are vital for minimizing potential harm.Benzodiazepines, due to their mechanism of action, can influence various bodily functions.
This can lead to a range of side effects, some mild and temporary, others more serious and persistent. The severity and likelihood of side effects can vary depending on the individual, the specific benzodiazepine used, and the dosage. It’s also important to remember that individual responses to medications can be unpredictable.
Potential Side Effects
Benzodiazepines can affect various physiological systems, leading to a wide range of side effects. These effects can include drowsiness, dizziness, and difficulty concentrating, all of which can impair cognitive function and motor skills. These are generally considered mild and temporary. More serious side effects can include respiratory depression, especially at higher doses or in combination with other depressant medications.
Mechanism of Side Effects
Benzodiazepines primarily work by enhancing the effects of GABA, an inhibitory neurotransmitter in the brain. This enhancement of GABAergic transmission leads to a calming effect. However, this increased inhibition can also lead to unwanted side effects. The exact mechanism by which certain side effects manifest is still under investigation, but it is thought to involve varying degrees of inhibition across different neural pathways.
Dependence and Withdrawal
Benzodiazepines can lead to physical dependence, meaning the body adapts to their presence. Stopping use abruptly can trigger withdrawal symptoms, which can range from mild discomfort to severe and potentially life-threatening conditions. Symptoms of benzodiazepine withdrawal can include anxiety, insomnia, tremors, and seizures. It’s crucial to gradually reduce the dosage under medical supervision to minimize withdrawal risks.
Gradual tapering under medical supervision is crucial to mitigate the risks of severe withdrawal.
Risks Associated with Different Types
Different benzodiazepines vary in their potency and duration of action. These differences influence the potential risks associated with each. For example, short-acting benzodiazepines may have a higher risk of dependence compared to long-acting ones. The specific half-life of each benzodiazepine impacts the likelihood and intensity of withdrawal symptoms.
Comparison of Risks
| Benzodiazepine Type | Potential Risks | Side Effects | Precautions |
|---|---|---|---|
| Short-acting (e.g., Alprazolam) | Higher risk of dependence, more rapid withdrawal symptoms | Dizziness, drowsiness, impaired coordination | Gradual tapering essential, close monitoring required |
| Intermediate-acting (e.g., Lorazepam) | Moderate risk of dependence, withdrawal symptoms may be less severe | Drowsiness, dizziness, difficulty concentrating | Careful dosage adjustment, regular follow-ups |
| Long-acting (e.g., Diazepam) | Lower risk of dependence, slower withdrawal symptoms | Drowsiness, dizziness, impaired coordination, potential for prolonged sedation | Gradual tapering essential, especially when discontinuing |
Interactions and Contraindications
Benzodiazepines, while often effective, can interact with other medications and pose risks for certain patient populations. Understanding these interactions and contraindications is crucial for safe and effective prescribing. This section delves into potential drug interactions, specific examples of medications to avoid or use cautiously, contraindications for various patient groups, and the importance of careful monitoring.
Potential Drug Interactions
Benzodiazepines can significantly affect the metabolism and efficacy of other medications. This interaction can lead to heightened side effects or reduced therapeutic benefits of the co-administered drugs. The combined effects of multiple medications can be unpredictable and potentially dangerous, especially if not carefully monitored.
Examples of Medications to Avoid or Use Cautiously
Certain medications interact significantly with benzodiazepines, increasing the risk of adverse events. Examples include:
- Alcohol: Combining alcohol with benzodiazepines dramatically increases the risk of sedation, respiratory depression, and cognitive impairment. The combined effect can be more pronounced than the sum of the individual effects.
- Opioids: The concurrent use of benzodiazepines and opioids can result in profound respiratory depression, potentially leading to life-threatening situations. This combination should be avoided whenever possible.
- Other CNS depressants: Benzodiazepines interact with other central nervous system (CNS) depressants like antihistamines, muscle relaxants, and certain antidepressants, potentiating the sedative effects and increasing the risk of respiratory depression. Careful consideration and monitoring are essential.
- Anticonvulsants: Some anticonvulsants may alter the metabolism of benzodiazepines, potentially affecting their efficacy or increasing the risk of side effects. Individualized dosing adjustments may be necessary.
Contraindications for Specific Patient Populations
Certain patient groups should avoid benzodiazepines due to increased risks. These include:
- Patients with severe respiratory issues: Benzodiazepines can suppress respiratory function, which can be life-threatening in individuals with pre-existing respiratory problems. Alternatives to benzodiazepines should be considered.
- Patients with a history of substance abuse: Benzodiazepines have a high potential for abuse, and patients with a history of substance abuse may be at a higher risk of dependence or overdose. Alternatives or careful monitoring should be considered in such cases.
- Patients with severe hepatic or renal impairment: Benzodiazepines are primarily metabolized by the liver and kidneys. Individuals with impaired liver or kidney function may experience delayed elimination, leading to accumulation of the drug in the body and increased risk of side effects. Lower doses or alternative therapies are often necessary.
- Patients with sleep apnea: Benzodiazepines can worsen sleep apnea by further relaxing the muscles in the throat, potentially leading to breathing problems. Alternatives should be considered.
Important Considerations
Careful monitoring is essential for patients taking benzodiazepines. Regular assessment of vital signs, including respiratory rate and blood pressure, is crucial to identify and manage potential side effects.
Table of Potential Drug Interactions and Contraindications
| Drug Interaction/Contraindication | Potential Risk | Mitigation Strategy |
|---|---|---|
| Alcohol | Increased sedation, respiratory depression | Avoid concurrent use; monitor closely |
| Opioids | Severe respiratory depression, overdose risk | Avoid concurrent use; use with extreme caution if unavoidable |
| Other CNS depressants | Exaggerated sedation, respiratory depression | Monitor closely; consider alternative therapies |
| Patients with severe respiratory issues | Respiratory depression, apnea | Avoid benzodiazepines; explore alternative therapies |
| Patients with substance abuse history | Increased risk of dependence, overdose | Careful monitoring; consider alternative therapies |
| Patients with hepatic/renal impairment | Delayed elimination, increased side effects | Lower doses; monitor closely |
Long-Term Effects and Considerations

Benzodiazepines, while effective for short-term anxiety and sleep disorders, can have significant long-term effects if used improperly. Understanding these potential consequences is crucial for responsible use and management. This section delves into the lasting impacts of benzodiazepine use, highlighting the importance of careful monitoring and tapering strategies.Long-term benzodiazepine use can lead to a range of physical and psychological changes.
The duration and dosage of the medication, combined with pre-existing health conditions, significantly influence the potential for negative outcomes. This discussion emphasizes the importance of open communication with healthcare providers regarding potential risks and alternative treatment options.
Potential Impact on Cognitive Function and Memory
Benzodiazepines can affect various cognitive functions, including memory and attention. Studies suggest that chronic use may lead to impairments in cognitive performance, affecting tasks requiring focus and recall. Individuals experiencing these effects may notice difficulties with concentration, learning new information, and remembering recent events. The extent of these cognitive impacts varies significantly among individuals, influenced by factors like age, pre-existing cognitive conditions, and the duration of benzodiazepine use.
Potential for Tolerance and Dependence
Tolerance to the effects of benzodiazepines frequently develops with prolonged use. This means that the initial dosage may become less effective over time, necessitating an increase in the dose to achieve the same therapeutic effect. This escalation can lead to dependence, where the body adapts to the presence of the medication and experiences withdrawal symptoms if use is abruptly discontinued.
Withdrawal symptoms can range from mild discomfort to severe complications, emphasizing the necessity of gradual tapering under medical supervision.
Importance of Careful Monitoring and Tapering Strategies
Discontinuing benzodiazepines abruptly can lead to serious withdrawal symptoms, including seizures, anxiety, and tremors. A gradual reduction in dosage, known as tapering, is crucial to mitigate these risks. This process requires careful monitoring by a healthcare provider to ensure a safe and controlled transition. A tapering schedule should be personalized, taking into account the individual’s specific needs, the duration of use, and the type of benzodiazepine being used.
Table of Long-Term Risks and Considerations
| Potential Long-Term Risk | Description and Considerations |
|---|---|
| Cognitive Impairment | Possible difficulties with concentration, memory, and learning. The risk increases with prolonged use. |
| Tolerance and Dependence | The body adapts to the medication, requiring higher doses for the same effect. Abrupt cessation can lead to severe withdrawal symptoms. |
| Withdrawal Symptoms | Can range from mild discomfort to severe complications (seizures, anxiety) if discontinued abruptly. Tapering is crucial. |
| Physical Health Impacts | Possible interaction with other medications, increasing the risk of adverse reactions. Chronic use can contribute to other health problems, including sleep disorders. |
| Psychological Effects | Prolonged use can increase the risk of anxiety, depression, and other mood disorders. |
Overdose and Emergency Management
Benzodiazepines, while crucial for managing anxiety and other conditions, carry the risk of overdose. Understanding the signs and symptoms, appropriate emergency procedures, and the role of antidotes is vital for ensuring patient safety. Knowing how to respond in a timely manner can significantly impact the outcome of a benzodiazepine overdose.Benzodiazepine overdose can manifest in a spectrum of symptoms, ranging from mild sedation to life-threatening respiratory depression.
Early recognition and prompt intervention are critical to minimize potential complications. It’s important to remember that these symptoms can vary depending on the specific benzodiazepine involved, the individual’s health status, and the amount ingested.
Signs and Symptoms of Benzodiazepine Overdose
Recognizing the signs and symptoms of benzodiazepine overdose is crucial for immediate action. Symptoms often include excessive drowsiness, confusion, slurred speech, and difficulty with coordination. More severe cases may present with respiratory depression, decreased heart rate, and loss of consciousness. The severity of these symptoms is often correlated with the dose of the benzodiazepine and the individual’s sensitivity.
Emergency Management Procedures
Prompt action is essential in managing a benzodiazepine overdose. The first step is to ensure the individual’s airway, breathing, and circulation (ABCs) are maintained. If the individual is unconscious, place them in the recovery position and call emergency services immediately. Providing supportive care, such as administering oxygen and monitoring vital signs, is vital.
Role of Specific Antidotes
While supportive care is the cornerstone of benzodiazepine overdose management, specific antidotes can play a crucial role. Flumazenil is a benzodiazepine antagonist commonly used in these situations. Its primary function is to reverse the effects of benzodiazepines by binding to benzodiazepine receptors and preventing further action of the drug.
Common Benzodiazepine Antagonists
Flumazenil is a crucial benzodiazepine antagonist used in emergency situations. It’s essential to understand that flumazenil is not a universal antidote and its use should be carefully considered and monitored by healthcare professionals.
Steps in Managing a Benzodiazepine Overdose
The following table Artikels the critical steps in managing a benzodiazepine overdose.
| Step | Action |
|---|---|
| 1 | Assess the situation: Ensure the individual’s airway, breathing, and circulation are maintained. |
| 2 | Call emergency services: Promptly contact emergency medical services for immediate assistance. |
| 3 | Provide supportive care: Administer oxygen, monitor vital signs, and maintain a safe environment. |
| 4 | Administer flumazenil (if appropriate and under medical supervision): This benzodiazepine antagonist can reverse the effects of the overdose, but its use requires careful consideration. |
| 5 | Transport to hospital: Immediate transport to a medical facility is essential for continued monitoring and treatment. |
Patient Counseling and Education
Educating patients about benzodiazepines is crucial for safe and effective use. This involves conveying not only the benefits but also the potential risks and side effects. A thorough understanding empowers patients to make informed decisions about their treatment and manage potential complications proactively. This section delves into essential information for patient counseling, addressing common questions, and outlining strategies for effective education.
Essential Information for Patient Counseling
Effective patient counseling requires a clear and concise explanation of benzodiazepines. Patients need to understand the purpose of these medications, how they work, and the potential consequences of misuse. This includes details about the medication’s intended use, its effects on the body, and its potential interactions with other substances. Crucially, patients should be aware of the possibility of developing tolerance and dependence.
Common Patient Questions
Patients often have concerns and questions about benzodiazepines. Understanding these questions allows healthcare providers to address patient anxieties and concerns effectively. Examples of frequently asked questions include:
- What are the potential side effects of this medication?
- How long will I need to take this medication?
- Can I stop taking this medication suddenly?
- How will this medication affect my daily activities?
- What are the risks of mixing this medication with alcohol or other substances?
- Are there any long-term effects associated with benzodiazepine use?
Importance of Patient Education
Patient education regarding benzodiazepines is vital. Understanding the potential risks and benefits empowers patients to make informed decisions about their treatment. This knowledge allows them to recognize and report any unusual side effects, preventing potential complications. The benefits of this knowledge are paramount to patient safety and adherence to treatment plans.
Strategies for Patient Education
Patient education should be tailored to individual needs and comprehension levels. Using clear, concise language is essential. Visual aids, such as diagrams or charts, can enhance understanding. Encourage open communication and address patient concerns directly.
- Use clear and concise language: Avoid medical jargon and explain complex concepts in simple terms. Provide examples relatable to the patient’s life.
- Emphasize the importance of adherence: Explain the importance of taking the medication as prescribed and the potential consequences of non-adherence.
- Address potential risks and benefits: Clearly articulate the benefits of the medication while highlighting potential side effects and risks. Provide resources for further information.
- Encourage open communication: Create a safe space for patients to ask questions and express concerns without fear of judgment. This will help them to understand the risks and benefits and make informed decisions about their treatment.
Key Points for Patient Counseling and Education
The following table summarizes essential points for patient counseling and education regarding benzodiazepine use.
| Topic | Key Point |
|---|---|
| Purpose | Benzodiazepines are used to treat anxiety, insomnia, and seizures. |
| Mechanism of Action | Benzodiazepines enhance the effects of GABA, a neurotransmitter that helps calm the brain. |
| Potential Risks | Tolerance, dependence, withdrawal symptoms, and interactions with other medications. |
| Importance of Adherence | Adherence to the prescribed dosage and schedule is critical for safety and effectiveness. |
| Patient Questions | Address patient questions and concerns regarding side effects, duration of use, and potential risks. |
| Education Resources | Provide educational materials and resources to patients for continued learning. |
Last Recap
In conclusion, benzodiazepines, while valuable in certain medical situations, come with a range of potential risks. Understanding their uses, types, and risks is essential for responsible use and informed decision-making. The potential for dependence and withdrawal, combined with possible long-term effects, underscores the need for careful monitoring and professional guidance. This comprehensive overview provides a foundation for further research and discussion, emphasizing the importance of patient education and communication with healthcare providers.