Nasal polyps symptoms dizzy can significantly impact daily life. This comprehensive exploration delves into the various symptoms, potential causes, and available treatment options for this condition. Understanding the interplay between nasal polyps and dizziness is crucial for effective management.
Nasal polyps are benign growths that develop inside the nasal passages. They often cause nasal congestion, difficulty breathing, and a range of other symptoms. This condition, while not life-threatening, can disrupt daily activities and quality of life. The connection between nasal polyps and dizziness is complex, often stemming from the swelling and inflammation within the nasal passages and their impact on the balance system.
This article will delve into these connections, examining the symptoms, causes, diagnosis, and treatment strategies.
Nasal Polyps and Dizziness: A Deeper Look
Nasal polyps are benign growths that develop within the lining of the nasal passages. These fleshy, often pale-colored tissues can obstruct airflow, leading to various symptoms. While often associated with chronic allergies or other inflammatory conditions, the exact cause of nasal polyps isn’t always clear. Understanding their presence and potential connections to dizziness is important for proper diagnosis and management.The presence of nasal polyps can create a cascade of symptoms, some of which are fairly common and some less so.
This exploration will delve into the potential link between nasal polyps and dizziness, examining the mechanisms that might explain this association.
Nasal Polyp Characteristics
Nasal polyps are noncancerous growths that form in the lining of the nasal passages and sinuses. They are often associated with chronic inflammation, typically from conditions like allergic rhinitis, cystic fibrosis, or asthma. Their development can be gradual, sometimes going unnoticed until they cause significant symptoms. The exact mechanisms leading to their formation remain an active area of research.
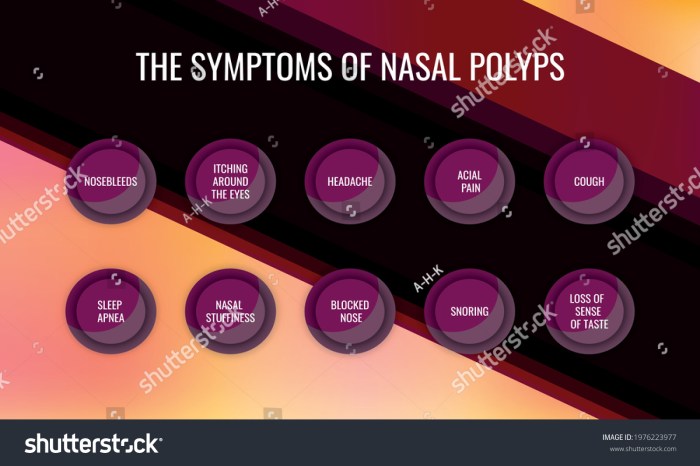
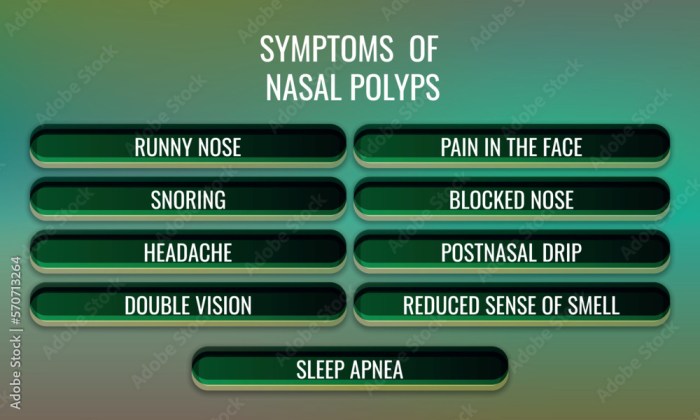
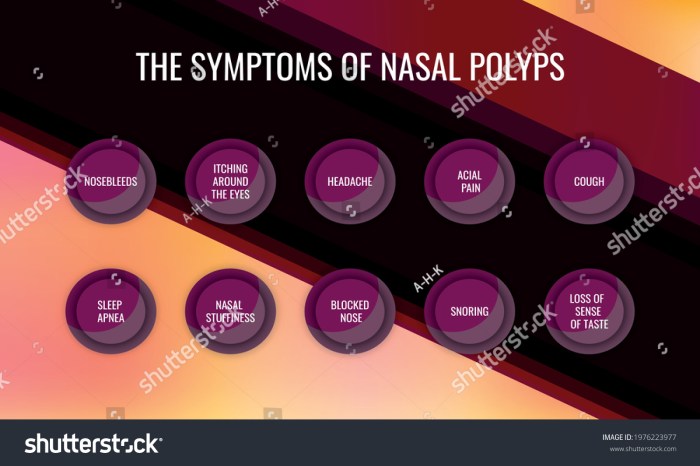
Symptoms of Nasal Polyps
Nasal polyps present a variety of symptoms, which can range from mild to severe. A key characteristic is the gradual onset and progression of these symptoms, which may initially be subtle and easily overlooked. Recognizing the specific symptoms and their frequency is critical in proper diagnosis and treatment planning.
| Symptom | Description | Frequency |
|---|---|---|
| Nasal Congestion | A feeling of stuffiness or blockage in the nasal passages, often impacting breathing. | Common |
| Facial Pain/Pressure | Discomfort or pain in the facial area, especially around the sinuses. | Common |
| Runny Nose | Discharge, which can be clear, white, or yellowish, and may be accompanied by a postnasal drip. | Common |
| Loss of Smell/Taste | Diminished or absent sense of smell or taste. | Common |
| Headaches | Pain in the head, often localized to the forehead or temples. | Common |
| Postnasal Drip | Mucus dripping down the back of the throat, causing a persistent cough or sore throat. | Common |
| Hearing Loss | Difficulty hearing clearly, sometimes related to Eustachian tube dysfunction. | Uncommon |
| Dizziness | A sensation of lightheadedness, imbalance, or spinning. | Potentially linked, but less common as a direct symptom. |
Nasal Polyps and Dizziness: Potential Mechanisms
While dizziness isn’t a primary symptom of nasal polyps, a connection is possible. Obstruction of the nasal passages can impact airflow and sinus pressure. This altered airflow can potentially affect the inner ear, leading to dizziness. Furthermore, inflammation related to nasal polyps might influence the central nervous system, impacting balance and equilibrium. However, more research is needed to definitively establish a direct causal relationship.
In some cases, a patient might report dizziness as a symptom alongside other polyp-related issues. It’s important to remember that the presence of nasal polyps doesn’t automatically mean dizziness will occur.
Symptoms of Nasal Polyps
Nasal polyps, while often benign growths, can significantly impact quality of life. Understanding the array of symptoms, including those potentially linked to dizziness, is crucial for timely diagnosis and effective management. This section delves into the various manifestations of nasal polyps, emphasizing their potential influence on dizziness.Nasal polyps can present with a wide range of symptoms, ranging from mild discomfort to severe impairment.
The symptoms often overlap with other conditions, making accurate diagnosis essential. The degree of symptom severity varies greatly depending on the size, location, and number of polyps, as well as the individual’s overall health.
Symptoms Related to Nasal Obstruction
Nasal obstruction is a hallmark symptom of nasal polyps. This blockage can lead to difficulty breathing through the nose, causing a shift in how the body processes airflow. This is often a common and early symptom reported by patients. The severity of obstruction can range from mild difficulty breathing to complete nasal blockage, requiring constant use of mouth breathing.
This constant mouth breathing can further contribute to issues like dry mouth and throat, as well as impacting sleep quality.
Symptoms Related to Sinus Pressure and Pain
Sinus pressure and pain are frequently associated with nasal polyps. The growths can press against the sinus cavities, causing discomfort, throbbing pain, or a feeling of fullness in the face. The pain can be localized to the forehead, cheeks, or around the eyes. In some cases, the pressure and pain can radiate to the temples or even the teeth.
The pain is often described as dull or sharp, and can vary in intensity.
Symptoms Related to Dizziness and Balance Issues
While not as prominent as other symptoms, dizziness and balance issues can sometimes be linked to nasal polyps. The nasal blockage caused by polyps can affect the normal airflow to the inner ear, impacting balance mechanisms. In some individuals, this may result in episodes of lightheadedness, vertigo, or unsteadiness. The severity of dizziness can vary, from mild feelings of faintness to more pronounced episodes of vertigo, impacting daily activities.
This is a less common symptom but should not be disregarded.
Symptoms Related to Hearing Loss
Nasal polyps, when situated close to the Eustachian tube, can sometimes lead to hearing loss. The blockage caused by the polyps can impair the tube’s ability to equalize pressure between the middle ear and the nasal passages, which is crucial for clear hearing. This is particularly noticeable in cases where the polyps are extensive. The hearing loss can be subtle or pronounced, and its severity depends on the extent of the blockage.
Symptoms Related to Smell and Taste Changes
Nasal polyps can impact the sense of smell and taste. The blockage can prevent odor molecules from reaching the olfactory nerves, resulting in a diminished sense of smell. Similarly, taste perception can also be affected, potentially causing a loss of taste or a change in taste perception. The degree of change can vary, from a slight reduction in sensitivity to a complete loss of smell or taste.
Experiencing nasal polyps and dizziness can be a real head-scratcher. It’s important to remember that these symptoms aren’t always related, but sometimes they can be. While researching other potential causes, you might find it interesting to learn about the differences between vitiligo and albinism, which are both skin conditions. For a detailed breakdown of vitiligo vs albinism what s the difference, check out this helpful resource: vitiligo vs albinism what s the difference.
Ultimately, if you’re concerned about these nasal polyp symptoms and dizziness, it’s always best to consult a doctor for proper diagnosis and treatment.
Symptom Summary Table
| Symptom | Description | Potential Impact on Dizziness |
|---|---|---|
| Nasal Obstruction | Difficulty breathing through the nose, mouth breathing | May affect airflow to inner ear, potentially leading to dizziness. |
| Sinus Pressure/Pain | Discomfort, throbbing, fullness in the face | Indirectly, significant pain can lead to dizziness through stress response. |
| Dizziness/Balance Issues | Lightheadedness, vertigo, unsteadiness | Directly related to potential inner ear airflow disruption. |
| Hearing Loss | Impaired ability to hear | May indirectly affect balance if the inner ear is impacted. |
| Smell/Taste Changes | Diminished sense of smell or taste | Indirectly, changes in smell/taste can cause discomfort or anxiety, potentially leading to dizziness. |
Potential Causes of Dizziness with Nasal Polyps
Nasal polyps, while primarily affecting the nasal passages, can sometimes lead to dizziness. Understanding the potential connections between these seemingly disparate issues is crucial for effective diagnosis and management. This exploration delves into the physiological mechanisms that might link nasal congestion with balance problems.The intricate relationship between the nasal passages and the body’s balance system is not immediately obvious.
However, the interconnectedness of the head and neck regions plays a significant role in how we perceive balance. Inflammation and swelling, common features of nasal polyps, can impact this intricate system, leading to symptoms beyond the typical nasal discomfort.
Physiological Connections
Nasal congestion, a hallmark of nasal polyps, can directly affect the balance system. The pressure changes and restricted airflow within the nasal passages can disrupt the normal functioning of the inner ear structures, including the semicircular canals, which are vital for balance. This disruption can trigger dizziness or vertigo. Additionally, inflammation and swelling can extend beyond the nasal cavity, potentially impacting nearby cranial nerves and blood vessels that influence equilibrium.
Impact of Nasal Congestion on the Balance System
Nasal congestion significantly impedes the normal function of the olfactory and trigeminal nerves, which play a crucial role in facial sensations. The obstruction of airflow can lead to reduced oxygenation, which in turn affects the brain’s ability to regulate balance and coordination. This can manifest as dizziness or even lightheadedness.
Role of Inflammation and Swelling
Inflammation and swelling associated with nasal polyps can extend to surrounding tissues, including the nerves and blood vessels crucial for maintaining equilibrium. This swelling can exert pressure on these delicate structures, causing disruption to their normal functioning. Chronic inflammation, a key feature of nasal polyps, can lead to long-term effects on the balance system, potentially resulting in persistent dizziness.
Potential for Other Underlying Medical Conditions
It’s important to remember that dizziness can stem from various medical conditions beyond nasal polyps. Other underlying conditions, such as inner ear infections, neurological disorders, or even medication side effects, can mimic the symptoms of dizziness. A comprehensive evaluation by a healthcare professional is essential to rule out other potential causes and ensure proper treatment.
Experiencing dizzy spells alongside nasal polyps can be a confusing mix of symptoms. While the exact connection isn’t fully understood, it’s important to explore potential underlying causes. Learning about drusen meaning and types might offer a clearer picture, as some conditions associated with these tiny deposits can also impact balance. drusen meaning and types could shed light on possible correlations, ultimately helping you understand the complex interplay of symptoms.
This knowledge could be helpful in discussing your symptoms with a doctor and getting the right diagnosis and treatment for nasal polyps symptoms dizzy.
Table of Potential Causes of Dizziness with Nasal Polyps
| Potential Cause | Explanation | Symptoms Associated with Dizziness |
|---|---|---|
| Nasal Polyp-Induced Congestion | Pressure changes and airflow restrictions within the nasal passages can disrupt the inner ear structures responsible for balance. | Dizziness, vertigo, lightheadedness, imbalance, nausea, and possible vomiting. |
| Inflammation and Swelling | Inflammation and swelling in the nasal passages and surrounding tissues can exert pressure on nerves and blood vessels that influence equilibrium. | Dizziness, fluctuating balance, and episodic vertigo, particularly after periods of exertion or stress. |
| Underlying Medical Conditions | Other medical conditions, including inner ear infections, neurological disorders, and medication side effects, can present with similar symptoms. | Dizziness, accompanied by other symptoms such as tinnitus, hearing loss, headache, or neurological deficits. |
Diagnosis and Treatment: Nasal Polyps Symptoms Dizzy
Unraveling the connection between nasal polyps and dizziness requires a meticulous diagnostic process. This often involves a combination of physical examinations, imaging techniques, and potentially, specialized tests to pinpoint the specific cause. Understanding the diagnostic steps and available treatments is crucial for effective management of these conditions.Accurate diagnosis hinges on a thorough evaluation of symptoms and medical history.
This includes a detailed description of the dizziness, its frequency, and potential triggers, alongside a comprehensive assessment of nasal polyp characteristics, duration, and associated symptoms.
Diagnostic Process for Nasal Polyps and Dizziness
The diagnostic process for nasal polyps and dizziness involves several steps, starting with a comprehensive medical history and physical examination. Physicians will investigate the nature of the dizziness, its frequency and intensity, and any potential triggers. A thorough nasal examination is crucial to identify the presence and characteristics of nasal polyps.
Potential Diagnostic Tests, Nasal polyps symptoms dizzy
Various diagnostic tests can aid in pinpointing the cause of dizziness and evaluating the extent of nasal polyps. These tests are essential to determine the underlying issues contributing to the patient’s symptoms.
- Nasal Endoscopy: This procedure involves inserting a thin, flexible tube with a camera into the nasal passages to visualize the nasal cavity and identify the presence, size, and location of polyps. This provides crucial information for guiding treatment decisions. Nasal endoscopy is a non-invasive technique, typically well-tolerated, and is highly effective in evaluating the nasal cavity.
- CT Scan or MRI: Computed tomography (CT) and magnetic resonance imaging (MRI) scans are valuable for providing detailed images of the sinuses and surrounding structures. CT scans are particularly helpful for evaluating bone structures and identifying any potential complications or structural abnormalities associated with nasal polyps. MRI scans are often employed when evaluating soft tissues, offering greater clarity in assessing the extent and potential spread of inflammation or infection.
- Audiometry: Evaluation of hearing is important as dizziness can sometimes be related to inner ear issues. Audiometry tests assess hearing sensitivity across various frequencies. Hearing loss can be a subtle indicator of an underlying problem that might contribute to the dizziness. For example, inner ear infections can lead to hearing loss and vertigo, often linked to dizziness.
Treatment Options for Nasal Polyps
Managing nasal polyps and associated dizziness requires a multifaceted approach. Treatment options vary depending on the severity of the condition and the presence of co-occurring issues.
- Medications: Nasal corticosteroids, like fluticasone and mometasone, are commonly prescribed to reduce inflammation and shrink the size of nasal polyps. These medications can be effective in alleviating symptoms, but their long-term use requires careful monitoring and consideration of potential side effects. For example, prolonged use of nasal sprays might lead to a decrease in the sense of smell.
- Surgical Procedures: Surgical removal of nasal polyps (polypectomy) is often considered for cases where medications are ineffective or when significant obstruction is present. This procedure involves carefully removing the polyps under local or general anesthesia. The effectiveness of surgery in alleviating dizziness directly depends on whether the dizziness is a consequence of nasal blockage.
- Other Interventions: In cases where underlying allergies or environmental factors contribute to nasal polyps, addressing these triggers through allergy management or environmental control can help reduce polyp recurrence. For example, avoidance of allergens and maintaining proper humidity levels can reduce the likelihood of polyp formation and recurrence.
Treatment Comparison Table
| Treatment Option | Effectiveness | Potential Side Effects | Typical Duration |
|---|---|---|---|
| Nasal Corticosteroids | Generally effective in reducing inflammation and polyp size | Potential for nasal dryness, irritation, or epistaxis (nosebleeds). Rarely, systemic side effects. | Ongoing, potentially lifelong, depending on the severity of the condition. |
| Polypectomy | Highly effective in removing polyps, often resulting in significant symptom improvement. | Potential for bleeding, infection, or scarring. Possible nasal discomfort or temporary loss of smell. | Recovery period varies depending on the extent of the procedure, typically several weeks. |
| Allergy Management | Effective in reducing polyp recurrence by addressing underlying causes. | Potential for allergic reactions to medications or environmental allergens. | Ongoing, potentially lifelong, to manage underlying allergies. |
Lifestyle Considerations
Managing nasal polyps and their associated dizziness requires a multifaceted approach, encompassing lifestyle adjustments that can help alleviate symptoms and promote overall well-being. Understanding how various lifestyle choices impact nasal inflammation and dizziness is crucial for developing a personalized management strategy. This section explores key lifestyle considerations to better understand how they might influence dizziness associated with nasal polyps.
Dietary Considerations
Dietary choices play a significant role in managing inflammation throughout the body, including the sinuses. Certain foods and dietary patterns may exacerbate nasal inflammation, potentially worsening dizziness. Conversely, some dietary approaches may help reduce inflammation and improve overall symptom control.A balanced diet rich in fruits, vegetables, and whole grains can contribute to a healthier immune system and potentially lessen inflammation.
Foods high in antioxidants, such as berries and leafy greens, may offer additional benefits. Avoiding processed foods, sugary drinks, and excessive intake of saturated fats is also recommended.
Environmental Factors
Environmental factors can significantly impact nasal inflammation and, consequently, dizziness. Exposure to irritants such as smoke, dust, and strong odors can trigger or worsen nasal congestion and inflammation. Maintaining a clean and well-ventilated environment, avoiding exposure to allergens, and using appropriate air purifiers can contribute to symptom relief.
Lifestyle Factors Impacting Dizziness
| Lifestyle Factor | Description | Potential Impact on Dizziness |
|---|---|---|
| Hydration | Maintaining adequate fluid intake. | Proper hydration can thin mucus, potentially reducing nasal congestion and associated dizziness. Dehydration can worsen nasal congestion, potentially leading to dizziness. |
| Stress Management | Practicing stress-reducing techniques like meditation, yoga, or deep breathing exercises. | Stress can exacerbate inflammation and worsen nasal symptoms. Effective stress management may contribute to improved symptom control and reduce dizziness. |
| Exercise | Regular physical activity, tailored to individual capabilities. | Regular exercise improves overall health, potentially boosting the immune system and reducing inflammation, potentially leading to reduced dizziness. Excessive or strenuous exercise may exacerbate existing symptoms. |
| Sleep Hygiene | Ensuring sufficient and quality sleep. | Adequate sleep is essential for the body’s natural repair and recovery processes, which may help reduce inflammation. Lack of sleep can contribute to increased inflammation and worsen symptoms, including dizziness. |
| Air Quality | Controlling indoor air quality, avoiding allergens, and using air purifiers. | Exposure to irritants like dust, smoke, or allergens can trigger or worsen nasal inflammation and associated dizziness. Maintaining a clean and well-ventilated environment can significantly improve symptoms. |
Case Studies and Examples
Understanding the connection between nasal polyps and dizziness requires looking at real-life scenarios. Case studies offer valuable insights into the diverse presentations and outcomes of this interplay. They highlight the importance of thorough diagnostic evaluations and personalized treatment plans.
Hypothetical Case Study 1: A Patient with Persistent Dizziness
A 35-year-old woman presented with a history of intermittent, worsening nasal congestion and facial pressure. She also reported experiencing frequent spells of dizziness, often accompanied by nausea and a feeling of imbalance. Physical examination revealed nasal polyps and signs of inflammation in the nasal passages. Further investigation, including imaging studies (CT scan or MRI), confirmed the presence of nasal polyps and their potential impact on the Eustachian tubes.
The patient’s dizziness was likely linked to the inflammation and pressure changes in her head and nasal cavity. The symptoms responded well to a combination of nasal steroid sprays and allergy management.
Hypothetical Case Study 2: A Different Presentation
A 60-year-old man with a history of chronic sinusitis presented with a gradual onset of dizziness, particularly during periods of physical exertion. He also reported a progressive loss of smell and taste, along with mild headaches. While nasal polyps were suspected, the presence of concurrent hearing loss and tinnitus prompted a comprehensive evaluation to rule out other possible causes of dizziness.
Experiencing dizzy spells alongside nasal polyps can be a real concern. While there’s no direct connection between shrinking nasal polyps and bunions, some natural remedies for managing bunions might surprisingly offer relief from the overall discomfort. For instance, exploring methods like those outlined in this guide on how to shrink bunions naturally might help to alleviate some of the general inflammation that could contribute to dizziness associated with nasal polyps.
Ultimately, it’s crucial to consult a doctor for a proper diagnosis and treatment plan for nasal polyps symptoms dizzy.
The imaging revealed significant nasal polyp growth and blockage of the Eustachian tubes. The combination of factors suggested a potential link between the nasal polyps, altered pressure within the inner ear, and the patient’s dizziness. Treatment focused on reducing inflammation, improving nasal airflow, and managing the patient’s symptoms.
Hypothetical Case Study 3: Diagnostic and Treatment Approaches
A 42-year-old female presented with a combination of symptoms including nasal blockage, postnasal drip, and episodic dizziness. Her medical history included a known allergy to dust mites. The initial evaluation involved a thorough physical examination, nasal endoscopy to visualize the polyps, and a hearing test to rule out inner ear involvement. Blood tests and allergy testing further narrowed down the potential causes.
The diagnosis confirmed the presence of nasal polyps and suspected connection to the patient’s symptoms. Treatment involved a multifaceted approach including allergy management with medications, nasal steroid sprays, and possible surgical removal of the polyps. Regular follow-up visits were scheduled to monitor the patient’s progress and adjust the treatment plan as needed.
Summary Table of Case Studies
| Case Study | Symptoms | Diagnosis | Treatment |
|---|---|---|---|
| 1: Persistent Dizziness | Nasal congestion, facial pressure, frequent dizziness, nausea, imbalance | Nasal polyps, inflammation, potential Eustachian tube impact | Nasal steroid sprays, allergy management |
| 2: Different Presentation | Chronic sinusitis, gradual dizziness (exertion-related), loss of smell/taste, mild headaches, hearing loss, tinnitus | Nasal polyps, blocked Eustachian tubes, possible inner ear pressure changes | Inflammation reduction, improved nasal airflow, symptom management |
| 3: Diagnostic & Treatment | Nasal blockage, postnasal drip, episodic dizziness, dust mite allergy | Nasal polyps, suspected connection to symptoms, allergy confirmation | Allergy management, nasal steroid sprays, possible polyp removal, follow-up monitoring |
Differentiating Nasal Polyp Symptoms from Other Conditions
Nasal polyps, while often associated with chronic nasal congestion, can sometimes present with dizziness, making accurate diagnosis crucial. Differentiating nasal polyp symptoms from those of other conditions requires careful evaluation of the complete clinical picture. This involves understanding the potential interplay between nasal polyps and other common causes of dizziness.Identifying the precise cause of dizziness is paramount for effective management.
Many conditions can mimic the symptoms of nasal polyps, including sinus infections, allergies, and even certain neurological issues. A comprehensive evaluation that considers the patient’s medical history, physical examination findings, and diagnostic tests is vital for distinguishing nasal polyps from other potential causes.
Comparison of Symptoms
Understanding the nuances of symptom presentation is critical for distinguishing nasal polyps from other conditions. Different conditions often have unique symptom profiles, providing clues for accurate diagnosis.
- Nasal Polyps: Nasal polyps often manifest as persistent nasal congestion, difficulty breathing through the nose, facial pressure, and a feeling of fullness in the ears. These symptoms can sometimes be accompanied by a postnasal drip and occasional headaches. Dizziness, if present, is often a secondary effect related to the underlying nasal blockage. The onset of symptoms is typically gradual and chronic.
- Sinus Infections: Sinus infections, commonly known as sinusitis, typically cause facial pain, pressure, and tenderness around the sinuses. Symptoms often include a thick, discolored nasal discharge, fever, and body aches. Dizziness is less common with sinusitis but can occur due to associated inflammation or secondary infections.
- Allergies: Allergies can trigger a variety of symptoms, including sneezing, runny nose, itchy eyes, and congestion. Dizziness, though possible, is not a typical allergy symptom. Symptoms related to allergies are often triggered by exposure to specific allergens.
Diagnostic Approaches
Different diagnostic approaches are employed to distinguish nasal polyps from other conditions. The process typically involves a comprehensive evaluation.
- Physical Examination: A physical examination of the nose and sinuses is a critical first step. The examination allows for direct visualization of nasal passages and potential polyps. This examination can also help in identifying the presence of any other contributing factors.
- Imaging Studies: Imaging techniques, such as CT scans or X-rays, can help visualize the structures of the nasal passages and sinuses, enabling the detection of nasal polyps and potential complications. These studies are often crucial for evaluating the extent and location of the nasal polyps.
- Allergy Testing: Allergy testing may be necessary if allergies are suspected as a contributing factor to the symptoms. These tests help identify specific allergens that might be triggering the symptoms.
Symptom Comparison Table
This table summarizes the key differences in symptoms, causes, and treatments for nasal polyps, sinus infections, and allergies, along with potential dizziness associations.
| Condition | Symptoms | Causes | Treatment |
|---|---|---|---|
| Nasal Polyps | Chronic nasal congestion, breathing difficulties, facial pressure, postnasal drip, occasional headaches, possible dizziness | Inflammation of the nasal lining, genetic predisposition, environmental factors | Surgical removal (polypectomy), medication to reduce inflammation |
| Sinus Infections | Facial pain, pressure, tenderness around sinuses, thick nasal discharge, fever, body aches, possible dizziness | Viral, bacterial, or fungal infections | Antibiotics (bacterial infections), pain relievers, nasal sprays |
| Allergies | Sneezing, runny nose, itchy eyes, congestion, possible dizziness (less common) | Exposure to allergens (pollen, dust mites, pet dander) | Allergy medications, avoidance of allergens, immunotherapy |
Illustrative Examples and Visualizations
Understanding nasal polyps and their potential link to dizziness requires a visual approach. This section provides illustrative examples to better grasp the physical presence of polyps, their impact on the nasal passages and balance, and the effects of congestion on blood flow. Visualizations will enhance comprehension and help distinguish the symptoms from other conditions.
Nasal Polyp Appearance and Impact
Nasal polyps are benign growths that develop within the lining of the nasal passages. They typically appear as smooth, pale, and often teardrop-shaped masses. Their size can vary significantly, from small, barely noticeable protrusions to large, obstructing growths. The size and location of the polyps directly impact the nasal cavity. For instance, large polyps can block the nasal airflow, leading to a sensation of stuffiness, difficulty breathing through the nose, and even sinus pressure.
This blockage can also cause a reduced sense of smell. Visualize a teardrop-shaped, pale mass growing within the intricate network of the nasal passages, potentially obstructing the airflow through the nostrils.
Visualizing the Impact on the Balance System
While nasal polyps themselves do not directly affect the balance system, their presence can indirectly impact balance through the effect of congestion. Nasal congestion can cause pressure changes in the sinuses, which, in turn, may influence the inner ear, potentially affecting the balance organs. This indirect influence can lead to feelings of dizziness or lightheadedness. Imagine a congested nasal cavity, where the air pressure is not consistent throughout the sinus cavity.
This pressure imbalance may affect the delicate structures within the inner ear, causing a disruption in the balance system.
Nasal Congestion’s Effect on Blood Flow and Oxygenation
Nasal congestion significantly reduces airflow and thus oxygen intake through the nose. This can lead to a decrease in oxygenated blood reaching the brain. Imagine a highway (blood vessels) with traffic (blood flow) being slowed or stopped by a construction site (nasal congestion). This reduced oxygenation can lead to symptoms like dizziness, headaches, and a general feeling of fatigue.
A visual representation of this would show the nasal cavity with reduced air intake, which would result in less oxygenated blood flowing to the brain.
Diagnostic Process Visualization
The diagnostic process for nasal polyps involves a series of steps, which can be visualized as a flowchart. First, a medical history is taken, followed by a physical examination, including nasal endoscopy. Nasal endoscopy involves inserting a thin, flexible tube with a camera into the nasal passages to visualize the interior and identify any abnormalities. This is often followed by imaging tests, such as CT scans or MRI scans, to provide detailed images of the nasal structures and surrounding tissues.
These images can confirm the presence and extent of polyps. A simple diagram showing a patient’s head with a nasal endoscope and subsequent CT/MRI scans would visually illustrate this process.
End of Discussion
In conclusion, nasal polyps and dizziness are often interconnected. Understanding the diverse symptoms, potential causes, and diagnostic methods is vital for effective management. This guide offers valuable insights into the connection between these conditions, providing readers with the knowledge needed to navigate this challenging health issue. Remember, this information is for educational purposes only and should not replace professional medical advice.
Consult with a healthcare provider for proper diagnosis and treatment.