Asymptomatic definition importance and controversy is a complex and crucial aspect of public health. Understanding how we define the absence of symptoms is essential for effective disease prevention and control strategies. This multifaceted issue involves diverse perspectives, ranging from medical definitions to public health implications, ethical considerations, and practical challenges in identification.
Different medical and public health contexts use varying criteria to define asymptomatic disease. This often leads to conflicting interpretations and challenges in managing outbreaks. The importance of accurate definitions becomes critical in determining the extent of transmission and implementing appropriate public health interventions.
Defining Asymptomatic Disease
Asymptomatic disease poses a unique challenge in public health. Understanding how to define and identify these conditions is crucial for effective disease surveillance, prevention, and treatment. The absence of symptoms can obscure the presence of a disease, making early detection and intervention more difficult. This necessitates nuanced definitions that account for the diverse contexts and populations affected.
Defining Asymptomatic Disease in Different Contexts
The concept of asymptomatic disease is interpreted differently across medical and public health contexts. In medicine, the focus is often on the individual patient, identifying the presence of a disease despite the absence of noticeable symptoms. Public health, however, frequently considers asymptomatic individuals as potential disease carriers, emphasizing the epidemiological impact of the disease. This difference in focus necessitates distinct criteria for defining asymptomatic disease in each context.
Challenges in Defining Asymptomatic Disease Across Populations and Conditions
Defining asymptomatic disease across various populations and conditions presents several challenges. The absence of symptoms can vary depending on the individual’s age, underlying health conditions, and the specific disease. Additionally, some diseases may exhibit different symptom profiles in different populations, making it difficult to establish consistent criteria. Moreover, the sensitivity and specificity of diagnostic tests can influence how asymptomatic disease is defined and diagnosed.
Table Comparing and Contrasting Definitions of Asymptomatic Disease
| Definition Type | Criteria | Examples | Limitations |
|---|---|---|---|
| Medical | Presence of detectable disease markers (e.g., elevated blood pressure, abnormal lab results, imaging abnormalities) in the absence of noticeable symptoms. Often relies on diagnostic tests or screening. | A person with elevated liver enzymes indicating liver disease, but no jaundice or other symptoms. A person with a positive antibody test for a specific virus but no fever or cough. | May not capture all forms of asymptomatic disease. Diagnostic tests may not always be available or reliable. |
| Public Health | Presence of disease markers or potential infectious agents capable of transmission, even without apparent symptoms. Focuses on the potential for disease spread within a population. | A person carrying a virus that can be transmitted through respiratory droplets, despite not exhibiting symptoms. A person with an undiagnosed chronic disease that is still capable of spreading the infection. | Can be difficult to distinguish between true asymptomatic carriers and individuals who are pre-symptomatic. May overestimate the risk of transmission in some cases. |
Importance of Asymptomatic Disease Recognition
Identifying and understanding asymptomatic disease is crucial for effective disease prevention and control. Often, individuals harboring the infection show no outward symptoms, making them seemingly healthy carriers. This hidden reservoir significantly impacts transmission dynamics and necessitates proactive public health strategies. This blog post will delve into the significance of recognizing asymptomatic disease, exploring its impact on disease transmission, and the implications for public health interventions.
Significance in Disease Prevention and Control
Recognizing asymptomatic disease is paramount in preventing outbreaks and containing the spread of infectious agents. Early detection and isolation of asymptomatic individuals can interrupt transmission chains before significant community-wide outbreaks occur. The early intervention strategy minimizes the risk of secondary infections and subsequent healthcare burdens. For instance, the early detection of asymptomatic individuals infected with SARS-CoV-2 in the early stages of the pandemic could have significantly altered the trajectory of the disease.
Role in Disease Transmission Dynamics
Asymptomatic individuals play a vital role in disease transmission. They can unknowingly transmit the pathogen to susceptible individuals, leading to further infections. Mathematical models often illustrate how asymptomatic carriers can contribute substantially to the overall disease burden. The rate of transmission from asymptomatic individuals can vary considerably depending on the specific pathogen and the mode of transmission.
Defining asymptomatic conditions is crucial, but often fraught with debate. Take guinea worm disease, or dracunculiasis, for example. Guinea worm disease dracunculiasis presents a fascinating case study, where the initial lack of symptoms makes diagnosis and treatment challenging. Ultimately, the importance of an accurate asymptomatic definition remains a key area of ongoing discussion in medical research.
For example, a respiratory pathogen may have a higher rate of transmission through respiratory droplets than a pathogen transmitted primarily through contact.
Implications for Public Health Interventions
The presence of asymptomatic cases significantly impacts public health interventions. Public health strategies need to be adapted to account for the potential for transmission from asymptomatic individuals. This necessitates a shift towards comprehensive surveillance strategies that include testing asymptomatic populations, especially in high-risk settings. The development of effective strategies for identifying asymptomatic individuals often involves deploying rapid diagnostic tools, expanding testing capacity, and optimizing contact tracing protocols.
These measures are crucial for reducing transmission and controlling outbreaks.
Impact on Disease Control Strategies: A Flowchart
 The flowchart illustrates the impact of asymptomatic disease recognition on disease control strategies. It begins with the identification of an asymptomatic case. Subsequent steps include the isolation of the individual, contact tracing, testing of contacts, and monitoring of public health measures. The flowchart concludes with the evaluation of the effectiveness of the interventions in reducing the spread of the disease. The identification of asymptomatic cases and the subsequent implementation of public health interventions often leads to a decrease in the transmission rate and helps to contain the outbreak.
The flowchart illustrates the impact of asymptomatic disease recognition on disease control strategies. It begins with the identification of an asymptomatic case. Subsequent steps include the isolation of the individual, contact tracing, testing of contacts, and monitoring of public health measures. The flowchart concludes with the evaluation of the effectiveness of the interventions in reducing the spread of the disease. The identification of asymptomatic cases and the subsequent implementation of public health interventions often leads to a decrease in the transmission rate and helps to contain the outbreak.
Controversies Surrounding Asymptomatic Disease
The concept of asymptomatic disease, while crucial for public health, has ignited significant controversies. Defining who is “asymptomatic” and how to manage those individuals with no apparent symptoms has sparked heated debates, particularly in the context of infectious diseases. Different stakeholders have varying interests and perspectives, leading to a complex landscape of arguments for and against different approaches.The management of asymptomatic individuals hinges on balancing public health protection with individual liberties.
Defining asymptomatic conditions is crucial but often fraught with debate. The line between truly asymptomatic and simply undiagnosed can be blurry, especially in complex cases. This is particularly relevant when considering drugs like amiodarone, which, while uniquely effective at controlling certain heart rhythms, carries a significant risk of severe side effects, as discussed in this article amiodarone uniquely effective but uniquely toxic.
Ultimately, a clear understanding of asymptomatic conditions remains essential for both diagnosis and treatment.
The potential for widespread transmission, even in the absence of visible symptoms, necessitates measures to control the spread. However, restrictions on asymptomatic individuals raise concerns about the impact on daily life, economic activity, and social well-being.
Testing Strategies
Effective testing strategies are essential for identifying and managing asymptomatic cases. However, the optimal approach to testing is contentious. Factors like the cost-effectiveness, availability of tests, and potential for false positives all play a role in shaping the debate. A key concern is the potential for widespread testing to overwhelm healthcare systems, especially in the face of limited resources.
This is particularly relevant when dealing with diseases like COVID-19, where the need for rapid and large-scale testing is paramount.
Quarantine Policies
Quarantine policies aimed at preventing the spread of asymptomatic disease are frequently debated. The efficacy of quarantine in reducing transmission is a subject of ongoing research and discussion. Different quarantine approaches have varying levels of restrictiveness, which directly impact individuals’ freedom of movement and social interactions. The potential for economic disruption and social isolation associated with quarantine measures also needs careful consideration.
For example, during the COVID-19 pandemic, the debate about quarantine policies for asymptomatic individuals often centered around the balance between protecting public health and minimizing the negative consequences for individuals and society.
Stakeholder Perspectives
Several stakeholders have differing perspectives on the management of asymptomatic disease. Public health officials often prioritize the collective well-being and aim to minimize transmission. Individuals, on the other hand, may prioritize their own autonomy and freedom from restrictions. Businesses and economic sectors are also concerned about the potential impact of testing and quarantine policies on their operations.
The varying interests of these stakeholders often lead to conflicting priorities and approaches to managing asymptomatic disease.
Arguments For and Against Different Approaches
- Approach: Increased Surveillance and Testing for Asymptomatic Individuals
- Arguments For: Early detection and isolation of asymptomatic carriers can help prevent further spread, reducing the overall burden of disease. This strategy can be particularly crucial in controlling highly contagious diseases, allowing for timely interventions.
- Arguments Against: Widespread testing can be costly and logistically challenging, potentially overwhelming healthcare systems. The potential for false positives can lead to unnecessary anxiety and restrictions.
- Approach: Focused Testing and Targeted Quarantine for High-Risk Individuals
- Arguments For: This approach can target individuals who are more likely to transmit the disease, maximizing the benefit of interventions while minimizing disruption for the wider population.
- Arguments Against: Identifying high-risk individuals may be challenging, potentially missing individuals who are unknowingly transmitting the disease.
Examples of Controversies
During the COVID-19 pandemic, several controversies arose regarding the management of asymptomatic cases. The debate about widespread testing for asymptomatic individuals, quarantine policies, and the economic implications of these measures highlighted the complexities involved. Specific examples include differing opinions on the necessity of mandatory mask-wearing for asymptomatic individuals in public settings.
Methods for Identifying Asymptomatic Cases
Identifying asymptomatic cases is crucial for effective disease management and prevention. Accurate detection of individuals harboring the disease without exhibiting symptoms allows for timely interventions, limiting transmission and potential complications. This is particularly important for diseases with long incubation periods or those with mild, non-specific symptoms. Early detection allows for prompt isolation, contact tracing, and treatment, potentially preventing further spread and severe outcomes.Various methods are employed to identify asymptomatic individuals, each with its own strengths and weaknesses.
These methods range from simple screening tools to advanced diagnostic technologies, enabling a comprehensive approach to disease surveillance. Understanding the accuracy and limitations of each method is essential for making informed decisions regarding disease management.
Screening Tools
Early detection often relies on simple screening tools that can identify individuals at risk. These tools are typically cost-effective and accessible, allowing for large-scale population screening. Examples include questionnaires, self-assessment tools, and simple physical examinations. These preliminary screenings can flag individuals who may require further investigation with more advanced diagnostic methods. The accuracy of these screening tools varies significantly depending on the specific disease and the characteristics of the population being screened.
For instance, a well-designed questionnaire for influenza-like symptoms can help identify individuals at risk of influenza, but it’s not a definitive diagnosis.
Diagnostic Tools and Technologies
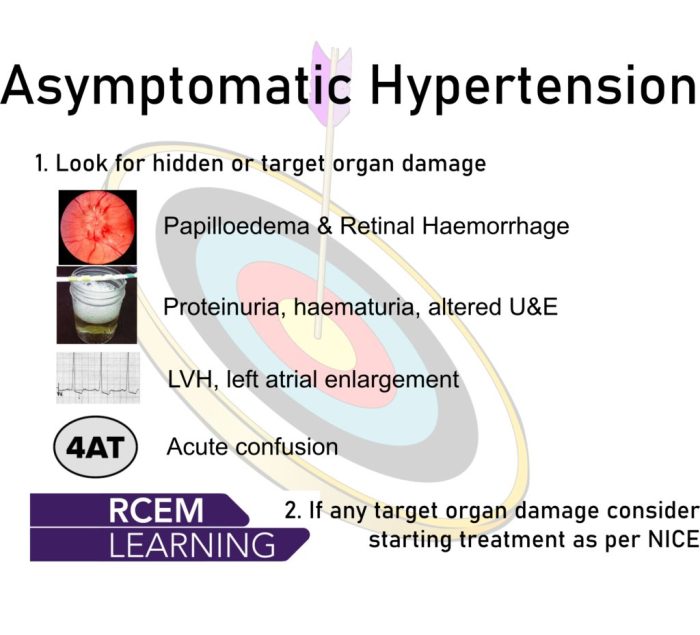
Advanced diagnostic tools and technologies play a vital role in identifying asymptomatic cases. These methods often involve laboratory tests or imaging techniques. Examples include polymerase chain reaction (PCR) tests for detecting viral genetic material, serological tests for identifying antibodies, and imaging techniques like X-rays or CT scans for detecting organ damage or abnormalities. The choice of diagnostic tool depends on the specific disease and the available resources.
For instance, PCR tests are highly sensitive and specific for detecting the presence of viral RNA, making them valuable for identifying asymptomatic individuals infected with viruses like SARS-CoV-2.
Accuracy and Limitations of Different Methods, Asymptomatic definition importance and controversy
The accuracy of a diagnostic method is a critical factor in its utility for identifying asymptomatic cases. Accuracy is typically measured by sensitivity (the ability to correctly identify individuals with the disease) and specificity (the ability to correctly identify individuals without the disease). However, different methods have different limitations. For example, while PCR tests are highly sensitive, they may yield false-positive results if contaminated samples are used.
Similarly, serological tests may not be accurate in the early stages of infection, and imaging techniques may not detect subtle abnormalities in asymptomatic individuals.
Summary Table of Identification Methods
| Method | Description | Accuracy | Limitations |
|---|---|---|---|
| Questionnaires/Self-Assessments | Identify individuals at risk based on symptoms or risk factors. | Moderate to High (depending on the tool) | May not identify all cases, susceptible to false positives/negatives. |
| Polymerase Chain Reaction (PCR) | Detects viral genetic material. | High sensitivity and specificity | Potential for false positives with contaminated samples, may not detect early stages of infection. |
| Serological Tests | Detects antibodies. | Variable, depends on the disease and stage of infection | May not be accurate in early stages, may show false positives if exposed to similar pathogens. |
| Imaging Techniques (e.g., X-rays, CT scans) | Identifies structural abnormalities. | Variable, depending on the disease and the severity | May not detect subtle abnormalities in asymptomatic individuals, expensive, may require specialized personnel. |
Impact of Asymptomatic Disease on Public Health
The presence of asymptomatic disease dramatically alters public health strategies. Traditional approaches, often focused on symptomatic individuals, are insufficient when a significant portion of the population harbors the infection without exhibiting any noticeable illness. This necessitates a shift in our understanding and response to disease outbreaks. The challenge lies in identifying and controlling the spread of infection before individuals develop symptoms, impacting everything from contact tracing to preventative measures.The impact of asymptomatic disease on public health strategies is multifaceted.
Defining asymptomatic conditions is crucial, but also surprisingly tricky. The debate around what constitutes “asymptomatic” often hinges on our understanding of the very nature of disease. This directly impacts treatment decisions and research priorities. For example, exploring the the history of surgery timeline reveals how our understanding of disease and treatment has evolved. This evolution underscores the constant need for a nuanced definition of asymptomatic, reflecting the dynamic relationship between symptoms and disease progression.
Public health measures must adapt to address the unseen spread of infection. Traditional models of disease transmission, often relying on symptomatic cases, become less effective when a substantial portion of the population is infected without symptoms. This means traditional contact tracing strategies, while valuable, may miss crucial transmission chains. Public health responses must evolve to consider the silent spread of infection and to proactively identify and manage the risks associated with asymptomatic carriers.
Challenges in Implementing Public Health Measures
Implementing effective public health measures to address asymptomatic disease presents several challenges. First, accurate identification of asymptomatic cases is crucial, but diagnostic tools and testing capacities may be limited, particularly during outbreaks. Second, public understanding and compliance with measures targeting asymptomatic individuals are often low. People may be less motivated to adhere to isolation or quarantine protocols if they do not feel ill.
Third, tracing asymptomatic carriers can be significantly more complex than tracing symptomatic ones. This requires extensive surveillance, robust testing strategies, and the ability to effectively isolate and manage asymptomatic individuals. Finally, the resources needed to manage asymptomatic individuals, including testing, isolation, and potential treatment, can be substantial, especially during widespread outbreaks.
Adapting Public Health Policies and Interventions
Public health policies and interventions need substantial adaptation to accommodate asymptomatic disease. Strategies for contact tracing must be revised to include asymptomatic individuals. Enhanced surveillance systems are necessary to detect and track asymptomatic cases. This may involve increased testing capacity, innovative surveillance methods, and the integration of data from various sources. The development of effective communication strategies to educate the public about the importance of preventative measures is crucial.
This includes clear messaging about the risks of asymptomatic transmission and the significance of compliance with public health guidelines, such as mask-wearing and social distancing. Furthermore, proactive measures, such as community-based screening programs, should be considered. These programs aim to identify asymptomatic cases and interrupt transmission chains before widespread community outbreaks.
Real-World Case Studies
Several real-world case studies demonstrate the importance of adapting public health responses to account for asymptomatic transmission. For example, the 2009 H1N1 influenza pandemic saw asymptomatic individuals play a significant role in the spread of the virus. Public health officials struggled to manage the unseen transmission pathways, highlighting the need for expanded surveillance and testing strategies. Similarly, the SARS-CoV-2 pandemic emphasized the crucial role of asymptomatic transmission in driving outbreaks.
Early responses, often focused on symptomatic cases, were hampered by the inability to effectively manage asymptomatic spread. These experiences underscore the need for proactive measures and comprehensive surveillance systems to effectively combat diseases with significant asymptomatic transmission. This includes adjusting strategies to anticipate and mitigate the risk of outbreaks by focusing on identifying and controlling asymptomatic spread.
Ethical Considerations in Handling Asymptomatic Disease
Navigating the complexities of asymptomatic disease requires a delicate balance between public health interventions and individual rights. The potential for widespread transmission coupled with the absence of obvious symptoms presents a unique set of ethical dilemmas, demanding careful consideration of informed consent, privacy, and potential conflicts of interest. This discussion will explore these critical aspects.The management of asymptomatic individuals presents a fundamental ethical challenge.
How do we weigh the need to protect the wider community against the rights and autonomy of asymptomatic individuals? This delicate balance necessitates a nuanced approach that considers both public health imperatives and individual liberties.
Public Health Interventions Targeting Asymptomatic Individuals
Public health interventions, such as mandatory testing and isolation measures for asymptomatic individuals, raise profound ethical concerns. These interventions can significantly impact an individual’s personal and professional life, potentially causing substantial economic and social disruption. For example, widespread mandatory testing could lead to undue financial burdens for individuals and potentially exacerbate existing societal inequalities. Furthermore, the potential for discrimination and stigmatization based on perceived risk associated with asymptomatic status necessitates careful consideration.
A just and equitable approach is crucial.
Conflicts of Interest in Dealing with Asymptomatic Disease
Potential conflicts of interest exist in the management of asymptomatic disease. Financial incentives, political pressures, and personal biases can influence decision-making regarding testing protocols, treatment strategies, and resource allocation. For instance, the development of new diagnostic tests or treatments might be driven by commercial interests, potentially prioritizing profit over public health needs. These conflicts require careful scrutiny and transparent decision-making processes.
Informed Consent and Privacy in Managing Asymptomatic Cases
Ensuring informed consent and protecting the privacy of asymptomatic individuals is paramount. Individuals must be fully informed about the nature of the tests, the potential risks and benefits, and the intended use of their data. Strict adherence to data privacy regulations is crucial to prevent the misuse or unauthorized disclosure of sensitive health information. A strong ethical framework should guide the collection, storage, and use of data associated with asymptomatic cases, upholding the principles of confidentiality and anonymity whenever possible.
Furthermore, transparent communication channels and clear guidelines regarding data usage should be established to build public trust.
Examples of Ethical Dilemmas
A hypothetical scenario illustrates a complex ethical dilemma. Imagine a highly contagious but mild asymptomatic disease affecting a large population. Public health authorities face the choice between widespread testing, which could significantly disrupt daily life and potentially lead to stigma, and a more limited approach. The decision requires balancing the need for public health protection with individual autonomy and the potential for economic hardship.
Decisions must be made thoughtfully, ethically, and transparently, considering all potential consequences.
Ending Remarks: Asymptomatic Definition Importance And Controversy
In conclusion, the asymptomatic definition importance and controversy highlights the intricate interplay between medical science, public health, and ethical considerations. The challenges in defining, identifying, and managing asymptomatic cases necessitate ongoing research, discussion, and adaptable strategies. Ultimately, effective public health responses require a nuanced understanding of the implications of asymptomatic disease and a willingness to adapt to evolving scientific knowledge and societal needs.