The gallbladder anatomy function and treatment is a crucial topic for understanding digestive health. This exploration delves into the gallbladder’s role in the human body, from its intricate structure to the various disorders that can affect it. We’ll cover everything from its location and function in the digestive process to the different treatment options available for gallbladder problems.
Understanding the gallbladder’s anatomy is key to grasping its role in bile storage and release. Its shape, size, and position within the abdomen are critical factors in how it interacts with other organs. The gallbladder concentrates bile, a crucial component of fat digestion, and its proper functioning is essential for overall health. This discussion will also highlight common gallbladder disorders, their causes, and the available treatments.
Gallbladder Anatomy
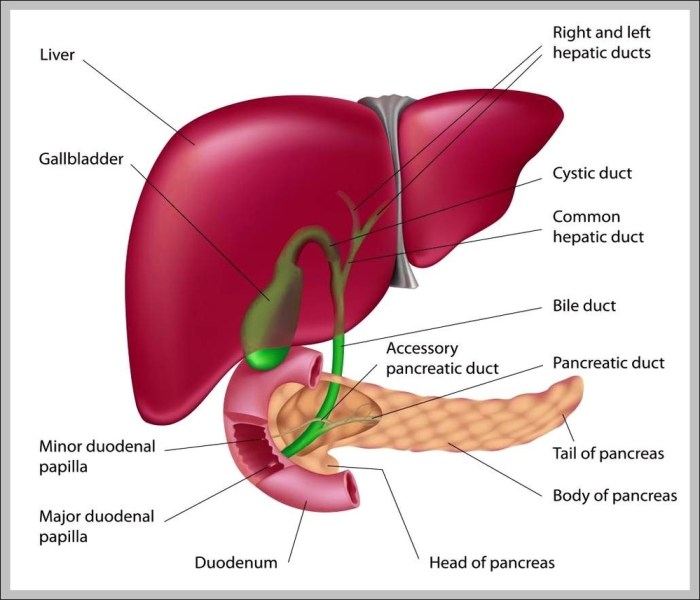
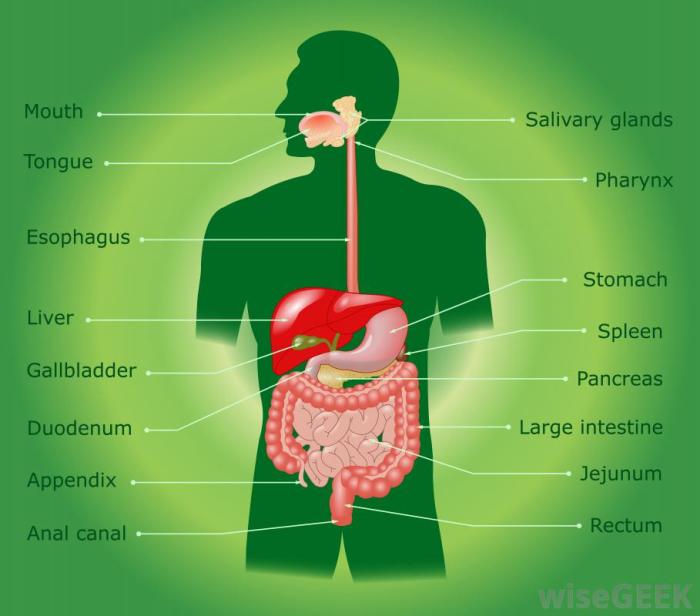
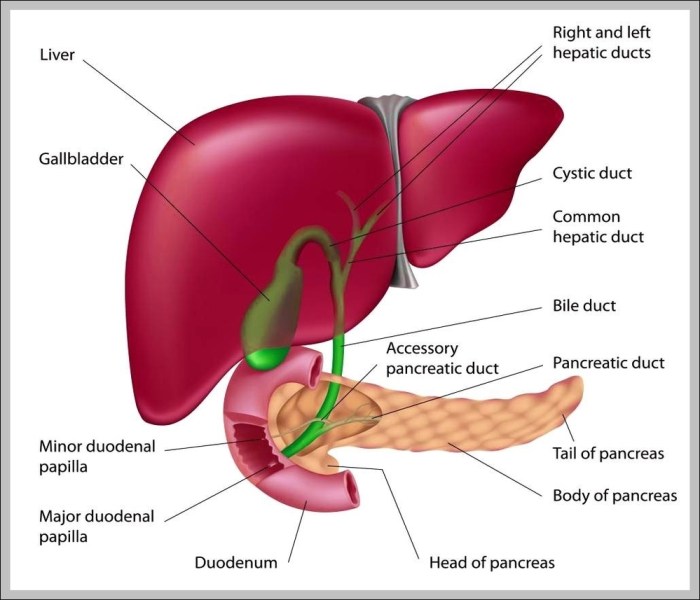
The gallbladder, a small, pear-shaped organ, plays a crucial role in the digestive process. Understanding its location, structure, and relationship to other organs is vital for comprehending its function and potential issues. This section delves into the detailed anatomy of the gallbladder.The gallbladder is situated beneath the liver, nestled in a shallow depression on its inferior surface. Its position, relative to other abdominal organs, allows it to efficiently collect and concentrate bile produced by the liver.
Gallbladder Location
The gallbladder rests in a fossa, a shallow depression, on the inferior surface of the liver. Its head points toward the right side of the body, while the tail curves slightly downward and toward the midline. The gallbladder is positioned in close proximity to the duodenum, a part of the small intestine. This anatomical arrangement allows bile to travel directly from the gallbladder to the duodenum when needed.
Gallbladder Structure
The gallbladder is a hollow, muscular organ, roughly 7-10 cm long and 3-4 cm wide. Its shape resembles a pear, with a wider, rounded fundus (the bottom portion), a narrow neck, and a body connecting the two. The fundus typically extends slightly beyond the liver’s edge. Its walls are relatively thin, composed of smooth muscle fibers that contract to release bile.
A mucous membrane lines the inner surface, allowing for the storage and movement of bile.
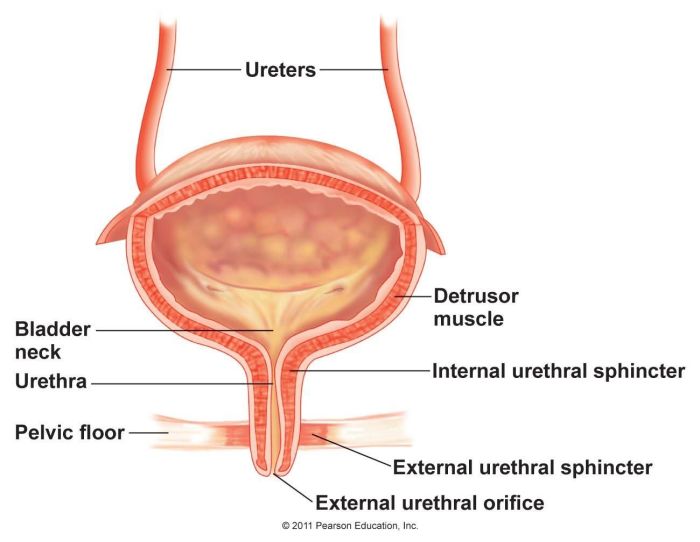
Gallbladder Wall Layers, The gallbladder anatomy function and treatment
The gallbladder wall consists of three distinct layers:
- The outer serosa, a thin layer of connective tissue, is the outermost layer. It provides protection and helps to hold the gallbladder in place. It’s a vital component of the peritoneum, the membrane that lines the abdominal cavity.
- The middle muscularis layer is comprised of smooth muscle fibers. These fibers contract to propel bile into the cystic duct. The strength of these contractions is essential for efficient bile release.
- The inner mucosa is a thin layer of epithelium, highly folded to increase surface area. This structure is important for the absorption of water from the bile and maintaining the consistency of the bile while it is stored in the gallbladder.
Dimensions and Shape Comparison
The following table compares the dimensions and shape of the gallbladder with other related organs.
| Organ | Dimensions (approximate) | Shape |
|---|---|---|
| Gallbladder | 7-10 cm long, 3-4 cm wide | Pear-shaped |
| Liver | 12-15 cm long, 7-8 cm wide | Irregularly lobed |
| Common Bile Duct | 5-10 mm in diameter | Tube-like |
Visual Representation
Imagine the liver as a large, reddish-brown, irregular-shaped organ dominating the upper right quadrant of the abdomen. Beneath it, tucked into a shallow depression, is the gallbladder. Its pear shape is clearly visible, with the wider fundus extending slightly beyond the liver’s edge. The neck of the gallbladder connects to the cystic duct, which then merges with the common bile duct.
This duct leads to the duodenum, where bile aids in the digestion of fats. The gallbladder’s position allows for efficient storage and release of bile into the small intestine.
Gallbladder Function
The gallbladder, a small pear-shaped organ nestled beneath the liver, plays a crucial role in the digestive process. It acts as a temporary storage reservoir for bile, a fluid produced by the liver essential for breaking down fats in the small intestine. Understanding its function is vital for comprehending how our bodies efficiently process nutrients.The gallbladder’s primary function is not to produce bile, but to concentrate and store it.
This allows for a controlled release of bile into the small intestine precisely when needed, maximizing its effectiveness in fat digestion. This process is tightly regulated, ensuring that the right amount of bile is available at the right time.
Bile Storage and Concentration
The liver constantly produces bile, which drains into the common bile duct. This duct leads to the gallbladder, where bile is temporarily stored. Inside the gallbladder, specialized cells absorb water and electrolytes from the bile, effectively concentrating it. This concentration process significantly increases the bile’s potency in breaking down fats, ensuring optimal efficiency in the digestive process.
The concentrated bile is stored until stimulated by the presence of fats in the duodenum. This process allows for the controlled release of concentrated bile, optimizing its effect.
Bile Release into the Small Intestine
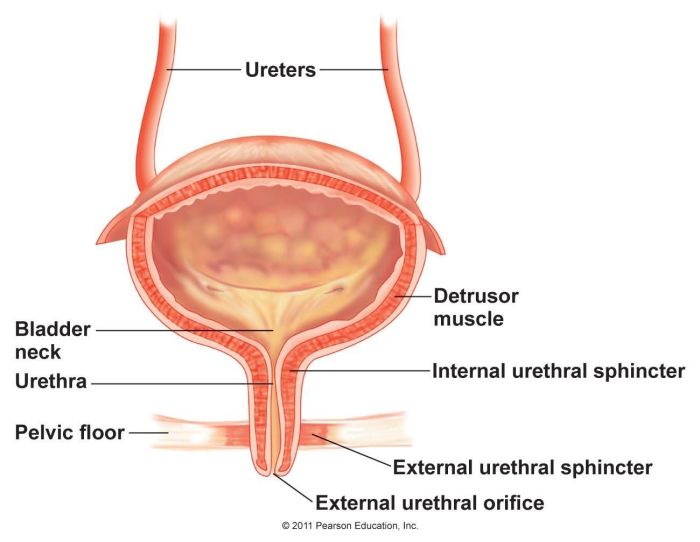
The gallbladder’s release of bile is triggered by the presence of fats in the duodenum, the first part of the small intestine. This triggers the release of cholecystokinin (CCK), a hormone. CCK signals the gallbladder to contract, pushing the concentrated bile into the common bile duct. The sphincter of Oddi, a muscular valve at the junction of the common bile duct and the duodenum, relaxes, allowing the bile to flow into the small intestine.
Understanding the gallbladder’s role in digestion is crucial – it stores and releases bile, essential for breaking down fats. Different treatments for gallbladder issues range from lifestyle changes to surgery. However, sometimes, medication choices like comparing the effectiveness of Tegretol and Lamictal in managing certain conditions are important. For a deeper dive into the nuances of tegretol vs lamictal how do they differ , explore the detailed analysis on their respective benefits and potential side effects.
Ultimately, proper gallbladder function is vital for overall health and well-being.
This precise mechanism ensures that bile is released only when needed, optimizing fat digestion.
Importance of Bile in Fat Digestion and Absorption
Bile plays a vital role in the digestion and absorption of fats. It emulsifies fats, breaking them down into smaller droplets, increasing the surface area exposed to digestive enzymes. This process makes it much easier for the enzymes to break down the fats into fatty acids and glycerol, which can then be absorbed into the bloodstream. Without bile, fat digestion would be significantly impaired, leading to malabsorption of essential nutrients.
This is crucial for the body to utilize fats for energy, hormone production, and cell function.
Bile Secretion, Storage, and Release Flowchart
The following flowchart illustrates the process of bile secretion, storage, and release:
| Step | Description |
|---|---|
| 1 | Liver produces bile. |
| 2 | Bile flows into the common bile duct. |
| 3 | Bile enters the gallbladder for storage. |
| 4 | Fats enter the duodenum. |
| 5 | Cholecystokinin (CCK) is released. |
| 6 | Gallbladder contracts, releasing bile. |
| 7 | Sphincter of Oddi relaxes. |
| 8 | Bile enters the small intestine. |
| 9 | Bile emulsifies fats, aiding digestion and absorption. |
Gallbladder Disorders
The gallbladder, a small, pear-shaped organ, plays a crucial role in fat digestion. However, various disorders can affect its function and health. Understanding these disorders is vital for recognizing symptoms and seeking appropriate medical care. Gallbladder issues, ranging from relatively benign gallstones to more severe cholecystitis, can significantly impact a person’s quality of life.Gallbladder disorders encompass a spectrum of conditions, from the relatively common presence of gallstones to the more serious inflammation of the gallbladder known as cholecystitis.
These conditions can lead to discomfort, pain, and, in some cases, require surgical intervention. Identifying the specific type of disorder and its underlying cause is essential for effective treatment.
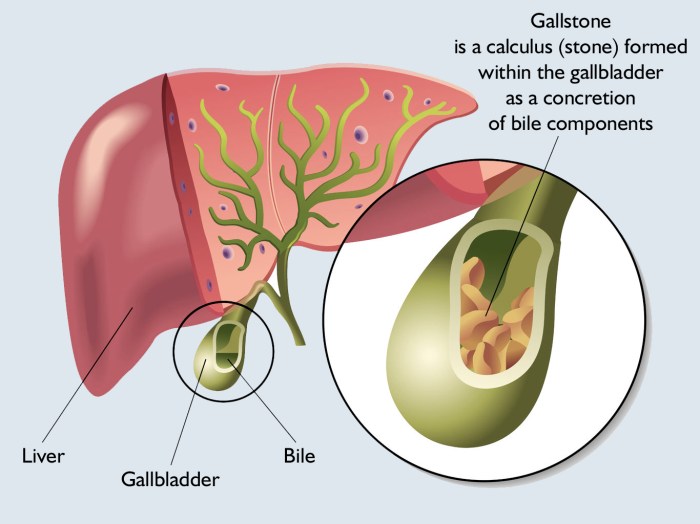
Gallstones
Gallstones are hardened deposits that form within the gallbladder. These stones can vary in size and composition, impacting their potential for causing symptoms. A variety of factors contribute to their formation.Common causes of gallstones include imbalances in the bile’s chemical composition, such as an excess of cholesterol or bilirubin. Certain lifestyle factors, such as obesity, rapid weight loss, and a diet high in fat, can also increase the risk.
Understanding gallbladder function, from its anatomy to potential treatments, is crucial for overall health. A healthy gallbladder helps process fats in our diet, but sometimes issues arise. Interestingly, a balanced diet, like the one often recommended by a high protein vanilla matcha latte dietitian, like this one , can play a role in supporting gallbladder health. Lifestyle choices, including dietary modifications, are often part of the treatment plan for gallbladder issues, highlighting the connection between nutrition and digestive health.
Genetic predisposition and certain medical conditions can also play a role in gallstone formation. Furthermore, pregnancy and prolonged fasting can also increase the risk. For example, individuals with a family history of gallstones or those who have undergone significant weight loss procedures may be at higher risk.
Cholecystitis
Cholecystitis is an inflammation of the gallbladder, often associated with the presence of gallstones. The inflammation can vary in severity, ranging from mild discomfort to severe pain and potentially life-threatening complications.The primary cause of cholecystitis is gallstones that obstruct the cystic duct, the tube connecting the gallbladder to the common bile duct. This blockage can lead to inflammation and infection within the gallbladder.
Other causes of cholecystitis, although less common, can include infections, tumors, or trauma to the gallbladder.
Symptoms and Diagnosis
The symptoms of gallstones and cholecystitis can overlap, making diagnosis challenging. However, some key differences exist.Gallstones may cause episodic pain, often located in the upper right abdomen or radiating to the back or right shoulder. This pain is typically severe and can be accompanied by nausea and vomiting. Cholecystitis pain is typically more persistent and intense, often accompanied by fever and chills.Diagnostic methods for both conditions include physical examinations, blood tests to assess inflammation markers, and imaging techniques.
Ultrasound is a common initial diagnostic tool. It provides images of the gallbladder and surrounding structures, allowing for the detection of gallstones and assessing the degree of inflammation. CT scans and MRCP (Magnetic Resonance Cholangiopancreatography) may be used in certain cases to obtain a more detailed view of the biliary system, especially when ultrasound results are inconclusive.
Gallstone Types
| Gallstone Type | Composition | Associated Risks |
|---|---|---|
| Cholesterol Stones | Predominantly cholesterol | Obesity, rapid weight loss, high-fat diet |
| Pigment Stones | Predominantly bilirubin | Liver conditions, hemolytic anemia |
| Mixed Stones | Combination of cholesterol and bilirubin | Combination of risk factors for cholesterol and pigment stones |
Diagnostic Tests
Several diagnostic tests are used to identify gallbladder disorders. Blood tests can help evaluate inflammation levels. Imaging techniques, such as ultrasound, CT scans, and MRCP, provide detailed visual representations of the gallbladder and biliary system, allowing for the identification of gallstones, blockages, and inflammation. A physician will determine the most appropriate tests based on the patient’s symptoms and medical history.
Gallbladder Treatment Options
Treating gallbladder disorders depends on the severity of the condition and the patient’s overall health. Effective management aims to alleviate symptoms, prevent complications, and improve quality of life. The available options range from lifestyle modifications to surgical interventions, each with its own set of benefits and risks.
Surgical Treatment Options
Surgical intervention, particularly laparoscopic cholecystectomy, is often the preferred approach for symptomatic gallbladder disease. This minimally invasive procedure offers several advantages over traditional open surgery, including reduced pain, shorter hospital stays, and faster recovery times.
Laparoscopic Cholecystectomy
Laparoscopic cholecystectomy involves making small incisions in the abdomen to insert specialized instruments and a tiny camera (laparoscope). The surgeon uses these tools to visualize the gallbladder and carefully remove it. This procedure is performed under general anesthesia.
“The use of specialized instruments and a laparoscope allows for precise removal of the gallbladder with minimal trauma to surrounding tissues.”
The procedure generally takes about 45-60 minutes.
Recovery Process Following Gallbladder Surgery
The recovery period after laparoscopic cholecystectomy is typically brief. Patients usually experience mild to moderate pain, which can be managed with prescribed medications. A gradual return to normal activities is encouraged, with physical limitations initially. Full recovery usually takes several weeks.
Risks and Complications
While laparoscopic cholecystectomy is generally safe, potential risks and complications include bleeding, infection, injury to nearby organs (such as the bile duct or liver), and the formation of scar tissue. Post-operative pain, bile duct injury, and wound infections are possible, although less common. The risk of complications is generally low, especially in experienced hands.
Understanding gallbladder anatomy, function, and treatment options is crucial for overall health. For example, gallstones can cause significant discomfort, and sometimes surgery is necessary. Interestingly, the diagnostic process for similar skin conditions, like plaque psoriasis, often involves a combination of physical examination and skin biopsy, as detailed in this helpful resource on how plaque psoriasis is diagnosed.
Ultimately, the right approach to gallbladder issues depends on the individual case and the severity of the problem.
Non-Surgical Treatment Options
Non-surgical approaches are considered for individuals with less severe gallbladder conditions or those who are not suitable candidates for surgery. These methods primarily focus on managing symptoms and improving overall health.
Dietary Modifications
Dietary changes can play a crucial role in managing gallbladder symptoms. A low-fat diet is often recommended to reduce the strain on the gallbladder. Eating smaller, more frequent meals and avoiding fatty foods, especially fried or greasy meals, can significantly help alleviate discomfort. It’s essential to consult a healthcare professional for personalized dietary recommendations.
Medical Management
Medication, such as pain relievers and medications to aid digestion, may be prescribed to manage symptoms. These medications help reduce inflammation and improve digestion, but they do not address the underlying cause of the gallbladder disorder.
Comparison of Surgical and Non-Surgical Treatment Options
| Feature | Surgical (Laparoscopic Cholecystectomy) | Non-Surgical |
|---|---|---|
| Procedure Type | Invasive, involves surgical removal of the gallbladder | Non-invasive, focuses on symptom management |
| Recovery Time | Several weeks | Can vary depending on the severity of symptoms |
| Effectiveness | Permanent resolution of the condition | Temporary relief of symptoms |
| Suitable for | Individuals with symptomatic gallbladder disease | Individuals with less severe conditions or those unsuitable for surgery |
| Risks | Bleeding, infection, injury to surrounding organs | Minimal, but can include side effects from medications |
Prevention and Management
Protecting your gallbladder involves a proactive approach, focusing on lifestyle choices and preventative measures. Understanding the factors that influence gallbladder health allows for informed decisions to reduce the risk of developing issues and manage any existing conditions effectively. A balanced approach combining dietary adjustments, regular checkups, and long-term management strategies can significantly impact overall well-being.
Lifestyle Factors Affecting Gallbladder Health
Maintaining a healthy weight and engaging in regular physical activity are crucial for gallbladder health. Obesity is a significant risk factor for gallstones, and regular exercise can help manage weight and reduce the likelihood of developing this condition. A sedentary lifestyle, conversely, increases the risk. Smoking also plays a role; research indicates a potential correlation between smoking and gallstone formation.
Genetic predisposition is another factor; a family history of gallstones can increase individual risk.
Dietary Recommendations for Gallstone Prevention
Dietary modifications play a key role in reducing the risk of gallstones. A diet low in saturated and trans fats, along with a balanced intake of fiber-rich foods, can be beneficial. Reducing refined carbohydrates and sugary foods can also contribute to overall health and lower the likelihood of developing gallstones. Individuals should prioritize whole, unprocessed foods. Small, frequent meals can also aid in preventing gallstone formation.
Importance of Regular Checkups and Screenings
Regular checkups are vital for early detection of potential gallbladder issues. A healthcare professional can identify risk factors and recommend appropriate screenings based on individual circumstances. These screenings can include blood tests, imaging scans, or other diagnostic procedures to monitor gallbladder health. Early detection allows for timely intervention and treatment if necessary, potentially preventing complications.
Long-Term Management Strategies for Gallbladder Disease
Long-term management of gallbladder disease focuses on mitigating symptoms and preventing recurrence. This may involve adhering to specific dietary guidelines, maintaining a healthy weight, and managing underlying conditions. Regular follow-up appointments with a healthcare professional are essential to monitor progress and adjust treatment plans as needed. For individuals who have undergone gallbladder removal, lifestyle modifications are crucial to prevent complications from developing.
Preventive Measures for Good Gallbladder Health
Maintaining good gallbladder health involves a combination of proactive measures.
- Maintain a healthy weight: Obesity is a significant risk factor for gallstones. Regular exercise and a balanced diet are crucial for weight management.
- Adopt a balanced diet: A diet low in saturated and trans fats, with adequate fiber intake, can reduce the risk of gallstones. Reducing refined carbohydrates and sugary foods is also recommended.
- Engage in regular physical activity: Regular exercise can help manage weight and improve overall health, lowering the risk of gallbladder issues.
- Maintain a healthy blood lipid profile: High cholesterol and other blood lipid abnormalities can contribute to gallstone formation. Consult with a healthcare professional for advice.
- Avoid rapid weight loss: Significant weight loss too quickly can increase the risk of gallstone formation.
- Regular medical checkups: Routine checkups are essential for early detection of potential gallbladder issues and risk factor assessment.
Final Thoughts: The Gallbladder Anatomy Function And Treatment
In conclusion, the gallbladder’s complex anatomy and function are essential for optimal digestion. This detailed look at its structure, role in the digestive process, and potential disorders provides a comprehensive understanding. The various treatment options, ranging from lifestyle changes to surgical interventions, offer hope for those affected by gallbladder issues. Remember that early diagnosis and proper management are crucial for maintaining digestive health.