Type 2 diabetes diet is crucial for managing this condition effectively. This guide provides a comprehensive overview of the dietary principles and strategies necessary for a healthy lifestyle. It explores the fundamental aspects of a balanced diet, emphasizing portion control and the importance of specific food choices. We’ll delve into macronutrient balance, food recommendations, practical implementation strategies, and monitoring techniques.
The content also addresses specific dietary needs for various populations, offering a holistic approach to managing type 2 diabetes through nutrition.
We’ll look at the differences between a healthy diet and a typical processed food diet, exploring the importance of macronutrients like carbohydrates, proteins, and fats. Different dietary approaches, like low-carb and Mediterranean diets, will be compared, and sample meal plans will illustrate practical applications. This guide aims to empower individuals with type 2 diabetes to make informed food choices and develop sustainable dietary habits for improved health and well-being.
Introduction to Type 2 Diabetes Diet
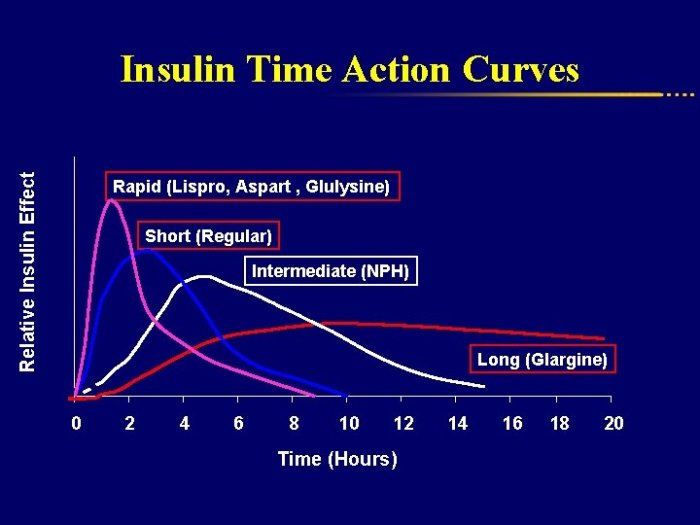
Type 2 diabetes is a chronic metabolic disorder characterized by high blood sugar levels. It occurs when the body either doesn’t produce enough insulin or the body’s cells don’t respond effectively to insulin. Diet plays a crucial role in managing type 2 diabetes. A well-structured dietary approach can help regulate blood sugar levels, improve insulin sensitivity, and promote overall health.
This is achieved through careful selection of foods, portion control, and consistent meal timing.A healthy diet for type 2 diabetes management focuses on whole, unprocessed foods, and limits refined carbohydrates, sugary drinks, and unhealthy fats. This approach emphasizes nutrient-rich foods that support insulin function and provide sustained energy without dramatic blood sugar spikes. It’s important to understand that this isn’t a restrictive diet, but rather a sustainable lifestyle change aimed at long-term well-being.
Fundamental Principles of a Healthy Diet
A healthy diet for managing type 2 diabetes emphasizes balanced intake of macronutrients (carbohydrates, proteins, and fats). It also prioritizes whole, unprocessed foods over highly processed items. Furthermore, it focuses on mindful eating habits, including portion control and regular meal timings. A balanced approach to food choices and mindful consumption are key components of effective management.
Key Goals of a Type 2 Diabetes Diet Plan
The primary goals of a type 2 diabetes diet plan are to:
- Maintain stable blood sugar levels throughout the day, avoiding significant fluctuations.
- Improve insulin sensitivity, allowing the body to utilize insulin more effectively.
- Promote weight management, as weight loss, even modest, can significantly improve blood sugar control.
- Reduce the risk of developing cardiovascular complications associated with diabetes.
Role of Portion Control
Portion control is a vital aspect of managing type 2 diabetes. Overeating, regardless of the type of food, can lead to blood sugar spikes and hinder the body’s ability to regulate it effectively. Understanding appropriate portion sizes and eating slowly helps to manage appetite and prevent overconsumption. By paying attention to hunger and fullness cues, individuals can achieve a healthy balance and avoid excess calorie intake.
This practice contributes to sustained weight management and improved blood sugar control.
Focusing on a type 2 diabetes diet is crucial for managing blood sugar levels, but sometimes other health concerns pop up. For example, a common ailment like a sore throat can sometimes affect your overall well-being and potentially impact your ability to adhere to a strict diabetes diet. Understanding the overview of sore throat can help you manage it effectively, which in turn supports your type 2 diabetes management plan.
Ultimately, a holistic approach to health, including a balanced diet, is key to maintaining good health with type 2 diabetes.
Comparison of Healthy vs. Processed Food Diets
| Characteristic | Healthy Diet | Typical Diet High in Processed Foods |
|---|---|---|
| Food Sources | Fruits, vegetables, whole grains, lean proteins, healthy fats | Processed meats, sugary drinks, refined grains, fast food, packaged snacks |
| Carbohydrate Type | Complex carbohydrates (e.g., brown rice, quinoa) | Simple carbohydrates (e.g., white bread, sugary cereals) |
| Fiber Content | High | Low |
| Nutrient Density | High | Low |
| Blood Sugar Impact | Slow, steady rise in blood sugar | Rapid, significant rise in blood sugar |
| Health Benefits | Improved blood sugar control, weight management, reduced risk of complications | Increased risk of blood sugar issues, weight gain, potential complications |
Macronutrient Balance in Type 2 Diabetes
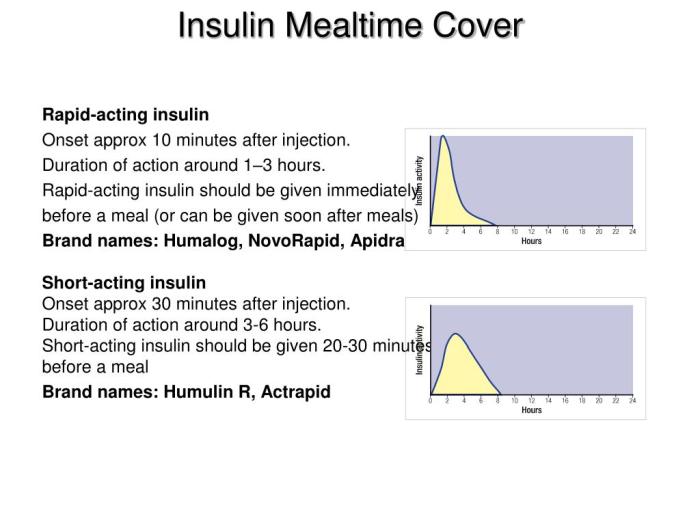
A balanced approach to macronutrients is crucial for managing type 2 diabetes effectively. This involves understanding the roles of carbohydrates, proteins, and fats, and how their consumption impacts blood sugar levels. Proper portioning and selection of foods within each category are key to achieving and maintaining optimal health.A key aspect of managing type 2 diabetes is understanding the impact of different foods on blood sugar.
Different macronutrients have varying effects on glucose levels. For example, carbohydrates are broken down into glucose, which directly influences blood sugar; proteins have a more gradual impact; and fats generally have a smaller effect on blood sugar compared to carbohydrates. By understanding these differences, individuals can make informed choices that support their overall health goals.
Carbohydrates
Carbohydrates are a primary source of energy for the body. However, individuals with type 2 diabetes need to be mindful of their carbohydrate intake, as high carbohydrate consumption can lead to blood sugar spikes. Choosing complex carbohydrates over simple carbohydrates is essential. Complex carbohydrates are digested more slowly, releasing glucose into the bloodstream gradually. This helps prevent significant fluctuations in blood sugar levels.
- Healthy sources include whole grains (brown rice, quinoa, oats), fruits (berries, apples, pears), and vegetables (broccoli, spinach, carrots).
Proteins
Proteins play a vital role in maintaining blood sugar levels by providing a sustained release of energy. They are essential for building and repairing tissues, and they also help to regulate appetite.
- Healthy sources include lean meats (chicken breast, fish), beans, lentils, tofu, and eggs.
Fats, Type 2 diabetes diet
Fats are essential for various bodily functions, including hormone production and nutrient absorption. Unsaturated fats, particularly monounsaturated and polyunsaturated fats, are beneficial for heart health. Trans fats and saturated fats should be limited.
- Healthy sources include avocados, nuts (almonds, walnuts), seeds (chia, flax), and olive oil.
Recommended Daily Intake Ratios
The recommended daily intake ratios for carbohydrates, proteins, and fats for managing type 2 diabetes vary depending on individual needs and health conditions. A balanced approach, often guided by a registered dietitian, is generally recommended. This generally involves consuming a moderate amount of carbohydrates, a moderate amount of protein, and a moderate amount of healthy fats.
The ideal ratio is not a fixed number but is customized for each individual.
Dietary Approaches for Type 2 Diabetes Management
Various dietary approaches can help manage type 2 diabetes. Some common approaches include the low-carb diet, the Mediterranean diet, and the DASH diet. Each approach emphasizes different macronutrient ratios and food groups.
Sample Meal Macronutrient Breakdown
| Meal | Carbohydrates (grams) | Protein (grams) | Fat (grams) |
|---|---|---|---|
| Oatmeal with berries and nuts | 30 | 15 | 10 |
| Grilled chicken salad with mixed greens and avocado | 25 | 30 | 15 |
| Lentil soup with whole-wheat bread | 40 | 20 | 10 |
Food Choices and Recommendations: Type 2 Diabetes Diet
Following a balanced diet is crucial for managing type 2 diabetes. It’s not just about restricting certain foods, but about making smart choices that support blood sugar control and overall health. This involves focusing on whole, unprocessed foods, understanding the role of fiber, and making informed decisions when eating out.Proper food choices play a pivotal role in effectively managing type 2 diabetes.
This includes a careful selection of foods that promote stable blood sugar levels and support overall well-being. By understanding the impact of different food groups and making mindful dietary decisions, individuals with type 2 diabetes can significantly improve their health outcomes.
Beneficial Food Groups
A diet rich in whole, unprocessed foods is essential for type 2 diabetes management. This includes a variety of fruits, vegetables, lean proteins, and whole grains. These foods provide essential nutrients without excessive added sugars or unhealthy fats.
- Fruits and Vegetables: Fruits and vegetables are packed with vitamins, minerals, and fiber, promoting satiety and aiding in blood sugar regulation. Choose a wide variety of colors, ensuring you get a diverse range of nutrients. Aim for at least five servings daily. Examples include berries, leafy greens, broccoli, and carrots.
- Lean Proteins: Lean protein sources, such as fish, poultry without skin, beans, and lentils, provide essential amino acids for tissue repair and growth, while also helping to maintain stable blood sugar levels. Limit red meat consumption due to its higher saturated fat content.
- Whole Grains: Whole grains, including brown rice, quinoa, oats, and whole-wheat bread, offer complex carbohydrates that release glucose more slowly into the bloodstream. This helps prevent sharp spikes in blood sugar.
Fiber’s Role in Blood Sugar Management
Fiber plays a significant role in managing blood sugar levels. It slows down the absorption of glucose, preventing rapid increases in blood sugar after meals. Soluble fiber, found in foods like oats and beans, can also help lower cholesterol levels.
Fiber helps regulate blood sugar by slowing the absorption of glucose into the bloodstream.
Increasing fiber intake is a key strategy for managing blood sugar levels. Include foods like beans, lentils, and whole grains in your diet.
Healthy Snack and Meal Ideas
Healthy snacks and meals are crucial for maintaining stable blood sugar levels throughout the day. These options should focus on complex carbohydrates, lean proteins, and healthy fats.
- Snacks: A handful of almonds or walnuts, a small portion of Greek yogurt with berries, or a slice of whole-wheat toast with avocado are all good examples of healthy snacks. Avoid processed snacks and sugary treats.
- Meal Ideas: Grilled chicken breast with brown rice and steamed vegetables, a lentil soup with whole-wheat bread, or a salad with grilled fish and a light vinaigrette dressing are all healthy meal options. These examples highlight the importance of balancing protein, carbohydrates, and healthy fats in each meal.
Limiting Sugary Drinks and Processed Foods
Sugary drinks and processed foods are often high in added sugars, unhealthy fats, and refined carbohydrates, which can significantly impact blood sugar control. Reducing or eliminating these foods from your diet can greatly benefit your health.
Focusing on a type 2 diabetes diet is crucial for managing blood sugar levels, but it’s also important to consider overall health. For example, knee injuries like ACL and PCL tears can significantly impact your ability to maintain a healthy lifestyle, making it harder to follow a balanced diet. Learning how to manage these injuries, like those detailed in this article about ACL and PCL injuries of the knee , is vital for ensuring you can stick to your diabetes diet plan and overall well-being.
Ultimately, a healthy diet and proactive injury management are key components for a better quality of life when managing type 2 diabetes.
Limiting sugary drinks and processed foods is crucial for maintaining stable blood sugar levels.
Eating Out Strategies
Eating out can be challenging for those managing type 2 diabetes. To make healthy choices, carefully review menus, choose dishes with plenty of vegetables, and opt for lean proteins. Ask for dressings and sauces on the side to control portion sizes.
Healthy Meal Options
| Meal | Dish | Description |
|---|---|---|
| Breakfast | Oatmeal with berries and nuts | A filling and nutritious breakfast that provides fiber, antioxidants, and healthy fats. |
| Lunch | Grilled chicken salad with mixed greens and vinaigrette | A balanced lunch with lean protein, fiber, and healthy fats. |
| Dinner | Baked salmon with roasted vegetables and quinoa | A healthy and delicious dinner option rich in omega-3 fatty acids and fiber. |
Practical Strategies for Diet Implementation
Turning a type 2 diabetes diet plan into a sustainable lifestyle requires practical strategies that go beyond just knowing what to eat. This involves incorporating the dietary recommendations into your daily routine, managing potential challenges, and building a healthy relationship with food. It’s about making informed choices that fit your preferences and lifestyle, not about restrictive or deprivation-based approaches.
Meal Planning and Preparation
Effective meal planning is crucial for successfully managing type 2 diabetes. A well-structured plan allows you to anticipate your dietary needs, shop efficiently, and prepare meals in advance. This proactive approach helps avoid impulsive choices and ensures you have healthy options readily available. Planning your meals and snacks for the entire week can significantly reduce the likelihood of unhealthy choices driven by hunger or convenience.
Portion Control and Mindful Eating
Portion control is an essential aspect of managing type 2 diabetes. By understanding appropriate portion sizes for different foods, you can better regulate calorie intake and maintain a healthy weight. Mindful eating encourages paying attention to your body’s hunger and fullness cues. This involves eating slowly, savoring each bite, and being present during meals, reducing the likelihood of overeating.
This practice promotes a healthier relationship with food and allows you to recognize when you’re truly satisfied, preventing unnecessary calorie consumption.
Managing Cravings and Emotional Eating
Cravings and emotional eating are common challenges for individuals with type 2 diabetes. Identifying the triggers for these cravings and developing healthy coping mechanisms is key to managing them. Recognizing emotional cues and substituting emotional eating with healthy activities can be a powerful tool. This could involve engaging in a physical activity, spending time in nature, or pursuing a hobby.
Experimenting with different strategies and finding what works best for you is essential.
Reading Food Labels and Identifying Hidden Sugars
Understanding food labels is critical for making informed choices. Pay close attention to the serving size, total carbohydrates, added sugars, and the total fat content per serving. Hidden sugars are often found in processed foods, sauces, and condiments. Carefully checking the ingredients list and understanding the different forms of sugar (e.g., high-fructose corn syrup, sucrose) is important.
Familiarizing yourself with the nutritional information on food labels helps you make healthier selections.
Grocery Shopping and Meal Preparation
Efficient grocery shopping is a significant part of implementing a type 2 diabetes diet. Creating a shopping list based on your meal plan helps avoid impulse buys and ensures you purchase only the necessary ingredients. Prepare ingredients in advance, such as chopping vegetables or cooking grains. This makes it easier to quickly and healthily prepare meals throughout the week.
Weekly Meal Planning Checklist
| Day | Breakfast | Lunch | Dinner | Snacks |
|---|---|---|---|---|
| Monday | Oatmeal with berries and nuts | Salad with grilled chicken | Baked salmon with roasted vegetables | Fruit and yogurt |
| Tuesday | Whole-wheat toast with avocado | Leftover salmon and vegetables | Lentil soup with whole-wheat bread | Hard-boiled eggs |
| Wednesday | Scrambled eggs with spinach | Tuna salad sandwich on whole-wheat bread | Chicken stir-fry with brown rice | Apple slices with peanut butter |
| Thursday | Greek yogurt with granola | Leftover chicken stir-fry | Turkey meatballs with zucchini noodles | Carrot sticks with hummus |
| Friday | Smoothie with fruits and protein powder | Leftover turkey meatballs | Vegetarian chili with whole-wheat crackers | Mixed nuts |
| Saturday | Whole-wheat pancakes with fruit | Quinoa salad with grilled vegetables | Homemade pizza with whole-wheat crust | Fruit salad |
| Sunday | Breakfast burrito with eggs and beans | Leftover pizza | Roast chicken with roasted potatoes | Popcorn |
Monitoring and Adjusting the Diet
A Type 2 diabetes diet is not a one-size-fits-all approach. Individual responses to dietary changes vary, and consistent monitoring is crucial for success. This phase emphasizes the importance of tracking your blood sugar levels and adjusting your food choices accordingly. Regular check-ins with your healthcare provider are vital to ensure the diet remains effective and safe.Maintaining a healthy blood sugar level is essential for managing Type 2 diabetes effectively.
A type 2 diabetes diet is crucial for managing blood sugar levels, but sometimes medication like metformin isn’t enough. If you’re noticing potential signs that metformin isn’t working for you, checking out this helpful guide on signs metformin not working could offer some insights. Ultimately, a balanced diet, combined with the right medication and lifestyle choices, remains the cornerstone of effective type 2 diabetes management.
Fluctuations can impact your overall well-being and increase the risk of complications. Continuous monitoring, alongside appropriate dietary adjustments, is key to achieving and maintaining optimal blood glucose control.
Importance of Regular Blood Sugar Monitoring
Regular blood sugar monitoring provides valuable insights into how your body responds to different foods and lifestyle choices. It helps identify patterns, allowing you to make informed decisions about your diet. Understanding how your blood sugar reacts to meals, snacks, and daily activities enables you to make adjustments to achieve and maintain target levels. This crucial information aids in preventing potential spikes and dips, thereby minimizing the risk of complications.
Role of a Healthcare Professional
A healthcare professional, such as a doctor or registered dietitian, plays a pivotal role in guiding your dietary choices. They can assess your individual needs and medical history, providing personalized recommendations tailored to your specific situation. Their expertise ensures the diet aligns with your overall health goals and prevents any unintended consequences. They can also address any concerns or complications that arise during the process.
Methods for Adjusting the Diet
Dietary adjustments are crucial for maintaining optimal blood sugar control. These adjustments might include modifying portion sizes, increasing or decreasing certain food groups, or incorporating specific healthy alternatives. For instance, someone experiencing high blood sugar after consuming refined carbohydrates might reduce their intake of white bread or pasta, replacing them with whole-grain alternatives. Another example might involve adjusting portion sizes of fruits or vegetables to maintain the desired macronutrient balance.
This personalized approach is vital for managing the condition effectively.
Strategies for Addressing Potential Challenges or Setbacks
Adjusting to a new diet can present challenges. Feeling deprived or facing unexpected setbacks can hinder progress. Strategies to overcome these challenges include:
- Seeking support from a registered dietitian or support group. The encouragement and guidance from others facing similar challenges can significantly improve motivation and adherence to the diet.
- Developing a supportive environment. Encouraging family members or close friends to understand your dietary needs can be crucial for maintaining consistency.
- Creating a meal plan that incorporates your preferences and lifestyle. This ensures the diet remains sustainable and enjoyable in the long run.
- Celebrating small victories. Acknowledging and appreciating progress, no matter how small, fosters a positive attitude and encourages continued adherence to the diet.
Potential Complications Related to Poor Diet
Poor dietary choices can exacerbate Type 2 diabetes, leading to various complications. This includes:
- Increased risk of cardiovascular disease. A diet high in saturated and unhealthy fats can contribute to high cholesterol levels, increasing the risk of heart problems.
- Neuropathy. Poor blood sugar control can damage nerves, leading to pain, numbness, or tingling in the extremities.
- Kidney damage. Chronic high blood sugar can strain the kidneys, potentially leading to kidney failure.
- Eye problems. Fluctuations in blood sugar can damage the blood vessels in the eyes, potentially leading to vision loss.
Potential Symptoms of Blood Sugar Imbalance
Recognizing symptoms of blood sugar imbalance is essential for prompt intervention.
| Symptom | Description |
|---|---|
| Increased thirst | Frequent and intense thirst, often accompanied by dry mouth. |
| Frequent urination | Increased need to urinate, particularly at night. |
| Unexplained weight loss | Significant weight loss without conscious effort to lose weight. |
| Blurred vision | Difficulty seeing clearly, often a gradual onset. |
| Slow-healing sores | Delayed healing of cuts or wounds. |
| Fatigue | Persistent feelings of tiredness or exhaustion. |
Dietary Considerations for Specific Populations
A type 2 diabetes diet is not a one-size-fits-all approach. Individual needs vary significantly depending on factors like age, pregnancy status, other health conditions, and cultural background. This section delves into the specific dietary considerations for different population groups to ensure optimal health management and well-being.
Dietary Modifications for Pregnant Women with Type 2 Diabetes
Managing type 2 diabetes during pregnancy requires careful attention to blood glucose control and fetal well-being. Pregnant women with type 2 diabetes need to closely monitor their carbohydrate intake, aiming for consistent and controlled portions throughout the day. Frequent, smaller meals or snacks are often recommended to prevent large fluctuations in blood sugar levels. This is crucial for both maternal and fetal health.
A registered dietitian or healthcare professional specializing in maternal-fetal health can provide personalized dietary guidance. Crucially, they will advise on appropriate calorie intake to support both the mother’s and the baby’s growth needs.
Needs of Children and Adolescents with Type 2 Diabetes
Children and adolescents with type 2 diabetes require a balanced diet tailored to their growth and development needs. Focus should be on providing nutrient-dense foods while managing carbohydrate intake. Portion control and regular mealtimes are essential for maintaining stable blood sugar levels. Dietary education plays a significant role in empowering children and adolescents to make healthy food choices.
This includes teaching them about carbohydrate counting and understanding the impact of different foods on their blood sugar. Parents and caregivers also need support and guidance to effectively manage the child’s diet within the family context.
Considerations for Older Adults with Type 2 Diabetes
Older adults with type 2 diabetes may have different nutritional needs compared to younger individuals. Factors like reduced appetite, decreased physical activity, and potential digestive issues need consideration. Dietary strategies should prioritize nutrient density, with an emphasis on easily digestible foods. Careful attention should be given to maintaining adequate protein intake to support muscle mass and function.
It is also important to address any potential vitamin or mineral deficiencies. Working closely with a healthcare professional is crucial to tailor the diet to the individual’s specific needs and circumstances.
Culturally Appropriate Dietary Options
Dietary patterns are deeply rooted in cultural traditions. A type 2 diabetes diet should be mindful of these traditions to ensure cultural sensitivity and promote adherence. Individuals should be empowered to incorporate culturally relevant foods into their meal plans while maintaining appropriate blood sugar management. This involves understanding the specific foods and preparation methods common in their culture and modifying them to fit the diabetic dietary guidelines.
Dietary Needs of Individuals with Other Health Conditions
Individuals with type 2 diabetes often have co-existing health conditions, which further complicate dietary management. For example, those with hypertension may require a low-sodium diet. Those with kidney disease might need to limit protein intake. Careful consideration of these additional health factors is crucial in developing a safe and effective dietary plan. Consulting a healthcare professional is essential for developing a comprehensive dietary plan that addresses all the individual’s health needs.
Examples of Culturally Appropriate Dietary Options
| Region | Culturally Relevant Food | Dietary Modification for Type 2 Diabetes |
|---|---|---|
| Mediterranean | Olive oil, vegetables, fish | Limit red meat, use healthy fats like olive oil, increase portion of vegetables, and include fish more frequently. |
| South Asian | Lentils, whole grains, vegetables | Limit refined carbohydrates, increase portion of vegetables, choose whole grains over refined grains, and substitute some dairy products with plant-based alternatives. |
| East Asian | Rice, noodles, vegetables, tofu | Limit refined carbohydrates, increase portion of vegetables, choose whole grains over refined grains, and consider lean protein sources like fish or tofu. |
| African | Beans, vegetables, fruits, whole grains | Limit processed foods, increase portion of vegetables and fruits, choose whole grains over refined grains, and include lean protein sources like beans or fish. |
Illustrative Examples of Healthy Meals and Snacks
A well-structured diet plays a crucial role in managing type 2 diabetes. Choosing the right foods and understanding portion sizes can significantly improve blood sugar control and overall health. This section provides practical examples of healthy meals and snacks designed to support diabetes management.
Healthy Breakfast
Breakfast is an important meal to kickstart your day, providing essential nutrients for energy and blood sugar stability. This example emphasizes whole grains, lean protein, and healthy fats. 
Example: Oatmeal with Berries and Nuts
- Oatmeal (1/2 cup dry): Provides complex carbohydrates, which are digested slowly, helping to maintain stable blood sugar levels. A half cup dry will yield about 150 calories and 3 grams of fiber.
- Berries (1/2 cup): Packed with antioxidants and vitamins, berries are low in sugar and high in fiber. A half cup of berries contains approximately 40-50 calories.
- Nuts (1/4 cup): A source of healthy fats, protein, and fiber. Almonds, walnuts, or pecans are excellent choices. A quarter cup of nuts has about 160-180 calories and 4-6 grams of protein.
Nutritional Content (approximate): Approximately 350 calories, 15-20 grams of carbohydrates, 5-7 grams of fiber, 8-10 grams of protein, and 15-20 grams of healthy fats.
Healthy Lunch
Lunch should provide sustained energy and a balanced mix of nutrients to prevent blood sugar spikes. This example focuses on lean protein, complex carbohydrates, and non-starchy vegetables. 
Example: Grilled Chicken Salad with Brown Rice
- Grilled Chicken Breast (4 ounces): A lean protein source that helps to keep you full and satisfied. A 4-ounce serving of grilled chicken breast contains approximately 140 calories and 30 grams of protein.
- Mixed Greens Salad (1.5 cups): Provides non-starchy vegetables and fiber. A 1.5-cup serving of mixed greens has around 20-30 calories.
- Brown Rice (1/2 cup cooked): A complex carbohydrate that digests slowly, providing sustained energy. A half cup of cooked brown rice has around 120 calories and 4-5 grams of fiber.
Nutritional Content (approximate): Approximately 300 calories, 30-40 grams of carbohydrates, 6-8 grams of fiber, 30-35 grams of protein, and 8-10 grams of healthy fats.
Healthy Dinner
Dinner should be a balanced meal, focusing on lean protein, non-starchy vegetables, and a controlled portion of complex carbohydrates. 
Example: Baked Salmon with Broccoli and Quinoa
- Baked Salmon (4 ounces): A rich source of omega-3 fatty acids and protein. A 4-ounce portion of baked salmon has approximately 180 calories and 25 grams of protein.
- Steamed Broccoli (1 cup): A low-calorie, high-fiber vegetable that supports overall health. A cup of steamed broccoli has around 30 calories and 3-4 grams of fiber.
- Quinoa (1/2 cup cooked): A complete protein and complex carbohydrate. A half cup of cooked quinoa has approximately 110 calories and 4 grams of protein.
Nutritional Content (approximate): Approximately 320 calories, 25-30 grams of carbohydrates, 7-9 grams of fiber, 30-35 grams of protein, and 5-7 grams of healthy fats.
Healthy Snacks
Snacks can help prevent blood sugar crashes and provide sustained energy between meals. 
Example Snacks:
- Handful of Almonds (1/4 cup): Provides healthy fats, protein, and fiber.
- Small Apple (1 medium): A source of fiber and natural sugars.
- Small Portion of Greek Yogurt (1/2 cup): A good source of protein and calcium.
Conclusion
In conclusion, managing type 2 diabetes through diet requires a multifaceted approach. By understanding the principles of a healthy diet, incorporating practical strategies, and monitoring your progress, you can effectively control your blood sugar levels and improve your overall health. Remember, consistency and personalization are key. This guide provides a solid foundation, but consulting with a healthcare professional is essential for tailored advice and support.