Prozac fluoxetine vs lexapro escitalopram: A comparison of these two popular antidepressants, both Selective Serotonin Reuptake Inhibitors (SSRIs), is crucial for individuals seeking effective treatment. This in-depth look examines their mechanisms of action, common side effects, dosage ranges, and potential interactions. Understanding the nuances between these drugs empowers informed decision-making with a healthcare professional.
This exploration delves into the scientific underpinnings of these medications, comparing their efficacy in treating various symptoms of depression and anxiety. We will analyze their individual mechanisms of action, dosage guidelines, and potential interactions with other medications. Ultimately, the goal is to provide a comprehensive overview that aids in the discussion between patients and their healthcare providers.
Introduction to Selective Serotonin Reuptake Inhibitors (SSRIs)
Selective Serotonin Reuptake Inhibitors, or SSRIs, are a class of antidepressant medications commonly prescribed to treat major depressive disorder and various anxiety disorders. They work by influencing the brain’s neurochemistry, specifically targeting serotonin, a neurotransmitter associated with mood regulation. Understanding how SSRIs function and their potential side effects is crucial for anyone considering this type of treatment.SSRIs work by blocking the reabsorption (reuptake) of serotonin in the brain’s synapses.
This means more serotonin remains available in the synaptic cleft, the space between nerve cells, to bind to receptors and potentially improve mood and reduce anxiety. This increased serotonin activity is believed to contribute to the therapeutic effects of these medications. However, it’s important to remember that the exact mechanisms by which SSRIs produce their effects are still being investigated and fully understood.
Common Side Effects of SSRIs
Several side effects are commonly associated with SSRI use. These can vary in intensity and duration among individuals, and often subside as the body adjusts to the medication. Some common side effects include nausea, headache, insomnia, anxiety, sexual dysfunction, and changes in appetite. It’s important to note that not everyone experiences all these side effects, and the severity can vary significantly.
Individual Patient Responses to SSRIs
Individual responses to SSRIs can differ greatly. Factors like age, pre-existing medical conditions, and genetic predispositions can influence how a person reacts to the medication. Some individuals may experience a rapid and significant improvement in their symptoms, while others may require adjustments to dosage or even a switch to a different medication to achieve optimal results. This variability highlights the importance of close monitoring by a healthcare professional throughout the treatment process.
Comparison of Common SSRIs
| Drug Name | Chemical Structure | Primary Action | Typical Dosage Range | Common Side Effects |
|---|---|---|---|---|
| Fluoxetine (Prozac) | A complex molecule with a specific arrangement of atoms. The exact chemical structure is beyond the scope of this discussion. | Blocks serotonin reuptake. | Generally 20-80 mg daily, in a single dose or divided doses. | Nausea, insomnia, headache, sexual dysfunction, weight changes, and anxiety. |
| Sertraline (Zoloft) | A complex molecule with a specific arrangement of atoms. The exact chemical structure is beyond the scope of this discussion. | Blocks serotonin reuptake. | Generally 50-200 mg daily, in a single dose or divided doses. | Nausea, diarrhea, insomnia, headache, sexual dysfunction, and dizziness. |
| Paroxetine (Paxil) | A complex molecule with a specific arrangement of atoms. The exact chemical structure is beyond the scope of this discussion. | Blocks serotonin reuptake. | Generally 10-50 mg daily, in a single dose or divided doses. | Nausea, insomnia, headache, sexual dysfunction, weight changes, and sedation. |
| Citalopram (Celexa) | A complex molecule with a specific arrangement of atoms. The exact chemical structure is beyond the scope of this discussion. | Blocks serotonin reuptake. | Generally 10-40 mg daily, in a single dose or divided doses. | Nausea, headache, insomnia, sexual dysfunction, and anxiety. |
| Escitalopram (Lexapro) | A complex molecule with a specific arrangement of atoms. The exact chemical structure is beyond the scope of this discussion. | Blocks serotonin reuptake. | Generally 5-20 mg daily, in a single dose or divided doses. | Nausea, headache, insomnia, sexual dysfunction, and anxiety. |
This table provides a general overview of common SSRIs. Dosage and specific side effects can vary depending on individual patient needs and responses. It’s important to remember that this information is not a substitute for professional medical advice.
I’ve been researching Prozac (fluoxetine) versus Lexapro (escitalopram) lately, and it’s fascinating how similar yet different these antidepressants can be. While researching the side effects, I stumbled upon information about a possible connection between certain medications and skin conditions, like a herpes rash on the body. This article highlighted the importance of understanding potential interactions, which got me thinking more deeply about the subtle differences between these two popular antidepressants.
Ultimately, I’m still trying to figure out which might be the best fit for me, and I’m hoping this deeper dive will help me make the right choice.
Fluoxetine (Prozac)
Fluoxetine, marketed as Prozac, is a widely prescribed selective serotonin reuptake inhibitor (SSRI) antidepressant. It’s often a first-line treatment for major depressive disorder, obsessive-compulsive disorder (OCD), and bulimia nervosa. Understanding its mechanism of action, potential side effects, dosage, and interactions is crucial for effective patient management.Fluoxetine works by increasing the levels of serotonin in the brain. Serotonin is a neurotransmitter involved in mood regulation, and low levels are associated with depression and anxiety.
Fluoxetine achieves this by inhibiting the serotonin transporter (SERT), a protein that removes serotonin from the synapse. By preventing this reuptake, more serotonin remains available to bind to its receptors, leading to a potential improvement in mood.
Mechanism of Action
Fluoxetine’s primary mechanism involves blocking the serotonin transporter (SERT). This prevents the reabsorption of serotonin into the nerve cells, allowing it to remain in the synaptic cleft for a longer period. This increased serotonin availability is thought to contribute to the therapeutic effects of the medication.
Common Side Effects
A variety of side effects can occur while taking Fluoxetine. Some are relatively common and transient, while others are more severe and require medical attention. Common side effects include nausea, insomnia, anxiety, sexual dysfunction, and headaches. It’s essential to report any concerning side effects to a healthcare provider.
Dosage and Variations
Fluoxetine dosage is highly individualized and depends on the specific condition being treated and the patient’s response. Typical starting doses range from 10 mg to 20 mg per day, gradually increasing as needed and tolerated. For severe depression or OCD, doses might reach 80 mg daily. Adjustments are made based on clinical assessment and patient monitoring. Long-term maintenance doses can vary, often remaining in the same range as the therapeutic dose.
Potential Drug Interactions
Fluoxetine can interact with numerous medications, potentially altering their effectiveness or increasing the risk of adverse effects. Some examples include medications for blood clotting, certain pain relievers, and other antidepressants. It’s critical for patients to disclose all medications, including over-the-counter drugs and supplements, to their healthcare providers. This proactive disclosure helps prevent potentially harmful interactions.
Comparison to Other SSRIs
| Characteristic | Fluoxetine (Prozac) | Other SSRIs (e.g., Sertraline, Paroxetine) |
|---|---|---|
| Metabolism | Primarily metabolized by the liver via CYP2D6 and CYP3A4 pathways. | Metabolism varies; some are primarily metabolized by CYP2D6, while others have different pathways. |
| Half-Life | Approximately 1-4 days, with a longer active metabolite (norfluoxetine) with a half-life of 4-6 days. | Half-lives vary, but some are similar, and others are shorter. |
| Potential Drug Interactions | High potential for drug interactions, particularly with CYP2D6 inhibitors. | Potential for drug interactions, but the specific interactions can vary. |
The table highlights the differences in metabolism, half-life, and potential drug interactions between Fluoxetine and other SSRIs. Understanding these differences is crucial for clinicians when choosing appropriate treatment strategies.
Escitalopram (Lexapro)
Escitalopram, sold under the brand name Lexapro, is another commonly prescribed Selective Serotonin Reuptake Inhibitor (SSRI) antidepressant. It works by increasing the levels of serotonin in the brain, which is believed to play a crucial role in regulating mood and other mental processes. Understanding how it works, its potential side effects, and typical dosages is important for anyone considering or taking this medication.
Mechanism of Action
Escitalopram, a chiral compound, is a selective serotonin reuptake inhibitor (SSRI). It specifically blocks the reabsorption of serotonin in the brain’s synapses. This allows more serotonin to remain in the synaptic cleft, increasing its availability to bind with serotonin receptors and potentially alleviate depressive symptoms. By enhancing serotonin activity, it’s thought to improve mood and other related cognitive functions.
While comparing Prozac (fluoxetine) and Lexapro (escitalopram), it’s important to remember that individual responses to these antidepressants can vary. One potential factor influencing how a person reacts to these medications is a possible citric acid allergy. Understanding the symptoms of a citric acid allergy and how to manage them is crucial, as this can affect the effectiveness of treatments like Prozac and Lexapro.
For more information on citric acid allergy symptoms and coping strategies, check out this helpful guide: citric acid allergy symptoms and how to cope. Ultimately, consulting a doctor for a personalized treatment plan remains the best approach for choosing between Prozac and Lexapro, or other similar medications.
Common Side Effects
Several side effects can be associated with escitalopram use. These are often temporary and can lessen with continued use or adjustments in dosage. Some of the more commonly reported side effects include nausea, headache, insomnia, dizziness, and sexual dysfunction. Other possible side effects include anxiety, agitation, tremor, sweating, and diarrhea.
Dosage Ranges
The typical starting dosage for escitalopram is generally between 5 to 10 mg daily, taken orally. The dosage can be adjusted upward in increments of 5 to 10 mg as needed and tolerated by the patient, under the guidance of a healthcare professional. The maximum recommended dosage is typically 20 mg daily, but higher doses may be considered in specific cases, again, always under close medical supervision.
Individual responses to escitalopram can vary significantly, and the optimal dosage must be tailored to the individual patient’s needs and response.
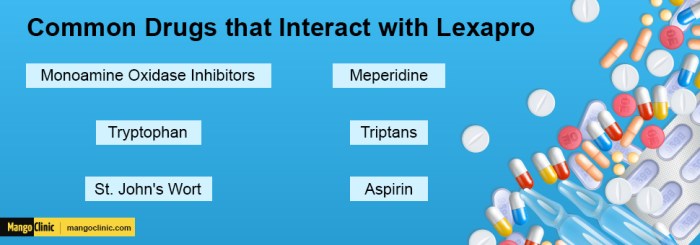
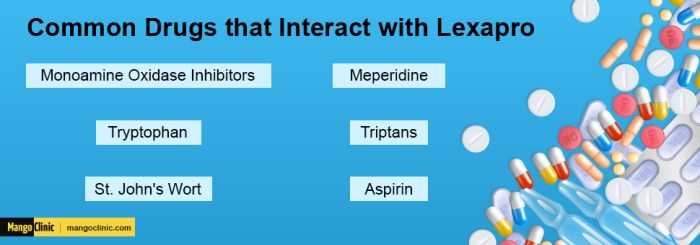
Potential Drug Interactions
Escitalopram can interact with various other medications, potentially altering their effectiveness or increasing the risk of adverse effects. These interactions can involve drugs used to treat other conditions like pain, anxiety, or high blood pressure. Interactions can occur when escitalopram is taken with other SSRIs, monoamine oxidase inhibitors (MAOIs), or certain medications used to treat heart conditions. It’s crucial to inform your healthcare provider about all medications you are taking, including over-the-counter drugs and supplements, to prevent potential drug interactions.
Comparison with Other SSRIs
| Characteristic | Escitalopram (Lexapro) | Fluoxetine (Prozac) | Sertraline (Zoloft) | Paroxetine (Paxil) |
|---|---|---|---|---|
| Efficacy | Generally comparable to other SSRIs in treating depressive disorders. Clinical studies have demonstrated its effectiveness in treating major depressive disorder. | Demonstrated effectiveness in treating depression, anxiety, and other conditions. | Demonstrated efficacy in treating depression, anxiety, and panic disorders. | Effective in treating depression, anxiety, and obsessive-compulsive disorder. |
| Common Side Effects | Nausea, headache, insomnia, sexual dysfunction, anxiety, dizziness, agitation, tremor, sweating, diarrhea. | Nausea, insomnia, sexual dysfunction, headache, anxiety, weight change, tremor. | Nausea, diarrhea, insomnia, sexual dysfunction, headache, anxiety, sweating. | Nausea, insomnia, sexual dysfunction, weight gain, headache, anxiety, drowsiness. |
This table provides a general comparison, and individual experiences may vary. It’s essential to consult with a healthcare professional for personalized advice regarding medication selection and management.
Direct Comparison: Fluoxetine vs. Escitalopram
Both fluoxetine (Prozac) and escitalopram (Lexapro) are selective serotonin reuptake inhibitors (SSRIs) commonly prescribed for depression and anxiety. While both aim to regulate serotonin levels in the brain, subtle differences in their mechanisms of action and potential side effects can influence treatment outcomes. This comparison will delve into their efficacy, side effect profiles, potential drug interactions, and key pharmacokinetic characteristics.
Efficacy in Treating Specific Symptoms
Clinical studies have shown comparable efficacy for both fluoxetine and escitalopram in treating core symptoms of depression, such as low mood, loss of interest, and changes in appetite and sleep. However, some studies suggest potential differences in managing specific symptoms. For example, some patients may find fluoxetine more effective in managing anxiety associated with obsessive-compulsive disorder (OCD), while escitalopram might be better suited for social anxiety.
Individual responses vary significantly, and the best choice often depends on the individual patient’s unique needs and symptom presentation.
Comparing Prozac (fluoxetine) and Lexapro (escitalopram) is a common question for those looking at antidepressants. While these are both selective serotonin reuptake inhibitors (SSRIs), subtle differences exist in their mechanisms. Recently, the FDA’s rejection of MDMA for PTSD treatment, as detailed in this article , highlights the ongoing research and debate around effective treatments for mental health conditions.
Ultimately, the best choice between Prozac and Lexapro, or any other medication, should always be made in consultation with a healthcare professional.
Side Effect Profiles
While both medications generally have a similar side effect profile, subtle differences exist. Fluoxetine is sometimes associated with a higher incidence of insomnia and agitation, while escitalopram may be linked to a slightly higher risk of nausea and gastrointestinal discomfort. It’s important to note that individual experiences can differ widely, and careful monitoring of side effects is crucial for each patient.
Potential Drug Interactions
Both fluoxetine and escitalopram can interact with other medications. These interactions can range from mild to severe and may alter the effectiveness or safety of the prescribed medications. For example, concurrent use with certain antidepressants or medications affecting the liver enzymes can lead to increased blood levels of one or both drugs, potentially causing adverse effects. Consult with a healthcare professional about potential drug interactions before starting any new medication, especially if already taking other prescription drugs.
Pharmacokinetic Comparison, Prozac fluoxetine vs lexapro escitalopram
| Characteristic | Fluoxetine (Prozac) | Escitalopram (Lexapro) |
|---|---|---|
| Absorption | Rapid absorption after oral administration, with peak plasma levels occurring within a few hours. | Rapid absorption after oral administration, with peak plasma levels occurring within a few hours. |
| Distribution | Wide distribution throughout the body, with significant binding to plasma proteins. | Wide distribution throughout the body, with significant binding to plasma proteins. |
| Metabolism | Extensive metabolism primarily by the cytochrome P450 enzyme system, specifically CYP2D6. Note that this can lead to potential interactions with other medications metabolized by the same enzymes. | Primary metabolism by CYP2C19. This pathway is less commonly involved in significant drug interactions compared to CYP2D6. |
| Excretion | Excreted primarily in the urine, with a portion also excreted in the feces. | Excreted primarily in the urine, with a smaller portion in the feces. |
Effectiveness in Different Depression Subtypes
| Depression Subtype | Fluoxetine Reported Effectiveness | Escitalopram Reported Effectiveness |
|---|---|---|
| Major Depressive Disorder (MDD) | Generally effective in treating core symptoms of MDD. | Generally effective in treating core symptoms of MDD. |
| Generalized Anxiety Disorder (GAD) | Demonstrates effectiveness in reducing anxiety symptoms. | Demonstrates effectiveness in reducing anxiety symptoms. |
| Obsessive-Compulsive Disorder (OCD) | Potentially higher efficacy in treating OCD symptoms compared to escitalopram in some cases. | Demonstrates effectiveness in treating OCD symptoms. |
Patient Considerations and Factors
Choosing the right antidepressant, like Fluoxetine (Prozac) or Escitalopram (Lexapro), is a crucial decision that hinges on understanding the individual patient’s needs and history. Both medications are effective SSRIs, but their specific properties and potential side effects may vary, making personalized treatment plans essential. Factors like a patient’s medical history, concurrent conditions, and anticipated response to treatment influence the selection process.Individual patient needs play a pivotal role in determining the most appropriate SSRI.
A thorough understanding of the patient’s overall health, including their medical history, family history, and current lifestyle, is paramount for informed decision-making. These factors provide a foundation for predicting potential responses to medication and tailoring the treatment approach accordingly.
Patient History and Individual Needs
Patient history significantly impacts the selection process. A comprehensive review of past mental health diagnoses, previous treatment responses, and any allergies or sensitivities to medications is vital. This detailed history aids in identifying potential risks or interactions that might influence treatment outcomes. Furthermore, a patient’s personal circumstances, such as their lifestyle, social support network, and adherence to treatment plans, also factor into the decision.
These elements collectively contribute to a personalized treatment plan, maximizing the likelihood of success.
Factors Influencing Response to SSRIs
Several factors may influence a patient’s response to a specific SSRI. Genetic predisposition, age, and body weight can all play a role. For instance, some individuals may metabolize medications at a faster rate than others, impacting the effectiveness of the chosen SSRI. Additionally, coexisting medical conditions, such as thyroid disorders or other chronic illnesses, can affect how the body processes medications.
Finally, the severity of the patient’s depressive symptoms and any other contributing factors, like stress or anxiety, also influence treatment outcomes. Understanding these factors allows healthcare providers to tailor treatment approaches to individual needs.
Comorbid Conditions and Treatment Choices
Comorbid conditions significantly impact treatment decisions. For example, a patient with anxiety disorders might respond better to an SSRI with additional anxiolytic properties. Similarly, patients with other medical conditions, such as cardiovascular issues, need careful consideration of potential drug interactions. Careful evaluation of the interplay between the primary condition and any comorbid factors allows for a more nuanced approach to treatment selection.
Patient Education and Medication Adherence
Patient education is crucial for successful treatment. Providing clear information about the medication, its potential side effects, and the importance of adherence to the treatment plan is essential. Open communication and active listening help patients understand the rationale behind their treatment and foster a sense of partnership in their recovery. This also encompasses educating patients about the signs and symptoms of potential side effects, empowering them to recognize and report any issues promptly.
Key Considerations for Healthcare Professionals
| Factor | Explanation |
|---|---|
| Patient History | Thorough review of past diagnoses, treatment responses, allergies, and lifestyle factors. |
| Individual Needs | Personalized approach considering patient’s circumstances and preferences. |
| Comorbid Conditions | Evaluation of interactions between the primary condition and any comorbid factors. |
| Patient Education | Providing clear information about the medication, side effects, and adherence. |
| Potential Side Effects | Informing patients about possible side effects and encouraging prompt reporting. |
| Metabolic Rate | Understanding how the body processes medications to optimize dosage and effectiveness. |
Treatment Strategies and Protocols
Navigating the path to recovery with SSRIs like Fluoxetine (Prozac) and Escitalopram (Lexapro) requires a personalized approach. Treatment plans are not one-size-fits-all, but rather dynamic and adaptable to the individual’s unique needs and response to medication. Factors like symptom severity, co-occurring conditions, and personal preferences play a crucial role in tailoring effective strategies.Understanding how the treatment unfolds, including adjustments based on individual responses, is vital.
This involves monitoring for both positive effects and potential side effects. Careful management of side effects and diligent progress monitoring are key elements in optimizing treatment outcomes. A comprehensive approach considers both medication and supplementary therapies.
Individualized Treatment Plans
Treatment plans for SSRIs must be tailored to each patient’s unique response. A patient who shows rapid improvement with a specific dose might require adjustments as their condition stabilizes. Conversely, a patient who experiences a slow or inconsistent response may need a higher dosage, a different SSRI, or the addition of other therapeutic interventions. Careful monitoring is essential to identify the most effective strategy.
Managing Side Effects
Side effects associated with SSRIs, while often temporary, can significantly impact patient adherence. Strategies for managing side effects encompass various approaches, including gradual dose titration, adjusting the timing of medication administration, and exploring alternative medications or dosages within the SSRI class. Communication with the prescribing physician is critical for addressing any emerging or persistent side effects. For example, if nausea is a concern, the physician might recommend taking the medication with food or suggest an antiemetic.
Monitoring Patient Progress
Monitoring patient progress is crucial during SSRI treatment. This involves regular check-ins with the prescribing physician, assessing symptom severity using standardized scales (e.g., Hamilton Depression Rating Scale), and tracking the patient’s overall well-being. This data provides valuable insights into the efficacy of the treatment and allows for necessary adjustments. Tracking mood, sleep patterns, and appetite can offer additional indicators of progress.
Treatment Strategies Table
| Patient Response | Treatment Strategy |
|---|---|
| Rapid improvement | Maintain current dose and monitor for continued effectiveness; adjust dosage as needed for sustained improvement. |
| Slow/Inconsistent response | Increase dosage, switch to a different SSRI, or consider combining with other therapies (e.g., psychotherapy, lifestyle modifications). |
| Severe side effects | Adjust dosage, switch to a different SSRI, explore non-pharmacological strategies (e.g., lifestyle modifications, complementary therapies), or consider alternative medications. |
Combined Therapeutic Approaches
Combining SSRIs with other therapeutic approaches can significantly enhance treatment outcomes. Psychotherapy, such as cognitive behavioral therapy (CBT), can provide valuable coping mechanisms and address underlying psychological factors contributing to the condition. Lifestyle modifications, including regular exercise, balanced nutrition, and stress management techniques, can further support overall well-being and improve treatment response. Examples of successful combined approaches include CBT paired with a gradual increase in Prozac dosage for a patient experiencing anxiety.
Last Point: Prozac Fluoxetine Vs Lexapro Escitalopram
In conclusion, choosing between Prozac and Lexapro depends significantly on individual patient needs and responses. Factors like patient history, potential side effects, and the specific symptoms being treated play critical roles. Open communication with a healthcare professional is paramount to determine the most suitable treatment strategy, considering the complexities of each individual’s situation. This comparison provides a framework for understanding these medications but does not substitute professional medical advice.