What is TMJ disorder? This comprehensive guide delves into the complexities of temporomandibular joint (TMJ) disorders, exploring everything from their intricate anatomy to effective treatment options. Understanding the structure and function of the TMJ is crucial to grasping the various types of TMJ disorders and their associated symptoms. We’ll also explore the causes, diagnosis, and available self-care strategies.
From the subtle aches and pains to the more pronounced symptoms, this guide will equip you with the knowledge needed to navigate the world of TMJ disorders. We’ll break down the different types of TMJ disorders, examining their unique characteristics and how they affect daily life. A detailed comparison table will visually illustrate the key differences between the TMJ and other similar joints.
Introduction to Temporomandibular Joint Disorder (TMJ)
Temporomandibular joint disorder (TMJD), often referred to as TMJ disorder, encompasses a range of conditions affecting the temporomandibular joint (TMJ). These conditions can cause pain, discomfort, and limited movement of the jaw. Understanding the anatomy and function of the TMJ is crucial for comprehending TMJ disorders.TMJ disorders are a complex group of conditions affecting the jaw joint and the surrounding muscles responsible for jaw movement.
These conditions can manifest as pain, clicking, or popping sounds in the jaw, difficulty opening or closing the mouth, and headaches. The pain and dysfunction can significantly impact daily life, affecting eating, speaking, and even sleep.
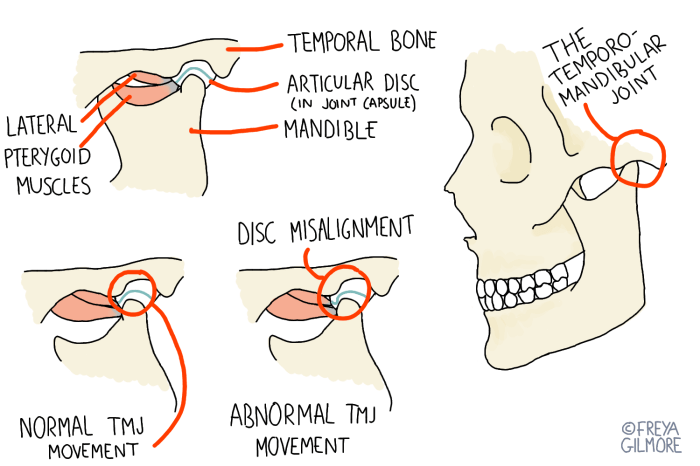
Anatomy of the Temporomandibular Joint
The temporomandibular joint (TMJ) is a unique joint connecting the mandible (lower jaw) to the temporal bone of the skull. It’s a bilateral joint, meaning there’s one on each side of the face. Crucially, the TMJ’s structure allows for a wide range of movements, including opening, closing, and side-to-side movement of the jaw. The joint is composed of articular cartilage covering the condyle of the mandible and the temporal bone.
A complex network of ligaments and muscles surrounds the joint, providing stability and control over its movement. The joint capsule encloses the articular surfaces and contains synovial fluid, lubricating the joint and facilitating smooth movement.
Normal Function of the Temporomandibular Joint
The normal function of the TMJ involves a precise interplay of bone, cartilage, ligaments, and muscles. The joint allows for a variety of jaw movements, including opening and closing, chewing, and speaking. The condyle of the mandible glides smoothly within the mandibular fossa of the temporal bone, enabling the intricate motions needed for these activities. The smooth gliding motion is supported by the synovial fluid, which acts as a lubricant, reducing friction and wear and tear on the joint surfaces.
Muscles attached to the mandible, such as the masseter and temporalis muscles, work in coordination with the joint to control and execute these movements.
Comparison of TMJ to Another Joint
The TMJ, while unique, shares some functional similarities with other joints in the body. Here’s a comparison to the knee joint, a commonly understood and structurally complex joint:
| Feature | TMJ | Knee Joint |
|---|---|---|
| Structure | Condylar joint with articular cartilage, ligaments, and a synovial membrane. The mandibular condyle glides within the mandibular fossa of the temporal bone. | Synovial hinge joint with menisci (meniscus) and ligaments, connecting the femur and tibia. |
| Function | Allows for opening, closing, and side-to-side movement of the jaw. Crucial for chewing, speaking, and facial expression. | Allows for flexion, extension, and rotation of the leg. Critical for walking, running, and other movements. |
| Motions | Complex gliding and rotational movements. | Mainly hinge movements, but also some rotation. |
Types of TMJ Disorders
Temporomandibular joint (TMJ) disorders encompass a range of conditions affecting the jaw joint and surrounding muscles. While often grouped together, these disorders can manifest in distinct ways, impacting daily life and requiring different treatment approaches. Understanding the various types and their characteristics is crucial for accurate diagnosis and effective management.
Classifications of TMJ Disorders
TMJ disorders are broadly categorized into internal derangements and other forms of TMJ dysfunction. Internal derangements involve displacement or damage within the joint itself, while other forms encompass a wider spectrum of problems, such as muscle pain and inflammation. This distinction helps in understanding the root cause of the discomfort and tailoring the treatment plan accordingly.
Internal Derangements, What is tmj disorder
Internal derangements of the TMJ are characterized by the displacement or damage of the articular disc, a cushion-like structure within the joint. This displacement can lead to a variety of symptoms, ranging from mild discomfort to significant pain and limited jaw movement. Common types include:
- Disc Displacement with Reduction: The disc can move out of place but spontaneously return to its normal position. This type often presents with clicking or popping sounds in the jaw, along with intermittent pain.
- Disc Displacement without Reduction: In this case, the disc is permanently displaced, preventing it from returning to its normal position. This often leads to persistent pain, limited jaw movement, and a feeling of locking or catching in the jaw.
Other Forms of TMJ Dysfunction
Other forms of TMJ dysfunction encompass a wider range of conditions affecting the jaw muscles and surrounding tissues. These conditions are often linked to factors like stress, bruxism (teeth grinding), or even arthritis.
- Myofascial Pain: This condition involves pain and tenderness in the muscles surrounding the jaw joint. The pain can be diffuse or localized, often radiating to the temples, neck, or ears. Stress and repetitive jaw movements are frequently implicated.
- Arthritis: Inflammation of the TMJ, often due to osteoarthritis or rheumatoid arthritis, can lead to pain, stiffness, and limited jaw movement. The symptoms can be gradual or sudden, depending on the severity of the underlying condition.
- Bruxism: Habitual teeth grinding, often occurring during sleep, can put excessive strain on the TMJ. This can lead to muscle pain, headaches, and tooth wear. While bruxism itself isn’t a specific TMJ disorder, it frequently contributes to TMJ dysfunction.
Summary Table of TMJ Disorders
| Type of TMJ Disorder | Description | Symptoms | Causes |
|---|---|---|---|
| Disc Displacement with Reduction | The articular disc moves out of place but spontaneously returns to its normal position. | Clicking or popping sounds in the jaw, intermittent pain. | Trauma, repetitive jaw movements. |
| Disc Displacement without Reduction | The articular disc is permanently displaced, preventing it from returning to its normal position. | Persistent pain, limited jaw movement, locking or catching in the jaw. | Trauma, gradual degeneration. |
| Myofascial Pain | Pain and tenderness in the muscles surrounding the jaw joint. | Diffuse or localized pain, radiating to temples, neck, or ears. | Stress, repetitive jaw movements, bruxism. |
| Arthritis | Inflammation of the TMJ, often due to osteoarthritis or rheumatoid arthritis. | Pain, stiffness, limited jaw movement. | Degenerative processes, autoimmune response. |
| Bruxism | Habitual teeth grinding, often occurring during sleep. | Muscle pain, headaches, tooth wear. | Stress, anxiety, sleep disorders. |
Symptoms and Diagnosis
Identifying TMJ disorder often begins with recognizing the various symptoms. A thorough understanding of these symptoms, coupled with appropriate diagnostic methods, is crucial for accurate identification and effective treatment. Accurate diagnosis allows for personalized treatment plans tailored to individual needs, ultimately leading to improved quality of life for those affected.Understanding the specific symptoms and diagnostic approaches is paramount to recognizing and addressing TMJ disorder effectively.
This knowledge empowers individuals to seek timely medical attention, enabling prompt intervention and management of the condition. Furthermore, an understanding of the role of medical imaging aids in a more precise diagnosis.
Common Symptoms of TMJ Disorder
TMJ disorder presents a diverse range of symptoms, impacting not only the jaw but also related areas. Recognizing these varied symptoms is essential for prompt diagnosis and appropriate treatment. Common symptoms often include:
- Jaw pain: This pain can manifest as a dull ache, sharp pain, or a throbbing sensation, localized around the jaw joint or radiating to other areas. It may worsen with chewing or jaw movement.
- Facial pain: Pain may extend to the temples, ears, or even the neck and shoulders. This often occurs alongside jaw pain, contributing to the overall discomfort.
- Clicking or popping sounds in the jaw: These sounds are often perceived during jaw opening or closing, sometimes accompanied by a grinding or grating sensation.
- Limited jaw movement: Difficulty opening or closing the mouth, or a restricted range of motion, can significantly affect daily activities.
- Headaches: Tension headaches or migraines can frequently accompany TMJ disorder, adding to the overall discomfort.
- Earaches: While not always directly related to the ear itself, pain or discomfort in the ear region is a symptom often associated with TMJ disorder.
Diagnostic Methods for TMJ Disorder
Diagnosis of TMJ disorder involves a multifaceted approach, combining a thorough patient history with physical examination and potentially, medical imaging.
- Patient History: A detailed account of symptoms, including their onset, frequency, and any associated factors, forms the foundation of the diagnostic process. The history also includes any past medical conditions, recent dental work, or any trauma to the head or neck.
- Physical Examination: A physical examination of the jaw joint, including palpation (feeling with fingers) to identify tenderness, clicking, or limited movement, is essential. The examiner assesses the alignment and symmetry of the jaw, along with the range of motion.
Role of Medical Imaging in Diagnosis
Medical imaging plays a crucial role in confirming a diagnosis or identifying underlying structural issues contributing to TMJ symptoms. Various imaging techniques are used depending on the specific suspicion.
- X-rays: Standard X-rays provide images of the jaw joint’s bony structures, allowing visualization of potential abnormalities such as fractures, dislocations, or degenerative changes. X-rays can reveal the extent of bone erosion, which can be an indication of severe TMJ issues.
- CT scans: Computed tomography (CT) scans offer detailed cross-sectional views of the jaw joint, providing a comprehensive view of both bone and soft tissue structures. CT scans are particularly helpful in detecting complex bone structures and potential complications.
- MRI scans: Magnetic resonance imaging (MRI) scans offer detailed images of the soft tissues within the jaw joint, including ligaments, tendons, and muscles. MRI scans are often used to identify soft tissue injuries, tears, or other structural abnormalities that might be causing the symptoms.
Diagnostic Flowchart for TMJ Disorders
A flowchart can illustrate the systematic approach to diagnosing TMJ disorders:
| Step | Action |
|---|---|
| 1 | Obtain detailed patient history and describe symptoms. |
| 2 | Perform physical examination of the jaw joint, focusing on range of motion, palpation, and presence of clicking/popping sounds. |
| 3 | Based on the initial assessment, consider appropriate medical imaging (X-rays, CT, or MRI) if needed. |
| 4 | Interpret medical imaging results to identify any structural abnormalities or underlying causes. |
| 5 | Consult with a specialist (dentist or oral surgeon) for a comprehensive diagnosis and treatment plan. |
Causes of TMJ Disorders: What Is Tmj Disorder
Understanding the causes of temporomandibular joint (TMJ) disorders is crucial for effective management and prevention. Various factors contribute to the development of these disorders, ranging from genetic predispositions to lifestyle habits. Pinpointing the specific cause often requires a comprehensive evaluation by a healthcare professional.
Potential Causes of TMJ Disorders
TMJ disorders aren’t always easily traced to a single cause. Often, a combination of factors, including genetics, environmental influences, and lifestyle choices, plays a role in their development. This complexity makes diagnosis and treatment challenging, but also highlights the importance of a multifaceted approach to care.
Role of Genetics
Genetic predisposition plays a significant role in some individuals’ susceptibility to TMJ disorders. Family history of TMJ problems can indicate a genetic link, increasing the likelihood of developing the disorder. Inherited traits can affect the structure and function of the jaw joint, making it more prone to dysfunction. This genetic component underscores the importance of considering family history when assessing risk.
Lifestyle Factors and TMJ
Lifestyle factors significantly impact the health of the TMJ. Chronic teeth grinding (bruxism) is a frequent culprit. The repetitive pressure exerted on the jaw joints can lead to pain, inflammation, and eventual damage. Similarly, improper posture and prolonged periods of stress can contribute to muscle tension around the jaw, exacerbating existing TMJ issues.
Specific Situations Contributing to TMJ Disorders
Certain situations can place increased stress on the TMJ, potentially leading to dysfunction. For example, forceful chewing, such as when consuming very hard or sticky foods, can strain the joint and surrounding muscles. Similarly, trauma to the jaw, such as a blow to the face, can result in TMJ disorders. Professional athletes involved in contact sports, such as boxing or hockey, might experience TMJ issues due to frequent impacts.
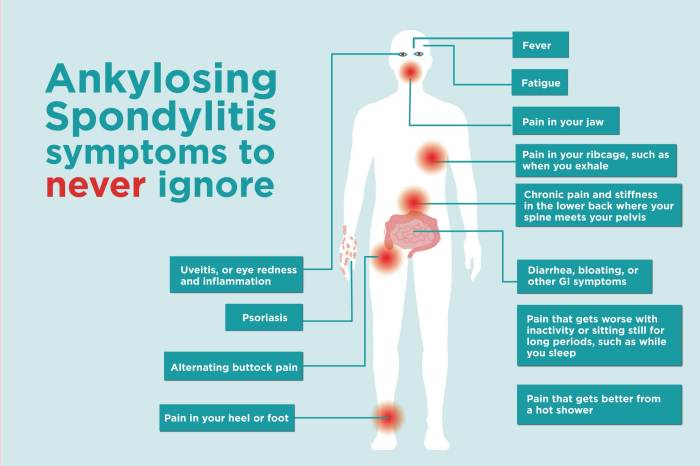
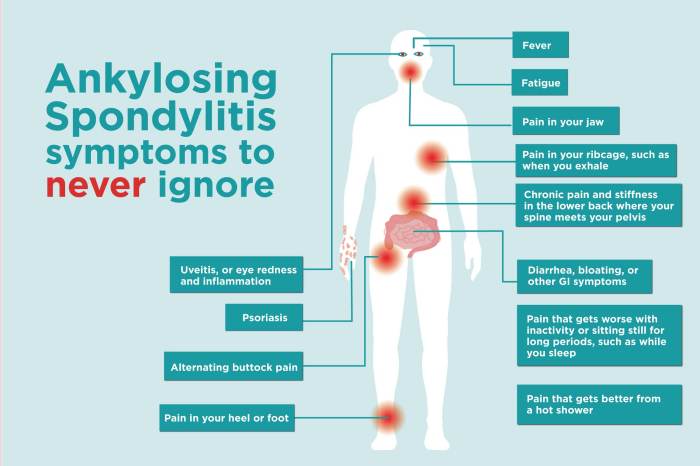
TMJ disorder, or temporomandibular joint disorder, is a tricky one. It involves pain and dysfunction in the jaw joint, and can manifest in various ways. Sometimes, it’s hard to tell if it’s a cold or COVID-19, as some symptoms overlap. If you’re unsure about the cause of your discomfort, checking out resources like do i have a cold or covid can help differentiate between the two.
Ultimately, though, if you’re experiencing jaw pain, it’s best to consult a healthcare professional to properly diagnose and treat TMJ disorder.
Risk Factors for TMJ Disorders
Several risk factors increase the likelihood of developing TMJ disorders. These factors include:
- Family history of TMJ disorders: A family history of TMJ problems can significantly increase the risk of developing the condition.
- Chronic teeth grinding (bruxism): Repetitive grinding of teeth, often during sleep, can put significant stress on the jaw joint and contribute to TMJ issues.
- Poor posture: Maintaining poor posture can lead to muscle tension in the neck and jaw area, potentially exacerbating existing TMJ problems or contributing to new ones.
- Stress and anxiety: Chronic stress and anxiety can lead to muscle tension, including those surrounding the jaw, increasing the risk of TMJ disorders.
- Previous jaw injuries: Past trauma to the jaw, such as fractures or dislocations, can increase the likelihood of developing TMJ problems later in life.
- Certain medical conditions: Conditions such as arthritis can impact the jaw joint and increase the risk of TMJ disorders.
Treatment Options

Managing temporomandibular joint (TMJ) disorders often involves a multifaceted approach, tailoring treatment to the specific type and severity of the condition. A comprehensive strategy typically begins with conservative measures and progresses to more invasive options if necessary. The goal is to alleviate symptoms, restore function, and prevent further complications.Effective treatment for TMJ disorders hinges on understanding the underlying cause and the patient’s individual needs.
A collaborative effort between the patient and healthcare provider is essential for achieving optimal outcomes.
Conservative Treatments
Conservative treatments aim to alleviate symptoms and improve joint function without surgery. These approaches typically address the underlying causes and contributing factors, such as muscle tension, stress, and bruxism.
- Physical Therapy: Physical therapy exercises focus on strengthening the muscles of mastication (chewing) and improving joint mobility. This may include manual therapy, stretching, and specific exercises designed to reduce pain and improve range of motion. A physical therapist can provide tailored exercises and guidance to help manage TMJ pain effectively.
- Medications: Over-the-counter pain relievers, such as ibuprofen or naproxen, can help reduce pain and inflammation. Prescription medications, such as muscle relaxants or anti-inflammatory drugs, may be necessary in more severe cases. These medications aim to manage symptoms, but may not address the root cause of the disorder.
- Stress Management Techniques: Stress plays a significant role in many TMJ disorders. Techniques like relaxation exercises, meditation, biofeedback, and counseling can help reduce stress levels, which in turn can alleviate TMJ pain and dysfunction. Chronic stress can contribute to muscle tension, further exacerbating TMJ symptoms. Addressing stress through various techniques can lead to significant improvements in pain management.
- Occlusal Splints/Guards: These custom-fitted appliances are worn over the teeth to reduce the pressure on the TMJ. They can help prevent teeth grinding (bruxism) and correct misalignment of the jaw. Occlusal splints are particularly effective in cases where bruxism is a significant factor in TMJ disorder. By preventing the grinding and clenching of teeth, these splints can protect the jaw and surrounding tissues, offering substantial pain relief.
Surgical Treatments
Surgical interventions are typically reserved for cases where conservative treatments have failed to provide adequate relief. These procedures aim to correct structural problems within the TMJ, often addressing joint damage or malocclusion.
- Arthrocentesis: This minimally invasive procedure involves injecting a sterile solution into the joint to flush out debris and reduce inflammation. It’s a relatively safe procedure with minimal recovery time compared to other surgical options.
- Arthroscopy: Using small incisions and a camera, arthroscopy allows surgeons to visualize and repair damaged joint tissues. This approach can be used to address issues like loose bodies, cartilage damage, or inflammation within the joint.
- Open Joint Surgery: This more extensive procedure involves a larger incision to directly address more complex structural problems. It’s typically reserved for cases with significant joint damage or malocclusion that haven’t responded to less invasive treatments. While it can provide long-term solutions for severe TMJ problems, it carries a higher risk of complications and a longer recovery period.
Effectiveness and Limitations
The effectiveness of TMJ treatment varies significantly depending on the individual, the type of disorder, and the chosen treatment approach. Conservative treatments are generally more effective in cases of mild to moderate TMJ disorders, where the underlying causes are amenable to non-surgical interventions. Surgical treatments are often reserved for more severe cases, where structural damage has significantly impacted joint function and pain.
It is important to discuss potential benefits and risks with a healthcare professional before deciding on a course of action.
Self-Care and Prevention
Taking proactive steps to manage TMJ symptoms and prevent future issues is crucial. Self-care strategies can significantly reduce pain and discomfort, improving overall quality of life. This section Artikels practical techniques for home management, exercises, and lifestyle adjustments to minimize the risk of TMJ disorders.Effective self-management involves understanding the triggers of your TMJ pain and implementing strategies to mitigate those triggers.
Early intervention and consistent self-care can help prevent the progression of the condition and reduce the need for more invasive treatments.
Home Management Techniques
Understanding and managing triggers is key to effective home treatment. Identifying activities or situations that exacerbate TMJ pain allows for targeted preventative measures. Resting the jaw, applying ice packs to the affected area, and using over-the-counter pain relievers are common, effective techniques.
TMJ disorder, or temporomandibular joint disorder, can cause a lot of pain and discomfort in your jaw. It’s often tricky to diagnose, but sometimes it’s linked to other conditions. For example, some people with rheumatoid arthritis might find that medications like DMARDs for rheumatoid arthritis, dmards for rheumatoid arthritis , can help alleviate some of the symptoms.
Ultimately, understanding TMJ disorder involves considering various factors, and seeking professional medical advice is crucial for proper diagnosis and treatment.
- Resting the Jaw: Avoid activities that put excessive strain on the jaw, such as chewing gum, biting hard foods, or forcefully clenching the teeth. Simple rest periods throughout the day can be highly beneficial.
- Applying Ice Packs: Applying ice packs to the affected area for 15-20 minutes at a time, several times a day, can help reduce inflammation and pain.
- Over-the-Counter Pain Relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen or naproxen, can help alleviate pain and inflammation.
Jaw Exercises and Stretches
Specific exercises and stretches can strengthen the muscles supporting the jaw and improve flexibility, helping to alleviate pain and discomfort. Consistency is key to achieving results.
TMJ disorder, or temporomandibular joint disorder, is a common issue causing jaw pain and discomfort. Sometimes, managing the pain involves exploring options like prescription and OTC drugs, which can help alleviate symptoms. For example, certain medications can help reduce inflammation or muscle spasms associated with TMJ. Finding the right approach to managing TMJ pain often involves exploring various treatment options, including exploring the potential benefits of different prescription and OTC drugs.
Ultimately, proper diagnosis and a tailored treatment plan are key to effectively managing TMJ disorder.
- Gentle Jaw Movements: Slowly open and close your mouth several times a day, ensuring the movement is controlled and pain-free. Avoid any jerky or forceful motions.
- Side-to-Side Jaw Movements: Slowly move your jaw from side to side, keeping the movement gentle and within comfortable limits. Repeat this exercise several times a day.
- Chin Tucks: Gently tuck your chin towards your chest, holding the position for a few seconds, then releasing. Repeat this exercise several times, ensuring no pain is experienced.
Lifestyle Modifications
Certain lifestyle choices can significantly influence the development and progression of TMJ disorders. Adopting healthier habits can contribute to reducing the risk of TMJ problems.
- Stress Management Techniques: Stress is often a contributing factor to TMJ pain. Incorporating stress-reducing activities like meditation, yoga, or deep breathing exercises can help manage stress levels.
- Proper Posture: Maintaining good posture throughout the day can help to minimize strain on the jaw and neck muscles.
- Hydration: Drinking plenty of water helps keep the soft tissues of the jaw hydrated, potentially reducing discomfort.
- Balanced Diet: A balanced diet with a focus on soft foods can reduce the strain on the jaw muscles. Avoid excessive chewing or biting on hard foods.
Self-Care Routine
A consistent self-care routine is essential for managing TMJ symptoms and promoting overall well-being. It is crucial to establish a routine that includes both physical and mental components.
- Daily Exercise Routine: Incorporating gentle jaw exercises and stretches into your daily routine helps maintain jaw flexibility and reduce pain.
- Stress Reduction Practices: Regular stress-reduction techniques, like meditation or yoga, help manage stress, a common trigger for TMJ symptoms.
- Regular Check-ups: Maintaining regular check-ups with your dentist or a TMJ specialist ensures early detection and management of potential problems.
Prognosis and Long-Term Management
TMJ disorders can range in severity and impact on daily life. Understanding the potential outcomes and the importance of consistent long-term management is crucial for achieving the best possible quality of life. While many people experience significant improvement with appropriate treatment, some individuals may require ongoing care and adjustments to lifestyle.The prognosis for TMJ disorders varies considerably depending on factors like the specific type of disorder, the severity of symptoms, and the individual’s response to treatment.
Early intervention and adherence to a well-structured management plan often lead to better outcomes. This involves a proactive approach to managing the condition, anticipating potential challenges, and fostering a collaborative relationship with healthcare providers.
Potential Outcomes of TMJ Disorders
TMJ disorders can manifest in various ways, leading to a spectrum of potential outcomes. Some individuals experience temporary discomfort that resolves with conservative treatments. Others may experience persistent symptoms that require more intensive interventions. The potential outcomes include complete resolution of symptoms, substantial improvement in symptoms, or the need for ongoing management strategies to maintain a manageable level of discomfort.
Chronic pain and dysfunction may persist, impacting quality of life and requiring long-term strategies for pain management and symptom control.
Importance of Long-Term Management Strategies
Long-term management is essential for achieving and maintaining optimal well-being for individuals with TMJ disorders. This proactive approach goes beyond addressing immediate symptoms and focuses on preventing future complications and maintaining a high quality of life. Proactive management helps to reduce the likelihood of symptom flare-ups and long-term disability.
Role of Follow-Up Care in Managing TMJ
Regular follow-up appointments with a healthcare professional are crucial in the management of TMJ disorders. These appointments provide opportunities for monitoring the effectiveness of treatment, adjusting the treatment plan as needed, and addressing any new concerns or symptoms that may arise. Regular check-ups enable early detection of potential complications, enabling timely interventions and minimizing the impact on overall health.
Follow-up care should be tailored to the individual’s specific needs and the nature of their TMJ disorder.
Potential Complications if TMJ Disorders are Left Untreated
Untreated TMJ disorders can lead to a range of complications. Persistent pain and discomfort can negatively affect daily activities, including eating, speaking, and sleeping. Chronic pain can lead to anxiety and depression, impacting mental health and overall well-being. Joint damage and dysfunction can also develop over time, potentially requiring more complex and invasive interventions in the future.
Examples include limited jaw movement, irreversible joint damage, and the development of chronic facial pain. In some cases, untreated TMJ disorders can also contribute to headaches and other musculoskeletal problems.
Closing Summary

In conclusion, TMJ disorders, while potentially debilitating, are often manageable with the right knowledge and care. This guide has provided a comprehensive overview of the condition, equipping you with insights into its various aspects, from anatomy and function to treatment options and self-care strategies. Remember, seeking professional medical advice is essential for accurate diagnosis and personalized treatment plans.