What medications cause sundowning symptoms? This exploration delves into the often-overlooked connection between prescription drugs and the distressing phenomenon of sundowning. Sundowning, characterized by a decline in cognitive function and behavioral changes, typically occurring in the late afternoon or evening, can significantly impact individuals and their caregivers. While various factors contribute to sundowning, understanding the role of medications is crucial for effective management.
We’ll uncover common culprits, examine potential interactions, and discuss strategies for monitoring and mitigating the impact on patients.
Sundowning symptoms, often associated with conditions like dementia and Alzheimer’s, can manifest as agitation, confusion, and disorientation. Medications can sometimes exacerbate these symptoms, making it essential to explore the link between specific drugs and this distressing pattern. This article aims to provide a comprehensive overview of the potential triggers, enabling caregivers and medical professionals to make informed decisions about medication management and overall care.
Introduction to Sundowning Symptoms
Sundowning symptoms, a common phenomenon in aging and cognitive decline, manifest as a worsening of behavioral and cognitive function in the late afternoon or evening hours. These symptoms can range from subtle changes in mood to significant disruptions in daily life, impacting both the individual experiencing them and those who care for them. Understanding the nature of sundowning, its potential causes, and the impact it has is crucial for providing effective support and care.
Definition of Sundowning Symptoms
Sundowning symptoms are characterized by a decline in cognitive function and behavioral changes that become more pronounced during the late afternoon and evening hours. This includes increased confusion, agitation, disorientation, and difficulty with communication. Sundowning is a broad term encompassing a spectrum of potential symptoms, from mild mood swings to severe behavioral disturbances.
Typical Characteristics and Behaviors
Sundowning symptoms often include increased restlessness, irritability, confusion, and difficulty with tasks requiring concentration. Individuals may exhibit wandering, aggression, or hallucinations. These symptoms can vary in intensity, but they typically emerge in the late afternoon or evening and subside or lessen with the onset of sleep.
Common Causes of Sundowning (Excluding Medications)
Sundowning is not a single condition, but rather a constellation of symptoms potentially stemming from several factors. Common causes include: changes in the body’s natural circadian rhythms, sleep disturbances, sensory overload, and environmental factors such as noise or lack of familiarity in a setting. Cognitive decline, particularly in conditions like Alzheimer’s disease and dementia, can exacerbate these symptoms.
Impact of Sundowning on Individuals and Caregivers
Sundowning symptoms significantly impact the quality of life for individuals experiencing them, often leading to feelings of isolation, frustration, and distress. For caregivers, it can be challenging to manage the increased agitation and confusion, often resulting in emotional exhaustion and stress. The unpredictability of sundowning can lead to significant difficulties in daily routines and create a constant sense of worry for both the individual and the caregiver.
Stages of Sundowning Severity
| Stage | Description | Impact on Daily Life |
|---|---|---|
| Mild | Occasional confusion, mood swings, and slight restlessness in the late afternoon or evening. Changes are noticeable but do not significantly disrupt daily activities. | Minor adjustments to schedules or routines might be necessary. |
| Moderate | Increased confusion, agitation, and disorientation in the late afternoon and evening. Tasks requiring concentration become challenging. Wandering or disruptive behaviors may appear. | Significant disruptions to daily routines, requiring increased supervision and support. |
| Severe | Extreme confusion, aggression, hallucinations, and severe disorientation in the late afternoon and evening. Individuals may exhibit significant safety concerns. | Requires constant supervision and specialized care. The safety and well-being of the individual and those around them are at risk. |
Medications Potentially Linked to Sundowning
Sundowning, a phenomenon characterized by increased agitation, confusion, and disorientation in the late afternoon and evening, can be influenced by a variety of factors, including medications. Understanding which medications might contribute to these symptoms is crucial for personalized care plans and symptom management. This section explores the link between specific medications and sundowning, highlighting potential mechanisms and providing examples.Medications can disrupt the delicate balance of neurochemicals in the brain, potentially exacerbating pre-existing cognitive impairments or introducing new symptoms.
The effects of certain drugs, particularly those with sedative or stimulating properties, can manifest as sundowning. Dosage, duration of use, and individual patient responses all play a role in the relationship between medications and sundowning.
Common Medications Potentially Contributing to Sundowning
Many medications, regardless of their intended purpose, can influence the brain’s chemistry, leading to sundowning-like symptoms. Understanding these effects is vital for healthcare professionals and caregivers.
- Anticholinergics: These medications block the action of acetylcholine, a neurotransmitter crucial for cognitive function and alertness. Anticholinergics can cause confusion, memory problems, and disorientation, symptoms often seen in sundowning. Examples include some antihistamines, tricyclic antidepressants, and certain Parkinson’s medications. High doses or prolonged use are often associated with these symptoms.
- Sedatives and Hypnotics: Medications used to induce sleep or reduce anxiety can lead to daytime fatigue and nighttime restlessness, creating a cycle that mirrors sundowning. This is particularly relevant for individuals with pre-existing sleep disorders. Benzodiazepines and some over-the-counter sleep aids fall into this category. Extended use or high doses can exacerbate these effects.
- Antipsychotics: While often used to treat psychosis, certain antipsychotic medications can cause confusion and agitation, contributing to sundowning. The specific mechanisms are complex, but include disruptions in neurotransmitter balance. The duration of use and individual tolerance play a critical role in assessing potential impacts.
- Pain Medications: Opioids and some nonsteroidal anti-inflammatory drugs (NSAIDs) can affect cognitive function and sleep patterns, potentially contributing to sundowning. The effects can be more pronounced in individuals with pre-existing cognitive impairment or in those taking multiple medications. Dosages and durations are crucial factors to consider in relation to sundowning.
Dosage and Duration Considerations, What medications cause sundowning symptoms
The relationship between medication dosage, duration of use, and the potential for sundowning is complex. A higher dosage or longer duration of use can intensify the impact of certain medications on cognitive function and sleep patterns.
- High Doses: Higher-than-recommended dosages of medications can more significantly affect cognitive functions and sleep cycles, increasing the likelihood of sundowning. This is particularly relevant for medications known to have a narrow therapeutic index.
- Prolonged Use: Prolonged use of medications can lead to tolerance and the development of compensatory mechanisms. However, in some cases, this can lead to a cumulative effect that contributes to sundowning. Long-term use of certain medications can also lead to the development of cognitive impairment.
Medication Type and Sundowning Impact Comparison
This table summarizes the potential impact of different medication types on sundowning symptoms. It is important to remember that individual responses vary, and this is not an exhaustive list.
| Medication Type | Potential Impact on Sundowning | Examples |
|---|---|---|
| Anticholinergics | Increased confusion, disorientation, and memory problems | Some antihistamines, tricyclic antidepressants, Parkinson’s medications |
| Sedatives/Hypnotics | Daytime fatigue, nighttime restlessness, sleep disturbances | Benzodiazepines, some over-the-counter sleep aids |
| Antipsychotics | Confusion, agitation, and sleep disturbances | Various antipsychotic medications |
| Pain Medications (e.g., Opioids, NSAIDs) | Cognitive impairment, sleep disturbances | Opioids, some NSAIDs |
Potential Interactions and Combinations
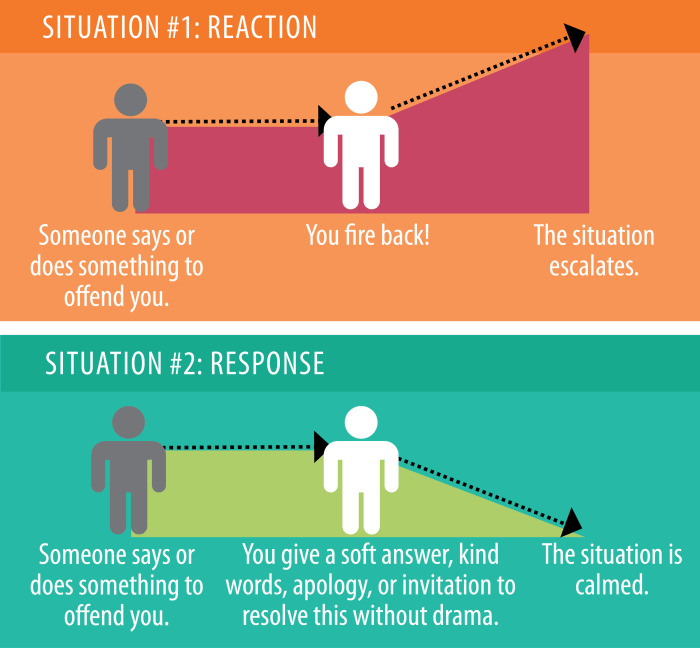
Sundowning, characterized by a decline in cognitive function and behavioral changes in the late afternoon and evening, can be significantly influenced by medication interactions. Understanding these interactions is crucial for effective management and improving the quality of life for individuals experiencing sundowning. A comprehensive approach to medication review is vital, especially when dealing with complex medical conditions that often involve multiple medications.Medication interactions can exacerbate sundowning symptoms by altering the effectiveness or side effects of individual drugs.
This is particularly true when several medications are taken simultaneously. Polypharmacy, the practice of taking multiple medications, is common, especially for older adults with complex health issues. However, this increased use of medications can also lead to unwanted and potentially dangerous interactions.
Certain medications can unfortunately trigger sundowning symptoms, making it harder to sleep and more likely to experience confusion. Sometimes, these symptoms can manifest as a tingling sensation in the head scalp, which can be a bit disconcerting. If you’re experiencing this, it’s crucial to consult your doctor to determine if there’s a connection to the medications you’re taking or explore other underlying causes, like those related to tingling sensation in head scalp.
Understanding the potential links between medications and sundowning is key to managing these effects and improving overall well-being.
Potential Medication Combinations Increasing Sundowning Risk
Certain combinations of medications can increase the risk of sundowning symptoms. For instance, combining sedative medications with other drugs that also have sedative properties can lead to excessive drowsiness and confusion, mirroring the characteristics of sundowning. Similarly, medications affecting the central nervous system, including those used for anxiety or depression, can, when combined, potentially worsen sundowning symptoms. Careful consideration of drug interactions is essential in managing sundowning.
Importance of Comprehensive Medication Reviews
A thorough medication review is critical for individuals experiencing sundowning. This review should consider all medications, including prescription drugs, over-the-counter medications, supplements, and herbal remedies. The review should meticulously analyze the potential for interactions between medications and their potential to contribute to sundowning symptoms. By identifying these interactions, healthcare providers can adjust medication regimens to minimize or eliminate the risk of sundowning.
This approach is essential to create personalized strategies for optimal health and well-being.
Examples of Medications Potentially Contributing to Sundowning
Numerous medications have the potential to contribute to sundowning. For instance, certain anticholinergics, commonly used to treat urinary issues, can cause cognitive impairment and behavioral changes, sometimes mimicking sundowning symptoms. Furthermore, some medications used to treat hypertension or other cardiovascular conditions can potentially exacerbate cognitive decline. Similarly, some antidepressants and antipsychotics can have side effects that contribute to sundowning symptoms.
Table of Potential Drug Interactions and Sundowning
| Medication Class | Example Medications | Potential Interaction | Potential Impact on Sundowning |
|---|---|---|---|
| Anticholinergics | Benztropine, scopolamine | Increased central nervous system effects when combined with other sedatives or anticholinergics | Increased drowsiness, confusion, and cognitive impairment, potentially worsening sundowning. |
| Sedatives | Benzodiazepines, some antihistamines | Additive sedative effects when combined with other sedatives or central nervous system depressants. | Exacerbation of drowsiness, confusion, and cognitive impairment, resembling sundowning patterns. |
| Antipsychotics | Haloperidol, risperidone | Potential for increased central nervous system effects when combined with other drugs affecting the nervous system. | Increased cognitive impairment, potentially mimicking sundowning. |
| Antihypertensives | Some beta-blockers | Potential for interactions with other medications affecting blood pressure or the nervous system. | Possible cognitive impairment or mood changes that might manifest as sundowning symptoms. |
Non-Pharmacological Factors
Sundowning, the worsening of symptoms in the late afternoon or evening, isn’t solely a medication-related issue. Various non-pharmacological factors often play a crucial role in its manifestation and severity. Understanding these factors is key to developing a comprehensive management strategy.Understanding the interplay between medication side effects and non-pharmacological triggers is crucial. For example, a medication might slightly impair sleep, and this sleep disruption could exacerbate sundowning symptoms, making it difficult to isolate the cause.
Sleep Disturbances
Sleep disturbances are frequently implicated in sundowning. These disturbances can manifest in various ways, including difficulty falling asleep, frequent awakenings during the night, and early morning awakenings. These disruptions can lead to fatigue, irritability, and cognitive impairment, all of which can contribute to the progression of sundowning symptoms. Ensuring a consistent sleep schedule and a calming bedtime routine can often help mitigate these issues.
Environmental Changes
Environmental changes can also significantly impact sundowning symptoms. Sudden shifts in lighting, noise levels, or temperature can be especially disruptive to individuals with cognitive impairment. A familiar and predictable environment, with consistent lighting and sounds, can often provide a calming and supportive setting.
Sensory Impairments
Sensory impairments, such as vision or hearing problems, can also contribute to sundowning. If an individual is unable to fully perceive their surroundings, it can create confusion and disorientation, leading to increased agitation and sundowning. Appropriate accommodations, such as assistive devices or modifications to the environment, can often significantly improve the situation.
Non-Medication Interventions
Various non-medication interventions can help reduce sundowning symptoms. These interventions are often crucial in addressing the underlying factors contributing to the symptoms. A holistic approach is often most effective, combining different strategies.
Certain medications can unfortunately trigger sundowning symptoms, a confusing mix of disorientation and agitation in the late afternoon and evening. While exploring the various causes, it’s interesting to consider how conditions like myasthenia gravis and ALS can also impact a person’s well-being, particularly as they relate to the sundowning phenomenon. For a deeper dive into the differences between myasthenia gravis and ALS, check out this helpful resource: myasthenia gravis vs als.
Ultimately, understanding the interplay between medications and sundowning is key to better management and support for those experiencing these symptoms.
- Consistent Routine: Establishing a regular daily schedule, including mealtimes, activities, and bedtime, can provide structure and predictability, reducing confusion and anxiety. A predictable schedule helps maintain a sense of normalcy and security. For instance, a person who typically enjoys a quiet evening reading before bed may find that maintaining this routine significantly mitigates evening agitation.
- Environmental Modifications: Adjusting the environment to create a calming and supportive atmosphere can be very effective. Dim lighting, soft music, and familiar objects can create a sense of comfort and security. Using visual cues, such as clocks and calendars, can also help maintain a sense of time and orientation. Examples include reducing glare, improving lighting, and ensuring that walkways are free of obstacles.
- Sensory Stimulation: Providing appropriate sensory stimulation, such as gentle touch, soft music, or calming aromatherapy, can help reduce anxiety and promote relaxation. Avoid overstimulation, which can worsen agitation. For example, a gentle massage or soft music played in the background can be soothing for someone experiencing sundowning.
- Cognitive Stimulation: Engaging in calming and appropriate cognitive activities, such as puzzles, games, or memory exercises, can help maintain cognitive function and reduce agitation. Activities should be tailored to the individual’s abilities and preferences, avoiding anything too challenging or stimulating. For instance, a simple memory game, like matching pictures, can be engaging and calming.
Importance of a Multifaceted Approach
Managing sundowning effectively often requires a multi-faceted approach that addresses both pharmacological and non-pharmacological factors. This holistic strategy aims to mitigate the impact of both medications and environmental factors.
| Non-Pharmacological Intervention | Potential Effectiveness |
|---|---|
| Consistent Routine | High |
| Environmental Modifications | High |
| Sensory Stimulation | Moderate |
| Cognitive Stimulation | Moderate |
Specific Populations and Sundowning: What Medications Cause Sundowning Symptoms
![[Resource] Is it time to review your medications? - Healthy Aging CORE ... What medications cause sundowning symptoms](https://healthytipp.com/wp-content/uploads/2025/09/13-PRESCRIPTION-MEDICATIONS-1-1.jpg)
Sundowning, the worsening of symptoms in the late afternoon and evening, isn’t a uniform experience. Its manifestation varies significantly across different populations, influenced by underlying conditions and individual factors. Understanding these variations is crucial for tailoring appropriate interventions and support.Sundowning in individuals with cognitive impairments is not simply a matter of worsening symptoms. It’s a complex interplay of factors, including the progression of the underlying condition, medication effects, and environmental stressors.
Certain medications can unfortunately trigger sundowning, a confusing symptom characterized by increased confusion and agitation in the late afternoon and evening. Learning how to manage these symptoms is crucial, and sometimes, that involves adjusting the timing of medications. For example, if you’re dealing with an ostomy appliance, ensuring proper care and timely changes, like in how to change an ostomy appliance , can reduce stress and improve overall well-being, which can also lessen the impact of sundowning-related symptoms.
Ultimately, identifying and managing any underlying medication factors is key to effectively combating sundowning.
For example, someone with mild cognitive impairment might experience subtle changes in mood and behavior, while someone with advanced Alzheimer’s disease might exhibit more pronounced agitation and disorientation. The same medication can affect different individuals in diverse ways.
Dementia-Related Sundowning Variations
Individuals with various types of dementia, such as Alzheimer’s disease, vascular dementia, and Lewy body dementia, can experience different forms of sundowning. The severity and presentation often correlate with the stage of dementia progression. Early-stage dementia may show subtle behavioral changes, while later stages may involve more pronounced confusion, anxiety, and agitation.
Alzheimer’s Disease-Specific Sundowning
In Alzheimer’s disease, sundowning often presents with increased anxiety, wandering, and aggression. These behaviors can be challenging for caregivers, and the intensity of sundowning may fluctuate based on the individual’s specific cognitive and emotional state. The presence of hallucinations or delusions can further complicate the picture.
Influence of Age and Pre-existing Conditions
Age and pre-existing health conditions can influence the impact of medications and environmental factors on sundowning. Older adults may be more susceptible to adverse drug reactions, and co-occurring conditions, such as arthritis or heart disease, can exacerbate sundowning symptoms. For instance, a 70-year-old with Alzheimer’s and arthritis might experience more pronounced sundowning symptoms compared to a 65-year-old with Alzheimer’s alone, especially if they are taking multiple medications.
Comparison of Sundowning Presentations Across Demographics
| Demographic | Typical Sundowning Presentation | Possible Contributing Factors |
|---|---|---|
| Individuals with Mild Cognitive Impairment (MCI) | Subtle changes in mood, increased irritability, and disorientation, often in the late afternoon and evening. | Progression of cognitive decline, medication side effects, and environmental factors. |
| Individuals with Moderate Alzheimer’s Disease | Increased agitation, confusion, wandering, and verbal outbursts. May exhibit more pronounced disorientation. | Progression of cognitive decline, medication side effects, and environmental factors, such as unfamiliar surroundings. |
| Individuals with Severe Alzheimer’s Disease | Extreme agitation, hallucinations, delusions, and aggressive behavior, usually in the late afternoon and evening. | Advanced cognitive decline, medication side effects, sensory overload, and environmental factors. |
| Individuals with Vascular Dementia | Fluctuating levels of confusion, disorientation, and agitation. May present with more pronounced mood swings. | Vascular damage affecting the brain, medication side effects, and environmental factors. |
Monitoring and Management Strategies

Sundowning, a phenomenon characterized by worsening cognitive and behavioral symptoms in the late afternoon or evening, can significantly impact the quality of life for individuals experiencing it. Effective management requires a multi-faceted approach that considers the complex interplay of medications, lifestyle factors, and environmental influences. Monitoring and adapting strategies to address sundowning are crucial for improving well-being and reducing distress.Understanding the intricate relationship between medications and sundowning symptoms is essential for successful management.
Often, adjusting medication regimens, even slightly, can dramatically improve outcomes. Furthermore, lifestyle adjustments and environmental modifications can complement these changes, creating a supportive environment for the individual. Careful monitoring and proactive intervention by healthcare professionals are vital to achieving optimal results.
Importance of Medication Side Effect Monitoring
Medication side effects can contribute significantly to sundowning symptoms. Careful monitoring of current medications is essential. This involves reviewing the individual’s medication list, paying close attention to potential side effects listed by the manufacturer, and noting any reported changes in behavior, mood, or cognition that might coincide with medication administration. This proactive approach allows for early identification of medication-related issues and enables timely adjustments.
Strategies for Managing Sundowning Symptoms
A comprehensive approach to managing sundowning requires a blend of adjustments to medication regimens, lifestyle changes, and environmental modifications. These strategies should be implemented in collaboration with healthcare professionals.
- Medication Adjustments: Adjusting medication dosages or switching to alternative medications may be necessary. For instance, if a particular medication is suspected to be contributing to sundowning symptoms, reducing the dosage or exploring an alternative with a similar therapeutic effect might be beneficial. Healthcare professionals should always be consulted before making any changes to medication regimens. Examples include reducing the dose of a stimulant or switching from a sedative to a less sedating alternative if possible.
It is critical to avoid abrupt changes and to work closely with the prescribing physician.
- Lifestyle Changes: Regular sleep schedules, physical activity, and social engagement can positively influence sundowning symptoms. Consistent sleep patterns are paramount. Encouraging physical activity during the day can also help regulate the individual’s internal clock and contribute to a more restful evening. Meaningful social interactions can combat feelings of isolation and loneliness, both of which can contribute to sundowning symptoms.
Creating a routine and predictable schedule can help to mitigate anxiety and confusion.
- Environmental Modifications: The environment plays a crucial role in managing sundowning. A well-lit, calming environment with clear pathways and minimized clutter can reduce confusion and disorientation. Providing visual cues, such as clocks and calendars, can also assist with maintaining orientation. Reducing noise and distractions can create a more peaceful atmosphere, particularly in the late afternoon and evening.
Minimizing environmental changes that occur at night is important.
Role of Healthcare Professionals
Healthcare professionals, including physicians, nurses, and therapists, play a critical role in assessing and managing sundowning. Their expertise in evaluating the patient’s overall health, medication history, and cognitive function is essential for developing a tailored management plan. This includes performing thorough assessments to identify underlying causes and potential interactions between medications and other factors.
- Assessment and Evaluation: Healthcare professionals should meticulously assess the patient’s medical history, including medications, past diagnoses, and any relevant family history. A thorough cognitive assessment, including memory and attention tests, can help determine the severity of sundowning and identify contributing factors. Careful consideration of the patient’s individual needs and preferences should be prioritized.
- Collaboration and Communication: Open communication among the healthcare team, family members, and caregivers is vital. Sharing information and coordinating care ensures a holistic approach to managing sundowning symptoms. This collaborative effort can lead to a more effective management plan.
Monitoring and Management Strategies Table
| Strategy | Description | Potential Benefits |
|---|---|---|
| Medication Adjustments | Adjusting dosage or switching medications | Reduced sundowning symptoms, improved overall well-being |
| Lifestyle Changes | Regular sleep schedule, physical activity, social engagement | Improved sleep quality, reduced anxiety, increased social interaction |
| Environmental Modifications | Well-lit, calming environment, clear pathways, minimized clutter | Reduced confusion, improved safety, increased sense of security |
| Healthcare Professional Involvement | Comprehensive assessment, medication review, care coordination | Accurate diagnosis, tailored management plan, improved patient outcomes |
Closure
In conclusion, understanding what medications cause sundowning symptoms is vital for effective care. While sundowning isn’t solely caused by medication, the potential impact of specific drugs shouldn’t be underestimated. This discussion highlights the importance of a holistic approach to managing sundowning, encompassing both pharmacological and non-pharmacological interventions. Comprehensive medication reviews, coupled with lifestyle adjustments and environmental modifications, can often significantly improve the quality of life for individuals experiencing sundowning.