Side effects of statins can range from mild discomfort to serious health concerns. This comprehensive guide delves into the potential side effects of statins, exploring everything from common issues like muscle pain to less frequent but potentially severe complications. We’ll cover the science behind these effects, discuss factors that influence their occurrence, and provide practical strategies for managing them.
Understanding the potential side effects is crucial for making informed decisions about statin use.
Statins are a class of medications widely prescribed to lower cholesterol levels. Their mechanism of action involves inhibiting an enzyme crucial for cholesterol production in the liver. Common types include atorvastatin, simvastatin, and rosuvastatin. While statins are generally safe and effective, potential side effects exist. This detailed exploration will help you understand the potential risks and benefits associated with statin therapy.
Introduction to Statins
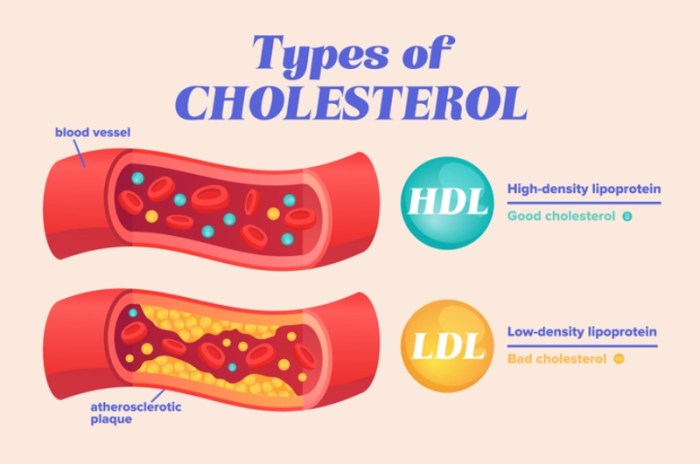
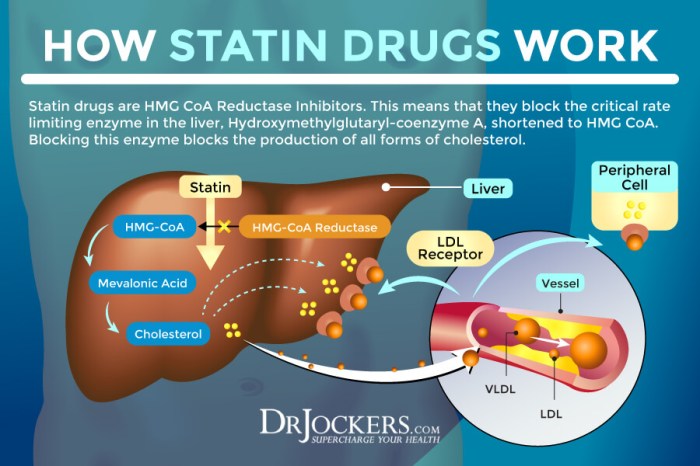
Statins are a class of medications widely prescribed to lower cholesterol levels in the blood. They play a crucial role in managing cardiovascular risk, a leading cause of death globally. Understanding how statins work and their potential side effects is vital for patients and healthcare providers alike.Statins achieve their cholesterol-lowering effects by inhibiting an enzyme called HMG-CoA reductase, a key enzyme in cholesterol synthesis.
By reducing cholesterol production in the liver, statins effectively decrease the amount of cholesterol circulating in the bloodstream. This, in turn, helps to reduce the risk of plaque buildup in arteries, a major contributor to heart disease and stroke.
Common Types of Statins
Various statins are available, each with slightly different properties and potential side effects. Understanding these differences allows for tailored treatment plans based on individual patient needs and characteristics. Common statins include atorvastatin, simvastatin, rosuvastatin, pravastatin, and lovastatin.
Mechanism of Action
Statins work by competitively inhibiting the enzyme HMG-CoA reductase, a crucial enzyme in the mevalonate pathway. This pathway is responsible for the synthesis of cholesterol in the liver. By blocking HMG-CoA reductase, statins reduce the production of cholesterol, leading to a decrease in circulating cholesterol levels. The reduced cholesterol levels help to prevent the buildup of plaque in arteries, thereby reducing the risk of cardiovascular events.
The reduced cholesterol production is a key factor in the efficacy of statins.
Risk-Benefit Profile
The decision to use statins is a complex one, weighing the potential benefits against potential side effects. The benefits often outweigh the risks for individuals at high risk of cardiovascular disease. Factors such as age, family history, lifestyle choices, and current health conditions influence the risk-benefit assessment. The benefits of statin therapy are generally substantial, particularly for patients with elevated cholesterol levels, diabetes, or a history of heart attacks or strokes.
Comparison of Statin Types
| Drug Name | Dosage (mg) | Common Side Effects |
|---|---|---|
| Atorvastatin | 10-80 mg | Muscle pain (myalgia), liver problems, gastrointestinal issues (e.g., nausea, constipation), and headache. |
| Simvastatin | 5-80 mg | Muscle pain (myalgia), liver problems, gastrointestinal issues (e.g., nausea, constipation), and headache. |
| Rosuvastatin | 5-40 mg | Muscle pain (myalgia), liver problems, gastrointestinal issues (e.g., nausea, constipation), and headache. |
| Pravastatin | 10-40 mg | Muscle pain (myalgia), liver problems, gastrointestinal issues (e.g., nausea, constipation), and headache. |
| Lovastatin | 10-80 mg | Muscle pain (myalgia), liver problems, gastrointestinal issues (e.g., nausea, constipation), and headache. |
Note: This table provides a general overview. Specific side effects and dosages may vary based on individual patient factors and the prescribing physician’s recommendations. Always consult with a healthcare professional before starting any new medication. Individual responses to statins can vary. Regular monitoring by a doctor is crucial.
Common Side Effects
Statins, while crucial for managing cholesterol and reducing cardiovascular risk, can sometimes cause unwanted side effects. Understanding these potential issues is vital for patients and healthcare providers to make informed decisions about treatment. Open communication between patients and doctors is key to managing any side effects effectively and ensuring the best possible health outcomes.Statins are a class of medications that work by reducing the production of cholesterol in the liver.
While generally well-tolerated, some individuals experience adverse reactions. The frequency and severity of these side effects vary greatly from person to person. This discussion will explore some of the most common side effects, focusing on the mechanisms behind them and the importance of open communication with healthcare professionals.
Muscle Pain and Damage
Muscle pain, or myalgia, is a frequently reported side effect of statin use. In some cases, this discomfort can progress to more serious muscle damage, known as rhabdomyolysis. This condition occurs when muscle tissue breaks down, releasing harmful substances into the bloodstream.Rhabdomyolysis can be a serious complication, potentially leading to kidney damage or failure. The risk factors for rhabdomyolysis vary, but some individuals are more susceptible than others.
These factors include high doses of statins, pre-existing muscle conditions, and concomitant use of other medications that can interact with statins. Close monitoring of muscle pain and symptoms is crucial.
Liver Enzyme Abnormalities
Statins can sometimes affect liver function, leading to elevated liver enzyme levels. While these abnormalities are typically mild and don’t result in significant liver damage, it’s important to monitor liver function regularly, especially in individuals with pre-existing liver conditions.Elevated liver enzymes can manifest as fatigue, nausea, or abdominal discomfort. Regular blood tests are often part of a patient’s monitoring protocol.
In cases of significant elevation, dosage adjustments or discontinuation of the statin may be necessary.
While researching the side effects of statins, I stumbled upon some interesting parallels with caregiver burnout. Many people taking these medications experience fatigue and muscle pain, which can mirror the exhaustion and emotional strain felt by caregivers. Understanding these symptoms is crucial, especially when considering the toll that caring for a loved one can take. Further exploration into the signs of caregiver burnout, like feeling overwhelmed or detached, can help in recognizing the early warning signs of this important issue.
Ultimately, recognizing these signs and symptoms can help manage the side effects of statins more effectively. signs of caregiver burnout are a valuable resource for anyone experiencing these issues.
Gastrointestinal Issues
Gastrointestinal side effects, such as nausea, vomiting, diarrhea, and abdominal pain, are also possible, though less frequent than muscle-related issues. These symptoms can be uncomfortable and potentially disrupt a patient’s daily life. In many cases, these gastrointestinal symptoms are mild and resolve spontaneously. However, if symptoms persist or worsen, it’s essential to discuss them with a healthcare professional.
Summary of Common Side Effects
| Side Effect | Frequency | Severity |
|---|---|---|
| Muscle pain (myalgia) | Common | Mild to moderate |
| Muscle damage (rhabdomyolysis) | Rare | Potentially severe |
| Liver enzyme abnormalities | Occasional | Mild to moderate, potentially severe in some cases |
| Gastrointestinal issues (nausea, vomiting, diarrhea, abdominal pain) | Occasional | Mild to moderate |
Less Common but Serious Side Effects
While statins are generally safe and effective, some individuals experience less common but potentially serious side effects. Understanding these less frequent complications is crucial for informed decision-making regarding statin use. It’s essential to remember that these side effects are not experienced by everyone taking statins and often can be managed or mitigated.
Neurological Side Effects
Statins can occasionally cause peripheral neuropathy, a condition characterized by damage to the nerves in the extremities. Symptoms can include numbness, tingling, pain, and weakness in the hands and feet. These symptoms can range from mild discomfort to debilitating pain. The exact mechanism by which statins may cause peripheral neuropathy is not fully understood, but it is thought to be related to their effects on the body’s cholesterol metabolism.
It is important to note that these symptoms are typically reversible if statin use is discontinued.
Diabetes-Related Complications
Statins have been linked to an increased risk of developing or worsening type 2 diabetes, particularly in individuals with pre-existing risk factors. This risk is generally considered low but is worth noting. People with a family history of diabetes, obesity, or high blood pressure may be more susceptible to developing diabetes from statin use. Monitoring blood sugar levels regularly is crucial, especially for individuals already at risk of developing or managing diabetes.
Medication Interactions
Statins can interact with other medications, potentially leading to adverse effects. These interactions can range from mild to severe, depending on the specific medications involved. It’s crucial to inform your doctor about all medications you are currently taking, including over-the-counter drugs, supplements, and herbal remedies. Your doctor can assess potential interactions and adjust the dosage of statins or other medications as needed.
Careful monitoring and communication with healthcare providers are vital when taking multiple medications.
Increased Risk of Certain Cancers
While some studies have suggested a possible link between statin use and an increased risk of certain cancers, the overall evidence remains inconclusive. It is crucial to emphasize that more research is needed to definitively establish any causal relationship. Consult your doctor for a comprehensive discussion about the potential risks and benefits of statin use in relation to your personal medical history and risk factors.
Further investigation is needed to definitively understand the relationship between statins and cancer risk.
Categorization of Less Common Side Effects
| Body System | Side Effect | Potential Severity |
|---|---|---|
| Neurological | Peripheral neuropathy (numbness, tingling, pain in extremities) | Mild to severe; often reversible with discontinuation |
| Endocrine | Increased risk of type 2 diabetes | Potentially serious, especially in those with risk factors; manageable with lifestyle changes and monitoring |
| Gastrointestinal | Muscle pain (myalgia) | Mild to moderate; often manageable with dosage adjustments or alternative medications |
| Hepatic | Liver damage (rare) | Serious; requires careful monitoring and potential discontinuation |
| Musculoskeletal | Muscle pain (myopathy), muscle weakness | Mild to severe; often manageable with dosage adjustments or alternative medications |
Factors Influencing Side Effect Occurrence

Statins, while remarkably effective in lowering cholesterol, aren’t without potential side effects. Understanding the factors that influence their occurrence is crucial for both patients and healthcare providers. This knowledge empowers informed decision-making and allows for proactive management of potential issues.Individual patient characteristics play a significant role in how a person responds to statin therapy. Genetics, pre-existing conditions, and age all contribute to variability in side effect susceptibility.
Dosage and duration of use also impact the likelihood of experiencing adverse reactions. Finally, concomitant medications, including those prescribed for other conditions, can influence the outcome of statin treatment. This comprehensive understanding enables healthcare professionals to tailor treatment plans to minimize potential risks and maximize benefits for each individual.
Individual Patient Factors
Various individual characteristics influence a patient’s response to statins. Age, pre-existing liver conditions, and genetic predispositions can all play a role. Older individuals may be more susceptible to certain side effects due to physiological changes. Pre-existing liver disease can increase the risk of liver damage, a rare but serious side effect of statins. Genetic variations in the way the body metabolizes statins can also affect the likelihood and severity of side effects.
Dosage and Duration of Use
The dosage and duration of statin therapy directly impact the potential for side effects. Higher dosages generally increase the risk of adverse reactions. Similarly, longer-term use, while crucial for long-term cholesterol management, can potentially elevate the risk of side effects over time. For example, a patient on a high dose of atorvastatin for five years might be more likely to experience muscle pain than someone on a lower dose for a shorter period.
Carefully considering the optimal dosage and duration based on individual needs and risk factors is vital.
Concomitant Medications
Many medications can interact with statins, altering their effectiveness or increasing the risk of side effects. This interaction can range from minor inconveniences to serious health concerns. For instance, certain medications that inhibit the body’s ability to break down statins could lead to elevated levels of the medication in the blood, resulting in more severe side effects. A careful review of all medications a patient is taking is crucial to identify and mitigate potential drug interactions.
Drug Interactions
Drug interactions with statins are a complex issue, as various medications can impact statin metabolism and efficacy. Interactions can lead to a variety of outcomes, including increased statin levels in the blood, altered drug absorption, and changes in the way the body processes other medications. Understanding these interactions requires a detailed review of all medications a patient is currently taking, both prescription and over-the-counter.
For instance, grapefruit juice can significantly increase the blood levels of some statins, leading to a higher risk of side effects.
Patient Factors Influencing Statin Side Effect Susceptibility
| Factor | Potential Impact |
|---|---|
| Age | Older adults may be more susceptible to muscle pain and liver damage. |
| Pre-existing liver conditions | Increased risk of liver damage. |
| Genetic variations | Variability in metabolism of statins, impacting side effect likelihood. |
| Dosage | Higher dosages generally increase the risk of side effects. |
| Duration of use | Longer-term use may increase the risk of some side effects over time. |
| Concomitant medications | Interactions with other medications can increase or decrease statin effectiveness and increase side effects. |
Management and Mitigation of Side Effects
Statins, while effective in lowering cholesterol, can unfortunately cause a range of side effects in some individuals. Understanding how to manage these side effects is crucial for maximizing the benefits of statin therapy while minimizing discomfort. This section details strategies for mitigating mild side effects, highlights when professional consultation is necessary, and explores alternative approaches.Managing statin-related side effects often involves a combination of lifestyle adjustments, medical interventions, and careful monitoring.
Statins, while often prescribed for cholesterol management, can sometimes have unwanted side effects. Understanding these potential issues is crucial for informed healthcare decisions. One important concept to consider is the potential for some side effects to be linked to cytotoxic effects, which means they can damage or kill cells. For a deeper dive into what “cytotoxic” means and examples of things that fit that definition, check out this helpful resource: cytotoxic definition and examples.
Ultimately, it’s important to discuss any concerns about statin side effects with your doctor.
Mild discomfort can frequently be alleviated through proactive measures, while more severe or persistent symptoms necessitate prompt medical attention.
Strategies for Managing Mild Side Effects
Mild side effects, such as muscle aches or digestive issues, can often be addressed through lifestyle modifications and dietary changes. These strategies aim to lessen the impact of statins without completely eliminating the medication.
- Dietary Adjustments: A balanced diet rich in fruits, vegetables, and whole grains can support overall health and potentially lessen some side effects. Limiting processed foods, saturated fats, and excessive alcohol intake can also be beneficial.
- Lifestyle Modifications: Regular exercise, stress reduction techniques, and adequate sleep can contribute to overall well-being and may help alleviate some mild side effects. Maintaining a healthy weight can also play a role in managing side effects.
- Gradual Dosing: In some cases, a gradual increase in the dosage of the statin can help the body adjust and reduce the intensity of side effects. This should only be done under the strict supervision of a healthcare professional.
When to Consult a Healthcare Professional
Prompt medical attention is essential for any side effects that are severe, persistent, or worsen over time. This includes muscle pain that interferes with daily activities, unexplained fatigue, or digestive problems that cause significant discomfort. Changes in liver function or kidney function, even if mild, should be evaluated by a physician.
- Persistent Muscle Pain: Muscle pain that doesn’t improve with rest or over-the-counter pain relievers should be evaluated by a healthcare professional. This is particularly important if the pain is severe or accompanied by other symptoms.
- Significant Digestive Issues: Persistent or severe digestive problems, such as nausea, vomiting, or diarrhea, warrant a consultation with a doctor. These symptoms can sometimes indicate more serious underlying issues.
- Signs of Liver or Kidney Issues: Any signs of liver or kidney problems, including jaundice, dark urine, or persistent fatigue, should prompt immediate medical attention. Blood tests can assess the status of these organs.
Alternative Therapies
While alternative therapies may show promise for some individuals, it’s crucial to consult with a healthcare professional before trying them. Some individuals may find relief through supplements or natural remedies, but these should never replace or substitute prescribed medications without a doctor’s approval.
- Supplements: Some individuals use supplements like coenzyme Q10 (CoQ10) in an attempt to lessen statin-related muscle pain. However, these should not be taken without first discussing it with a physician.
Recommendations for Minimizing Statin-Related Side Effects
Following these recommendations can significantly improve the experience of taking statins.
- Regular Check-ups: Regular check-ups with your physician are essential to monitor your health and identify any potential side effects early. Blood tests, including liver and kidney function tests, can help assess your overall health.
- Open Communication: Maintain open and honest communication with your healthcare provider about any side effects you experience. This allows for personalized strategies to manage the symptoms.
- Patient Education: Educating yourself about statins, including potential side effects, helps you actively participate in your healthcare decisions.
Flow Chart for Managing Suspected Side Effects
The following flow chart provides a step-by-step approach to managing suspected statin-related side effects:
| Step | Action |
|---|---|
| 1 | Identify and document the symptom. |
| 2 | Assess symptom severity. Is it mild, moderate, or severe? |
| 3 | Consult with your healthcare professional. |
| 4 | Follow their advice and recommendations. |
| 5 | Monitor the symptoms closely. |
Specific Side Effects and Their Descriptions
Statins, while crucial for cardiovascular health, can sometimes lead to unwanted side effects. Understanding the specific nature of these reactions is vital for both patients and healthcare providers. This section delves into the details of common side effects, exploring their potential severity, underlying causes, and management strategies.
Muscle Pain (Myalgia)
Muscle pain, or myalgia, is a frequently reported side effect of statin therapy. The pain can range from mild discomfort to severe debilitating conditions. The severity varies significantly between individuals.
Myalgia, often described as muscle aches, pains, or tenderness, can be a symptom of statin-induced muscle damage, a condition known as myopathy. The severity can range from mild discomfort to severe muscle weakness and pain, potentially leading to rhabdomyolysis, a life-threatening condition. In most cases, myalgia is mild and temporary, resolving with dosage adjustment or discontinuation of the medication. However, it’s crucial to consult a healthcare professional if the pain is severe or persistent.
The potential for myalgia is influenced by factors such as dosage, individual metabolism, and concomitant medications. Certain genetic predispositions may also increase the risk. Individuals experiencing persistent or severe muscle pain should seek immediate medical attention to rule out more serious conditions and ensure proper management.
Liver Enzyme Abnormalities
Statins can occasionally impact liver function. Monitoring liver enzyme levels is crucial during statin therapy to detect any abnormalities promptly.
Statins can cause an elevation in liver enzymes, which are proteins produced by the liver. While usually mild and temporary, in some cases, these elevations can signal more serious liver damage. Regular monitoring of liver function tests (LFTs) helps detect any such issues early. Treatment options vary depending on the severity and cause of the elevation. In many cases, a dosage adjustment or discontinuation of the statin may be necessary.
The majority of liver enzyme abnormalities associated with statins are mild and do not require significant intervention. However, close monitoring is essential, especially in patients with pre-existing liver conditions or those taking other medications that may affect liver function.
Gastrointestinal Side Effects
Gastrointestinal side effects are another possible concern associated with statin use.
Gastrointestinal issues can include nausea, vomiting, diarrhea, constipation, or abdominal pain. These effects, while often mild, can be disruptive. The exact mechanisms behind these symptoms are not fully understood, but they are often related to the medication’s effect on the digestive system. In most cases, these symptoms are temporary and resolve with continued treatment or a change in dosage. If symptoms persist or worsen, medical advice should be sought.
Statins, while often prescribed for heart health, can sometimes come with unexpected side effects. It’s important to discuss these potential issues with your doctor, especially if you’re experiencing anything unusual. Knowing how to navigate a visit to the gynecologist can also be helpful for managing overall health, especially if you’re taking medication. For a helpful guide on going to the gynecologist 101, check out this informative article going to the gynecologist 101.
Ultimately, open communication with your healthcare providers is key to understanding and managing any potential side effects, including those from statins.
The frequency and severity of gastrointestinal side effects vary among individuals. Patients who experience these symptoms should consult their doctor for advice on potential management strategies, including dosage adjustments or alternative medications.
Skin Reactions, Side effects of statins
Skin reactions, while less common, can occur in some patients taking statins.
Skin reactions to statins can manifest as rashes, itching, or other forms of skin irritation. In rare instances, more severe reactions, such as Stevens-Johnson syndrome or toxic epidermal necrolysis, can occur. These conditions require immediate medical attention. The precise mechanisms behind skin reactions to statins are not completely understood. If any skin rash or unusual skin reaction develops, patients should immediately contact their doctor.
Individual susceptibility to skin reactions varies, and a thorough medical history is critical to identify potential risk factors. Prompt diagnosis and appropriate treatment are vital to ensure the well-being of patients experiencing skin reactions.
Illustrative Cases: Side Effects Of Statins
Statins, while highly effective in reducing cholesterol, can unfortunately cause a range of side effects. Understanding these side effects and how they manifest in different patients is crucial for effective management. The following case studies highlight various side effects and the approaches healthcare professionals might take to address them.
Muscle Pain (Myopathy)
Muscle pain, a common side effect of statins, can range from mild discomfort to severe muscle damage. Prompt diagnosis and appropriate management are essential.
Case Study 1: A 65-year-old male patient presented with increasing muscle pain and weakness after starting a statin for hyperlipidemia. The pain was localized to his thighs and shoulders, and was aggravated by movement. Initial blood tests revealed elevated creatine kinase (CK) levels, an indicator of muscle damage. The statin was immediately discontinued, and the patient was started on alternative lipid-lowering therapies.
Physical therapy and pain management strategies were also implemented. After a few weeks, the patient’s muscle pain significantly subsided, and his CK levels returned to normal. This case emphasizes the importance of monitoring CK levels and promptly adjusting or discontinuing statin therapy if myopathy develops.
Liver Enzyme Abnormalities
Some individuals may experience elevated liver enzyme levels while taking statins. This typically manifests as mild elevations in liver function tests (LFTs). Regular monitoring and appropriate adjustments to therapy are crucial.
Case Study 2: A 52-year-old female patient, taking a statin for cholesterol control, showed mildly elevated liver enzyme levels during a routine check-up. The physician closely monitored the patient’s LFTs and reduced the statin dosage. Further testing confirmed the liver enzyme levels normalized within a few weeks. This case illustrates the importance of routine LFT monitoring and the potential for dosage adjustments in managing elevated liver enzymes related to statin use.
Gastrointestinal Issues
Gastrointestinal side effects, such as nausea, diarrhea, and abdominal pain, are also possible with statin use. These side effects are often mild and transient.
Case Study 3: A 48-year-old patient reported mild nausea and occasional bouts of diarrhea after initiating a statin. The physician advised the patient to take the medication with food, which significantly reduced the gastrointestinal discomfort. The patient continued to report mild symptoms, but they did not significantly impact their quality of life. This case highlights the potential for gastrointestinal side effects and the importance of lifestyle adjustments (like taking with food) in mitigating them.
Drug Interactions
Statins can interact with other medications, potentially increasing the risk of side effects or decreasing the effectiveness of the medication. Carefully reviewing all medications taken by a patient is critical.
Case Study 4: A patient taking a statin was also prescribed a medication for high blood pressure. The patient’s doctor noted that the blood pressure medication and the statin could potentially interact. The physician adjusted the dosage of the blood pressure medication to minimize any interaction and monitored the patient for any unusual side effects. This case exemplifies the importance of thorough medication history and a proactive approach to managing potential drug interactions.
Summary of Case Studies
| Case Study | Patient Profile | Symptoms | Treatment |
|---|---|---|---|
| 1 | 65-year-old male with muscle pain and weakness | Muscle pain, weakness, elevated CK levels | Statin discontinued, alternative therapy initiated, physical therapy |
| 2 | 52-year-old female with elevated liver enzymes | Elevated liver enzymes (LFTs) | Statin dosage reduced, LFTs monitored |
| 3 | 48-year-old with gastrointestinal symptoms | Nausea, diarrhea | Medication taken with food |
| 4 | Patient on statin and blood pressure medication | Potential drug interaction | Blood pressure medication dosage adjusted, monitoring for side effects |
Ultimate Conclusion
In conclusion, while statins are valuable for managing cholesterol, it’s essential to be aware of the potential side effects. Understanding the diverse range of possible reactions, from common muscle pain to rare but serious complications, empowers individuals to discuss concerns with their healthcare providers. This guide provides a comprehensive overview, but consulting a doctor remains crucial for personalized advice and tailored management strategies.
Remember, proactive communication and informed decision-making are key to navigating statin therapy effectively.