Rheumatoid arthritis in the neck can significantly impact your quality of life, causing pain, stiffness, and reduced mobility. Understanding the specific ways RA affects the cervical spine, along with its symptoms and treatment options, is crucial for effective management. This guide delves into the complexities of rheumatoid arthritis in the neck, providing a comprehensive overview for anyone affected by or interested in learning more about this condition.
This detailed exploration will cover the spectrum of RA in the neck, from its initial symptoms to potential long-term complications. We’ll examine the interplay between RA and the cervical spine, discuss diagnostic methods, and explore the range of treatment options available. We’ll also highlight the importance of lifestyle adjustments and support systems in managing RA in the neck.
Rheumatoid Arthritis in the Neck: Understanding the Impact
Rheumatoid arthritis (RA) is a chronic autoimmune disease that affects the body’s immune system, causing it to mistakenly attack healthy tissues and joints. This inflammation can lead to pain, stiffness, and swelling, potentially impacting various bodily functions and overall well-being. The progression of RA can vary significantly from person to person, but it generally involves a gradual worsening of symptoms over time if left untreated.Rheumatoid arthritis can affect the cervical spine, the part of the spine in the neck region.
This can result in a range of issues, from mild discomfort to significant structural changes that can impact the alignment and mobility of the neck. The inflammatory process associated with RA can cause erosion and damage to the cartilage and bones of the cervical spine, leading to pain, stiffness, and potential complications like nerve impingement. This damage can also lead to instability in the neck.
Common Symptoms of RA in the Neck
Common symptoms of rheumatoid arthritis in the neck include pain, stiffness, and limited range of motion. These symptoms are often more pronounced in the morning or after periods of inactivity. Pain can radiate to other parts of the body, and individuals may experience other symptoms, like fever or fatigue.
Dealing with rheumatoid arthritis in the neck can be tough, and managing weight is often a part of the journey. Finding the right balance of nutrients, like protein, is key. For example, understanding how much protein should I eat to lose weight can significantly impact your overall health and well-being, especially if you have RA in the neck.
Proper nutrition is vital for supporting your body as you manage the inflammation and stiffness associated with rheumatoid arthritis in the neck. how much protein should i eat to lose weight This can help you feel better and reduce the impact of the condition on your daily life.
| Symptom | Description | Frequency | Severity |
|---|---|---|---|
| Pain | Aching or throbbing sensation in the neck, potentially radiating to the shoulders, head, or arms. May be worse in the morning or after periods of rest. | Frequent, often daily. | Variable, ranging from mild discomfort to severe debilitating pain. |
| Stiffness | Limited ability to move the neck through its full range of motion. This stiffness may be especially noticeable in the morning or after periods of inactivity. | Frequent, especially in the morning. | Variable, ranging from slight limitation to significant restriction of movement. |
| Limited Range of Motion | Difficulty turning, bending, or tilting the head. This can impact activities like looking over your shoulder or reaching for something above your head. | Variable, can worsen over time. | Variable, ranging from mild restriction to complete loss of motion in extreme cases. |
| Inflammation | Swelling and tenderness in the neck, potentially visible or palpable. | Variable, not always present. | Variable, may be mild or severe, depending on the individual’s response to the disease. |
| Tenderness | Pain upon touch or pressure in the neck area. | Frequent, especially in areas of inflammation. | Variable, from slight discomfort to intense pain. |
Symptoms and Diagnosis
Rheumatoid arthritis (RA) in the neck, while less common than RA in other joints, can significantly impact quality of life. Understanding the specific symptoms and diagnostic methods is crucial for early intervention and effective management. This knowledge empowers individuals to seek appropriate medical care and potentially alleviate suffering.Recognizing the signs and symptoms of RA in the neck is vital for prompt diagnosis.
Early detection allows for earlier intervention, potentially minimizing long-term damage and improving overall outcomes. Accurate diagnosis relies on a combination of clinical assessments and diagnostic tests.
Key Symptoms of RA in the Neck
The symptoms of RA in the neck can vary in severity and presentation. Common symptoms include persistent pain, stiffness, and reduced range of motion. Pain often worsens in the morning or after periods of inactivity. Stiffness can limit the ability to turn, bend, or move the neck freely. The affected area may also feel warm to the touch.
These symptoms, while often indicative of RA, can also be associated with other neck pain conditions. Careful consideration of the patient’s medical history and other presenting symptoms is crucial in reaching an accurate diagnosis.
Methods for Diagnosing RA in the Neck
Diagnosing RA in the neck involves a multi-faceted approach. A thorough physical examination by a healthcare professional is essential. This examination includes assessing the range of motion, palpating the affected areas for tenderness and inflammation, and evaluating the overall musculoskeletal system. Imaging tests, such as X-rays and MRIs, can help visualize the structures of the neck, potentially revealing joint damage or inflammation.
Rheumatoid arthritis in the neck can be debilitating, affecting daily life significantly. While managing the pain and stiffness is crucial, exploring all treatment options is important. For example, considering the various pros and cons of IUDs pros and cons of iud might be beneficial for some, but this isn’t directly related to neck arthritis. Ultimately, the best approach to rheumatoid arthritis in the neck depends on individual needs and circumstances.
Blood tests, particularly those measuring specific inflammatory markers, can provide valuable information about the presence and activity of RA. These tests, alongside the clinical evaluation, assist in differentiating RA from other possible causes of neck pain.
Differentiating RA from Other Neck Pain Conditions
Accurate diagnosis involves distinguishing RA from other possible causes of neck pain. Conditions like osteoarthritis, whiplash injuries, or infections can present with similar symptoms. A comprehensive medical history, a detailed physical examination, and appropriate diagnostic tests are essential to rule out other potential causes and arrive at a definitive diagnosis.
Diagnostic Table
| Symptom | Possible Cause (RA) | Possible Cause (Other) | Diagnostic Test |
|---|---|---|---|
| Persistent neck pain, especially in the morning | Inflammation of the joints in the neck | Muscle strain, osteoarthritis, or other musculoskeletal issues | Physical exam, blood tests (ESR, CRP), X-ray, MRI |
| Stiffness and limited range of motion in the neck | Inflammation and damage to the joint tissues | Muscle spasms, whiplash, or other soft tissue injuries | Physical exam, X-ray, MRI, blood tests |
| Swelling and warmth around the affected joints | Inflammation related to RA | Local infections, injuries, or other inflammatory conditions | Physical exam, blood tests (ESR, CRP), MRI, X-ray |
Impact on Cervical Spine: Rheumatoid Arthritis In The Neck
Rheumatoid arthritis (RA) doesn’t just affect the joints; it can significantly impact the entire cervical spine, the portion of the spine in the neck. This impact manifests in various ways, leading to structural changes, pain, and potential functional limitations. Understanding these effects is crucial for effective management and improving quality of life for those with RA.The cervical spine, crucial for neck movement and head support, is particularly vulnerable to the destructive processes of RA.
Inflammation, a hallmark of RA, causes the immune system to attack the lining of joints, leading to cartilage erosion and bone destruction. This progressive damage, if left unchecked, can result in instability and deformities that restrict movement and cause pain.
Cervical Spine Structural Damage
The inflammatory process in RA targets the cartilage and bone within the cervical spine joints. Cartilage, the smooth tissue cushioning the bones, is progressively damaged, leading to bone-on-bone contact. This friction can cause significant pain and stiffness. Bone erosion, the gradual wearing away of bone tissue, can further weaken the structure of the spine, making it more susceptible to fractures.
These processes are particularly pronounced in individuals with more severe or longer-standing RA.
Cervical Instability and Deformity
The erosion and inflammation can lead to instability in the cervical spine. The weakened ligaments and joints lose their ability to maintain proper alignment, increasing the risk of dislocations or subluxations (partial dislocations). These instabilities can manifest as pain, numbness, or tingling in the arms and hands, and can severely limit movement. Over time, this instability can lead to significant deformities in the cervical spine, impacting posture and function.
Examples include forward head posture and fusion of vertebrae.
Role of Inflammation in Pain and Stiffness
Inflammation plays a critical role in the pain and stiffness associated with RA in the neck. The inflammatory response releases chemicals that cause swelling, irritation, and pain in the surrounding tissues. This inflammation also leads to stiffness and reduced range of motion as the joints become inflamed and swollen. Chronic inflammation in the cervical spine can cause persistent pain, even when the individual is at rest.
Impact on Cervical Spine: A Table
| Affected Structure | Description of Damage | Symptoms | Imaging Findings |
|---|---|---|---|
| Cartilage | Progressive thinning and destruction, leading to bone-on-bone contact. | Pain, stiffness, limited range of motion, grinding or popping sensations. | Narrowing of joint spaces, loss of cartilage thickness on X-rays, MRI showing inflammation. |
| Bone | Erosion and thinning of bone tissue. | Pain, tenderness, and possible increased susceptibility to fractures. | Loss of bone density, visible bone erosions on X-rays, possible bony spurs on X-rays, MRI showing inflammation. |
| Ligaments | Weakening and laxity, leading to instability. | Pain, clicking or popping sounds in the neck, numbness or tingling in the arms or hands. | Loss of normal alignment on X-rays, instability demonstrated on stress views. |
| Soft Tissues | Inflammation and swelling of muscles, tendons, and ligaments. | Pain, stiffness, tenderness, limited range of motion. | Soft tissue swelling and inflammation visible on MRI. |
Treatment Approaches
Managing rheumatoid arthritis (RA) in the neck requires a multifaceted approach tailored to individual needs. Effective treatment aims to reduce inflammation, alleviate pain, preserve cervical spine function, and prevent further damage. A combination of medications, physical therapy, and potentially surgery plays a crucial role in achieving these goals.Treatment strategies for RA in the neck are not simply about alleviating symptoms; they are designed to address the underlying cause of the condition.
This includes suppressing the immune system’s attack on the joints and minimizing the inflammatory response. Different approaches offer varying degrees of effectiveness and potential side effects, necessitating careful consideration and collaboration between patients and healthcare providers.
Medication Strategies
Various medications are used to manage RA in the neck, each with its own mechanism of action, efficacy, and potential side effects. Nonsteroidal anti-inflammatory drugs (NSAIDs) are often the first line of defense against pain and inflammation. However, their effectiveness in controlling the underlying disease process is limited. Disease-modifying antirheumatic drugs (DMARDs) are more potent and can significantly slow the progression of RA, reducing the risk of long-term complications.
Rheumatoid arthritis in the neck can be tricky, impacting not only the neck’s mobility but also potentially affecting other areas. Sometimes, the symptoms overlap with other conditions, like difficulties with processing sounds, which can manifest as an auditory processing disorder in adults. Auditory processing disorder in adults might be mistaken for stiffness or pain in the neck.
However, understanding these potential connections is key to accurate diagnosis and targeted treatment for rheumatoid arthritis in the neck.
- NSAIDs: These drugs, such as ibuprofen and naproxen, provide temporary relief from pain and inflammation. They work by inhibiting cyclooxygenase enzymes, which are involved in the production of prostaglandins. However, long-term use can lead to gastrointestinal issues, including ulcers and bleeding.
- DMARDs: These drugs, such as methotrexate, sulfasalazine, and hydroxychloroquine, are crucial for modifying the course of RA. They work by targeting various aspects of the immune response, aiming to slow or stop joint damage. DMARDs often require regular monitoring due to potential side effects, which can vary depending on the specific drug and individual patient response. Examples include liver damage (methotrexate), blood disorders (sulfasalazine), and visual problems (hydroxychloroquine).
These medications usually take several weeks or months to demonstrate their full effect.
Physical Therapy
Physical therapy plays a vital role in maintaining and improving cervical spine mobility and function. Exercises and stretches can help strengthen supporting muscles, improve range of motion, and reduce pain. Physical therapists also educate patients on proper posture and body mechanics to prevent further injury.
- Exercises: Specific exercises tailored to the needs of each patient can improve strength, flexibility, and range of motion. These exercises often focus on strengthening the neck and shoulder muscles, which provide stability and support.
- Manual Therapy: Techniques such as massage, mobilization, and manipulation can help alleviate pain, improve joint mobility, and restore function. This can include gentle adjustments to the neck and surrounding areas.
- Education: Physical therapists provide education on proper posture, body mechanics, and exercises to prevent further injury and maintain long-term health.
Surgical Interventions
In severe cases where other treatments have failed to adequately control symptoms or prevent further damage, surgical intervention might be considered. Surgical options aim to stabilize the cervical spine, reduce pain, and improve functionality. Examples include fusion procedures, which involve joining two or more vertebrae to prevent movement and stabilize the spine.
- Cervical Fusion: This surgical technique involves joining two or more vertebrae to stabilize the spine. It can effectively address instability and pain, but it permanently restricts movement in the affected segment.
Multidisciplinary Approach
A multidisciplinary approach is essential for optimal management of RA in the neck. This involves collaboration among rheumatologists, physical therapists, occupational therapists, and potentially other specialists. This coordinated effort ensures comprehensive care, addressing not only the physical symptoms but also the emotional and social impact of the disease.
| Treatment Type | Mechanism of Action | Potential Benefits | Potential Risks |
|---|---|---|---|
| NSAIDs | Inhibit cyclooxygenase enzymes | Temporary pain and inflammation relief | Gastrointestinal issues, including ulcers and bleeding; limited effect on underlying disease |
| DMARDs | Target various aspects of the immune response | Slow or stop joint damage; modify the course of RA | Potential side effects (e.g., liver damage, blood disorders, visual problems); delayed onset of action |
| Physical Therapy | Strengthening, stretching, and education | Improved mobility, reduced pain, improved function | Requires patient compliance; potential for discomfort during treatment |
| Surgery (Cervical Fusion) | Stabilize the spine | Reduced pain, improved stability | Permanent loss of movement in the affected segment; risk of complications associated with surgery |
Management and Prevention
Managing rheumatoid arthritis (RA) in the neck requires a multifaceted approach that addresses pain, inflammation, and the preservation of cervical spine health. This involves a combination of medical interventions, lifestyle adjustments, and proactive measures to prevent further damage. A personalized strategy, tailored to individual needs and disease progression, is crucial for optimal outcomes.Effective management of RA in the neck goes beyond simply treating symptoms.
It’s about empowering individuals to actively participate in their care and make informed decisions about their health. This includes understanding the impact of RA on the cervical spine, recognizing early warning signs, and adopting strategies to minimize the long-term consequences.
Pain Management Techniques
Effective pain management is essential for maintaining mobility and quality of life. This encompasses a range of approaches, from over-the-counter medications to prescription drugs, physical therapies, and complementary methods. Medication selection should consider individual tolerance, potential side effects, and the severity of pain.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) can provide relief from mild to moderate pain and inflammation. Examples include ibuprofen and naproxen.
- Disease-modifying antirheumatic drugs (DMARDs) are prescribed to slow or stop the progression of RA. They work by suppressing the immune system’s attack on the joints.
- Corticosteroids can be used to reduce inflammation quickly, but their long-term use should be carefully considered due to potential side effects.
- Physical therapy, including heat therapy, cold therapy, and gentle stretching exercises, can help alleviate pain and improve range of motion.
- Complementary therapies, such as acupuncture, massage, and mindfulness practices, can also contribute to pain relief.
Exercise Routines
Regular exercise is crucial for maintaining muscle strength, flexibility, and joint mobility. However, exercises must be tailored to the individual’s capabilities and the specific areas affected by RA. Consult a physical therapist to create a safe and effective exercise program.
- Gentle stretching exercises, such as neck rotations and side bends, can help maintain flexibility and prevent stiffness.
- Strengthening exercises, targeting the neck and shoulder muscles, can improve stability and reduce pain.
- Low-impact aerobic exercises, such as swimming or walking, can help maintain cardiovascular health and overall well-being.
- Avoid activities that put excessive strain on the neck, such as heavy lifting or jarring movements.
Assistive Devices
Assistive devices can significantly improve comfort and independence for individuals with RA in the neck. These tools can help reduce strain on the neck and provide support during daily activities.
- Cervical collars or supports can provide stability and reduce pain during movement.
- Adaptive utensils and clothing can simplify tasks like eating and dressing, reducing strain on the neck.
- Ergonomic chairs and workstations can help maintain proper posture and reduce stress on the neck throughout the day.
- Weighted blankets or pillows can provide support and comfort during sleep.
Preventive Measures
Proactive measures to prevent further damage to the cervical spine include managing inflammation, maintaining good posture, and avoiding activities that exacerbate pain.
- Regular monitoring of RA symptoms and prompt intervention for flares can help slow disease progression.
- Maintaining good posture, whether sitting or standing, is crucial to reduce strain on the neck.
- Avoiding activities that place excessive stress on the neck, such as heavy lifting or forceful movements, can prevent further injury.
- Using assistive devices, like ergonomic tools, can help to reduce the strain on the neck.
Lifestyle Factors
Lifestyle factors, including diet and stress management, play a significant role in managing RA.
- A balanced diet rich in fruits, vegetables, and whole grains can provide essential nutrients for overall health and support immune function.
- Stress management techniques, such as meditation, yoga, and deep breathing exercises, can help reduce inflammation and improve overall well-being.
- Adequate sleep is essential for allowing the body to repair itself and manage pain effectively.
- Maintaining a healthy weight can reduce stress on joints.
RA management requires a comprehensive approach encompassing medication, exercise, assistive devices, and proactive lifestyle adjustments. A balanced diet, stress reduction techniques, and adequate sleep are vital components in managing the condition and preventing further complications.
Living with RA in the Neck
Living with rheumatoid arthritis (RA) in the neck can significantly impact daily life, causing pain, stiffness, and reduced mobility. Understanding the challenges and adapting to them is crucial for maintaining a good quality of life. This section explores the daily realities and available support for individuals facing RA-related neck issues.
Impact on Daily Activities and Quality of Life
RA in the neck can lead to a range of difficulties in performing everyday tasks. Pain and stiffness can make simple movements, like turning your head, reaching for objects, or even getting dressed, challenging and time-consuming. This can affect work productivity, social activities, and overall well-being. The chronic nature of the condition can also contribute to emotional distress and fatigue, further impacting quality of life.
Strategies for Adapting to Challenges
Several strategies can help individuals with RA in the neck manage their symptoms and maintain their independence. These include employing assistive devices like neck supports or ergonomic tools to minimize strain during activities. Regular exercise, tailored to individual needs and limitations, can improve range of motion and overall strength. Proper posture and body mechanics can also help alleviate pain and prevent further damage to the cervical spine.
Learning relaxation techniques, such as deep breathing or meditation, can help manage stress and pain.
Support Resources and Organizations
Numerous support resources and organizations are available to help individuals with RA in the neck navigate their condition. These resources provide valuable information, emotional support, and practical guidance. Local RA support groups offer a forum for connecting with others who understand the challenges and can share coping strategies. Online communities and forums can provide a similar sense of connection and support, regardless of geographic location.
Healthcare professionals, such as rheumatologists, physical therapists, and occupational therapists, play a vital role in providing personalized care and guidance.
Table of Daily Activities, Impact, Adaptive Strategies, and Support Resources
| Daily Activity | Impact of RA | Adaptive Strategies | Support Resources |
|---|---|---|---|
| Turning head | Pain, stiffness, limited range of motion | Using a neck support, gentle stretching exercises, ergonomic positioning | Physical therapist, online RA forums, local RA support groups |
| Reaching for objects | Pain, weakness, difficulty with fine motor skills | Using assistive devices (e.g., long-handled utensils), adjusting workspace layout | Occupational therapist, ergonomic assessments, online RA support groups |
| Getting dressed | Pain, stiffness, difficulty with upper body movements | Wearing looser clothing, using adaptive clothing, seeking assistance when needed | Physical therapist, support groups, home healthcare aids |
| Working | Reduced productivity, fatigue, pain | Adjusting work schedule, modifying tasks, using ergonomic tools, communicating needs to employer | Rheumatologist, employer support programs, employee assistance programs, online RA forums |
| Social Activities | Pain, fatigue, social isolation | Scheduling activities in advance, pacing oneself, communicating limitations to friends and family, utilizing support networks | Support groups, online communities, family and friends |
Potential Complications
Untreated or poorly managed rheumatoid arthritis (RA) in the neck can lead to a range of serious complications, impacting the cervical spine’s structural integrity and function. These complications can significantly diminish quality of life and necessitate careful monitoring and management. Early intervention and adherence to treatment plans are crucial to minimize these risks.RA’s inflammatory processes can erode cartilage and bone in the cervical spine, potentially causing instability and deformity.
This can lead to a variety of issues, from pain and stiffness to more severe complications like spinal cord compression and nerve damage. Understanding these potential problems is vital for proactive management and seeking appropriate medical attention.
Spinal Cord Compression
RA can cause inflammation and erosion of the bones and tissues surrounding the spinal cord in the neck. This narrowing of the spinal canal, known as spinal stenosis, can put pressure on the spinal cord. Symptoms can include numbness, tingling, weakness, or paralysis in the arms and legs, as well as bowel and bladder dysfunction. The severity of these symptoms can vary significantly.
For instance, some individuals might experience mild discomfort, while others might face debilitating paralysis. Early recognition and treatment are essential to prevent permanent neurological damage.
Nerve Damage
The inflammatory process associated with RA can also affect the nerves that branch out from the spinal cord in the neck. This can result in pain, numbness, tingling, and weakness in the arms, hands, and shoulders. The extent of nerve damage depends on the severity of RA and the affected nerves. Some individuals may experience intermittent symptoms, while others might experience persistent discomfort and functional limitations.
Prompt diagnosis and treatment are vital to minimize nerve damage and preserve function.
Reduced Mobility
Progressive inflammation and joint damage caused by RA can restrict movement in the neck. This reduced mobility can impact daily activities, such as eating, dressing, and working. The loss of flexibility can also contribute to chronic pain and discomfort. The level of mobility loss can range from mild stiffness to significant limitation in range of motion. Physical therapy and assistive devices can be beneficial in maintaining mobility and preventing further complications.
Long-Term Implications
The long-term consequences of untreated or inadequately managed RA in the neck can be significant. These can include chronic pain, disability, and decreased quality of life. Individuals with RA in the neck may experience persistent stiffness and pain, impacting their ability to perform routine tasks. Furthermore, the potential for spinal cord compression or nerve damage underscores the importance of early diagnosis and aggressive treatment to mitigate long-term complications.
Potential Complications Table
| Complication | Cause | Symptoms | Prevention Strategies |
|---|---|---|---|
| Spinal Cord Compression | Inflammation and erosion of bone and tissues surrounding the spinal cord | Numbness, tingling, weakness, or paralysis in the arms and legs; bowel and bladder dysfunction | Early diagnosis and treatment; regular monitoring; adherence to prescribed medication and therapies |
| Nerve Damage | Inflammation affecting nerves branching from the spinal cord | Pain, numbness, tingling, and weakness in the arms, hands, and shoulders | Early diagnosis and treatment; regular follow-up appointments; avoidance of activities that exacerbate symptoms |
| Reduced Mobility | Progressive inflammation and joint damage | Stiffness, pain, and limitation in range of motion in the neck | Physical therapy; assistive devices; maintaining a healthy lifestyle; managing RA with prescribed medication |
Illustrations and Visualizations

Understanding rheumatoid arthritis (RA) in the neck requires visualizing the changes it causes in the cervical spine. Visual aids help us grasp the complexities of the disease, from the initial inflammation to the long-term structural alterations. Illustrations and imaging findings offer crucial insights into the impact of RA on the neck, enabling better diagnosis, treatment, and management.The illustrations and visualizations presented here will detail the normal cervical spine, highlight the structural modifications caused by RA, and showcase how imaging techniques like X-rays and MRI reveal these changes.
They will also depict the inflammatory mechanisms at play, demonstrating how the immune system attacks the joints and tissues in the neck. This will aid in understanding the disease’s progression and the rationale behind various treatment strategies.
Healthy Cervical Spine, Rheumatoid arthritis in the neck
The healthy cervical spine is a complex structure composed of seven vertebrae, intervertebral discs, ligaments, and muscles. These components work together to provide stability, flexibility, and support for the head and neck. The vertebrae are stacked atop one another, forming a curved structure that allows for a wide range of motion. The intervertebral discs act as cushions between the vertebrae, absorbing shock and facilitating movement.
Ligaments connect the vertebrae, providing stability and preventing excessive movement. The muscles surrounding the spine provide additional support and control. A healthy cervical spine allows for smooth and controlled head and neck movements.
Structural Changes in the Cervical Spine Due to RA
Rheumatoid arthritis (RA) in the neck leads to a series of structural changes in the cervical spine. The immune system mistakenly attacks the synovial lining of the joints, causing inflammation and erosion of cartilage. This process can lead to joint instability, bone fusion (ankylosis), and the formation of bony spurs (osteophytes). Over time, these changes can result in significant loss of cervical spine mobility and stability.
The cervical curve can become flattened or even reversed. Ligaments and muscles can weaken and atrophy due to disuse or inflammation. The inflammatory response can cause the surrounding soft tissues to swell and become painful.
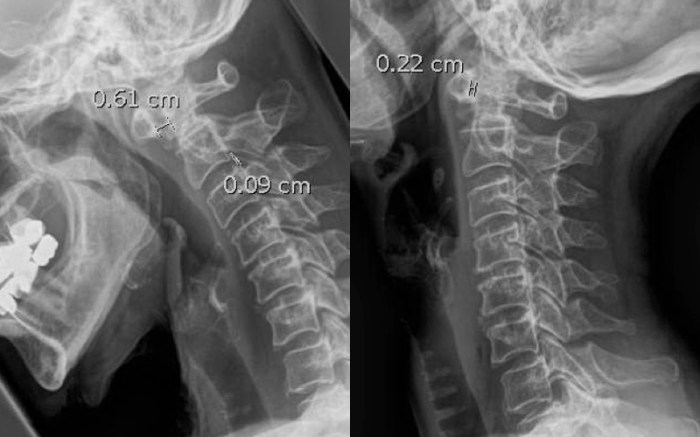
Imaging Findings in Patients with RA in the Neck
Imaging plays a crucial role in diagnosing and monitoring RA in the cervical spine. X-rays and MRI scans are commonly used to assess the extent of the disease.
- X-rays: X-rays primarily reveal the bony structures of the cervical spine. In patients with RA, X-rays often show narrowing of the joint spaces, erosion of bone, and the development of osteophytes (bony spurs). The extent of these changes can vary significantly from patient to patient.
- MRI: Magnetic resonance imaging (MRI) provides detailed information about the soft tissues in the cervical spine, including the ligaments, muscles, and discs. MRI can detect inflammation, swelling, and damage to these structures, which are not always visible on X-rays. This is important because inflammation can be present even before significant bony changes are apparent on X-rays. Furthermore, MRI can differentiate between different types of tissues, making it helpful in identifying subtle signs of RA-related damage.
Illustration of RA-Related Cervical Spine Inflammation
The inflammatory process in RA-related cervical spine disease involves a complex interplay of immune cells and inflammatory mediators.
- Immune Response: The immune system mistakenly targets the synovial lining of the joints. This leads to the recruitment of inflammatory cells, such as neutrophils and macrophages, into the affected area. These cells release inflammatory mediators, such as cytokines (e.g., TNF-α, IL-1β), which cause further damage to the joint structures.
- Synovial Tissue Involvement: The synovial membrane, the lining of the joint capsule, becomes inflamed and thickened. This thickened synovial tissue, known as pannus, can erode cartilage and bone.
- Cartilage Destruction: The inflammatory process leads to the breakdown of cartilage, the protective tissue covering the ends of the bones. This loss of cartilage leads to bone-on-bone contact, causing pain and further joint damage.
- Bone Erosion: The inflammation and pannus can erode the underlying bone. This erosion can lead to instability and deformities in the cervical spine.
Final Conclusion
In conclusion, rheumatoid arthritis in the neck presents a multifaceted challenge requiring a multifaceted approach to treatment and management. By understanding the condition’s impact on the cervical spine, recognizing the symptoms, and exploring available treatments, you can better navigate the complexities of RA in the neck. Early diagnosis and a proactive approach to treatment, alongside supportive care, are key to managing this condition and maintaining a high quality of life.

