Self collection hpv tests – Self-collection HPV tests offer a new approach to cervical cancer screening. This guide dives deep into the specifics of self-collection HPV tests, examining everything from the available kits and collection methods to the accuracy, accessibility, and ethical considerations surrounding this evolving healthcare practice. Understanding the benefits and potential drawbacks of this method is crucial for anyone considering it.
From the various types of HPV self-collection kits to the step-by-step procedures, this guide provides a thorough overview. We will also explore the potential accuracy differences compared to traditional methods, along with the cost-effectiveness and accessibility of self-collection tests. This information empowers individuals to make informed decisions about their health.
Introduction to Self-Collection HPV Tests
Self-collection kits for human papillomavirus (HPV) testing are rapidly gaining popularity as a way to make screening more accessible and convenient. These kits allow individuals to collect samples from the comfort of their own homes, eliminating the need for a clinic visit and potentially reducing anxiety associated with traditional doctor’s office procedures. This approach can significantly improve adherence to recommended screening guidelines, particularly for individuals who might face barriers to attending scheduled appointments.Self-collection kits offer a streamlined alternative to traditional methods, and their growing prevalence underscores a shift towards empowering individuals in their health management.
Self-collection HPV tests are becoming increasingly popular, offering a convenient way to manage your health. While these tests are useful for early detection, it’s important to remember that some health conditions, like psoriatic arthritis, require a different approach. For example, understanding what medications treat psoriatic arthritis what medications treat psoriatic arthritis is crucial for effective treatment.
Ultimately, self-collection HPV tests empower individuals to take proactive steps in their health journey.
By understanding the various types of kits and their respective advantages, individuals can make informed decisions about their screening needs.
Types of HPV Self-Collection Kits
The availability of self-collection kits has expanded significantly, offering various methods to collect the necessary samples. Different kits cater to specific needs and preferences, reflecting the diverse nature of patient populations.
- Swab-based kits: These kits typically utilize a specialized swab to collect cells from the cervix or vagina. The swab is then placed into a collection vial and sent to a laboratory for analysis. This method is relatively simple and often preferred for its ease of use and straightforward process.
- Liquid-based kits: These kits use a special liquid solution to preserve the collected cells, maximizing the viability and quality of the sample for testing. This method often involves a small device or applicator for collecting cells. The liquid-based method is generally considered more efficient in preserving the cells for comprehensive analysis.
- Other emerging methods: Innovative approaches are continuously being developed. These include non-invasive techniques utilizing specialized devices or applications for sample collection, aiming for improved accuracy and comfort.
Methods of Self-Collection
Understanding the specific method used for self-collection is crucial for accurate and reliable results. Different kits employ varying techniques, and following the instructions meticulously is paramount.
- Cervical swabs: These swabs are typically designed for collecting cells from the cervix, the lower part of the uterus. Proper technique ensures adequate sample collection without causing discomfort. Instructions will usually detail the necessary steps and precautions to avoid contamination.
- Vaginal swabs: These swabs collect cells from the vaginal area. Instructions will guide users through the process, emphasizing the importance of following the steps precisely to avoid mishaps and ensure proper sample collection.
- Liquid-based collection: The process for liquid-based collection often involves a small applicator or device to collect the sample. Following the kit instructions and ensuring correct handling of the collection device is crucial for successful sample preservation.
Benefits of Self-Collection
Self-collection kits offer a variety of advantages over traditional methods. These benefits address the practical needs and preferences of individuals seeking more autonomy in their healthcare.
- Increased Accessibility: Self-collection kits expand access to HPV testing, particularly for individuals in remote areas or those with scheduling difficulties. The ability to collect samples at home reduces barriers to screening, potentially leading to earlier diagnoses.
- Enhanced Privacy and Convenience: Self-collection kits provide a higher degree of privacy, as individuals can collect the sample in the comfort of their own homes. This also translates to increased convenience, avoiding the need for a clinic visit, and reducing the overall time commitment.
- Lower Costs: Self-collection kits often have a lower price point than traditional physician-administered tests. This accessibility can make HPV screening more affordable for many people, improving their overall health management.
Comparison of Self-Collection and Traditional HPV Testing
| Feature | Self-Collection | Traditional Method |
|---|---|---|
| Accessibility | High | Low |
| Cost | Low | High |
| Privacy | High | Moderate |
| Convenience | High | Low |
| Accuracy | Potentially similar to traditional methods, but accuracy depends on proper technique and following instructions. Studies have shown comparable accuracy, but adherence to protocols is key. | Accuracy is generally high when performed by trained professionals. |
Procedure and Supplies for Self-Collection
Taking control of your health by performing a self-collection HPV test empowers you to proactively manage your well-being. Understanding the procedure and necessary materials ensures a smooth and accurate collection process. This section provides a comprehensive guide for performing a self-collection HPV test.
Materials Needed for Self-Collection
The essential materials for a self-collection HPV test are carefully designed to ensure the integrity and accuracy of the sample. These include specific swabs, collection vials, and accompanying instructions. Proper handling of these materials is crucial for the success of the test.
- Collection Kit: This kit typically contains pre-packaged components designed for the specific HPV test method. The kit usually includes detailed instructions, which you should carefully review before starting the process.
- Swabs: Sterile swabs are essential for collecting the sample. They are designed for optimal cell collection and are usually provided in the collection kit.
- Collection Vials: The vials are specifically designed to hold the collected sample and maintain its integrity. They are also part of the collection kit.
- Instructions: Detailed instructions, either printed or digitally available within the kit, Artikel the specific steps for performing the self-collection procedure. Carefully following these instructions is vital for a successful and accurate result.
Step-by-Step Procedure for Self-Collection
The following table Artikels the steps involved in performing a self-collection HPV test. Adhering to these steps will ensure the integrity and accuracy of the sample.
Self-collection HPV tests are becoming increasingly convenient, but what about other health habits? For example, are you wondering about the daily intake of apple cider vinegar? Finding the right amount for your needs can be tricky, and resources like how much apple cider vinegar a day can help. Ultimately, though, prioritizing your health through self-collection HPV testing is still key for early detection.
| Step | Description |
|---|---|
| 1 | Carefully prepare the collection kit by reviewing the included instructions. This includes understanding the specific steps involved, any precautions to take, and the proper handling of the materials. |
| 2 | Clean the area around the sample site with the provided cleansing solution or according to the kit’s instructions. This step ensures a clean and sterile environment for sample collection. |
| 3 | Follow the kit’s instructions meticulously for collecting the sample using the provided swabs. This might involve specific motions or durations for optimal sample collection. |
| 4 | Properly package and return the sample to the designated laboratory, adhering to the provided instructions for packaging and shipping. This ensures the sample reaches the lab in optimal condition. |
Potential Challenges During Self-Collection
While self-collection HPV tests are generally straightforward, some individuals may encounter certain challenges. These include discomfort, difficulty in following the instructions, or concerns about the procedure itself.
- Discomfort: Some individuals may experience mild discomfort during the swabbing process. Taking deep breaths and relaxing can help manage this discomfort. Applying a cold compress after the procedure can also provide relief.
- Difficulty following instructions: Misunderstanding the instructions or experiencing difficulty with the procedure can lead to an inaccurate sample. Carefully reviewing the instructions and seeking clarification from a healthcare professional if needed can resolve this issue.
- Concerns about the procedure: Some individuals may have concerns about the procedure itself. Talking to a healthcare professional or a trusted friend or family member can ease anxieties and provide support.
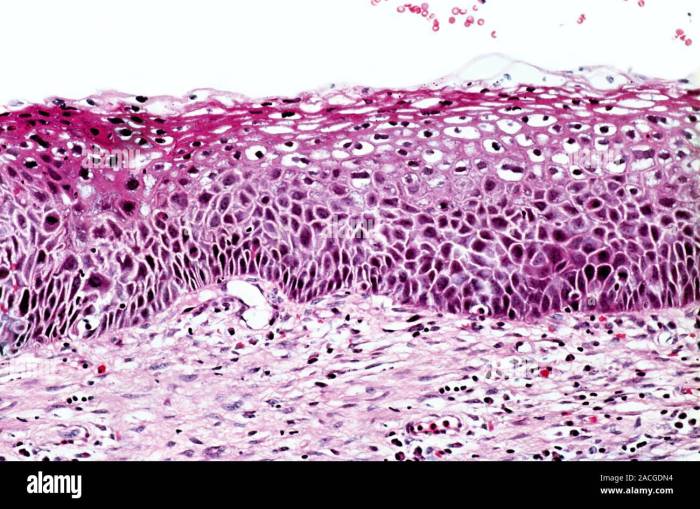
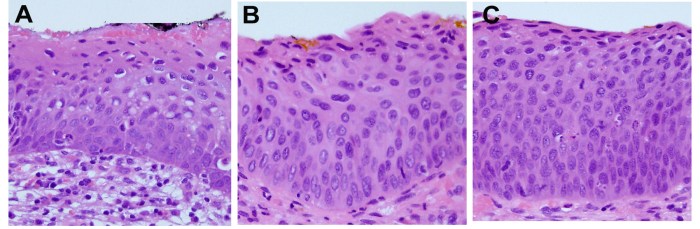
Accuracy and Reliability of Self-Collection Tests
Self-collecting HPV tests offer a convenient and accessible way to screen for the virus. However, understanding the accuracy and potential limitations of these at-home tests is crucial for informed decision-making. This section delves into the factors affecting the reliability of self-collected HPV samples, comparing them to professionally collected ones.The accuracy of self-collected HPV tests is generally comparable to professionally collected samples, but not identical.
While both methods aim to achieve the same goal, variations in technique and sample handling can impact the results. Understanding these nuances is vital for interpreting the outcome correctly.
Comparison to Professional Collections
Self-collection methods are designed to mimic professional collection techniques. However, the lack of direct supervision and standardized procedures can introduce variations. While some studies show comparable accuracy, others highlight potential discrepancies. These differences often stem from factors such as proper sample handling, technique, and the specific HPV type being tested.
Factors Influencing Accuracy
Several factors can influence the accuracy of self-collected HPV samples. These include the individual’s experience with the self-collection process, adherence to the provided instructions, and the overall quality of the sample. Factors like the presence of inflammation or recent sexual activity can potentially affect the results, impacting the ability to obtain a representative sample. It is important to be aware of these variables.
Potential Sources of Error
Potential sources of error in self-collection procedures include improper sample handling, insufficient sample volume, and contamination. These errors can lead to false-negative or false-positive results, impacting the interpretation of the test outcome. Thoroughly following the instructions and paying close attention to the collection procedure are essential for minimizing these errors.
Sensitivity and Specificity Comparison, Self collection hpv tests
Sensitivity and specificity are crucial metrics in evaluating the performance of any diagnostic test. Sensitivity measures the test’s ability to correctly identify those with the infection, while specificity measures its ability to correctly identify those without the infection. Studies comparing self-collection methods to professional collections often demonstrate similar levels of sensitivity and specificity, though further research is ongoing.
Interpreting Self-Collection Results
Interpreting the results of a self-collected HPV test is essential for appropriate follow-up. A positive result indicates the presence of HPV, necessitating further investigation and consultation with a healthcare professional. A negative result does not definitively rule out the possibility of infection, as it might be due to the factors discussed previously. Always consult a healthcare provider for proper interpretation and guidance.
Self-collection HPV tests are becoming increasingly popular, offering a convenient way to manage your health. While these tests are helpful, it’s important to remember that other oral symptoms, like those associated with herpangina viral infection of the mouth and throat, could potentially mimic some HPV-related symptoms. So, if you experience unusual oral discomfort, always consult a healthcare professional for proper diagnosis and treatment, even if you’ve already done a self-collection HPV test.
Accessibility and Cost-Effectiveness
Self-collection HPV tests offer a significant advancement in cervical cancer screening, promising wider access and potentially lower costs compared to traditional methods. This accessibility is particularly crucial for underserved populations and those facing logistical barriers to traditional clinic visits. The potential for cost savings, both for individuals and healthcare systems, is a key driver in the adoption of this technology.The affordability and ease of use of self-collection kits make them attractive for a broader range of individuals.
This accessibility is a significant step forward in promoting preventative health measures and reducing disparities in healthcare access.
Accessibility for Diverse Populations
Self-collection HPV tests are designed to be user-friendly and can be completed in the comfort of one’s own home. This accessibility is particularly beneficial for individuals in remote areas, those with mobility limitations, or those who experience barriers to traditional healthcare settings. The ability to conduct the test at a convenient time significantly reduces logistical challenges and encourages participation, especially for individuals who might otherwise delay or avoid testing.
Cost-Effectiveness Comparison
Self-collection HPV tests have the potential to reduce healthcare costs through increased participation rates and streamlined testing processes. Traditional methods often involve clinic visits, physician appointments, and laboratory analysis, which can be expensive and time-consuming. Self-collection kits often provide a more cost-effective alternative, especially when considering the overall healthcare costs associated with cervical cancer prevention and treatment.
Reduced Healthcare Costs
Self-collection HPV tests can contribute to a reduction in healthcare costs in several ways. Firstly, by encouraging wider participation in screening, they can help identify precancerous lesions earlier, allowing for timely intervention and potentially preventing more costly treatments later. Secondly, the reduced need for clinic visits and specialized personnel can lead to significant savings in healthcare infrastructure and operational costs.
Pricing Comparison
The cost-effectiveness of self-collection kits varies depending on the specific kit and the associated testing laboratory fees. However, in many cases, the cost of self-collection kits is lower than the combined costs of a traditional physician visit, laboratory analysis, and potentially follow-up appointments. A direct comparison of pricing for self-collection kits and traditional methods can vary depending on factors like insurance coverage, location, and specific testing laboratory partnerships.
Cost-Effectiveness Summary Table
| Feature | Traditional Method | Self-Collection Method |
|---|---|---|
| Initial Testing Cost | Higher (physician visit, lab analysis) | Lower (kit cost) |
| Follow-up Costs (if abnormal results) | Potentially higher (additional visits, procedures) | Potentially lower (if results are immediately actionable via telehealth or online follow-up) |
| Accessibility | Limited by clinic availability, transportation | Higher accessibility due to home-based testing |
| Convenience | Requires scheduling and travel | Convenient, self-administered at home |
| Potential for Increased Participation | Limited by logistical factors | Potentially higher participation due to ease of use |
| Overall Cost Savings | Potentially higher due to delayed detection | Potentially lower due to earlier detection and reduced follow-up costs |
Safety and Hygiene Practices
Self-collection HPV tests offer convenience and accessibility, but understanding and adhering to safety and hygiene practices is crucial for accurate results and to prevent potential complications. Proper techniques minimize the risk of infection and ensure the integrity of the collected sample. This section delves into the critical aspects of safety and hygiene during the self-collection process.
Safety Precautions for Handling Self-Collection Kits
Handling self-collection kits requires careful attention to safety procedures to prevent contamination and maintain the integrity of the sample. Always follow the manufacturer’s instructions meticulously, as they provide specific guidance for safe handling.
- Kit Sterilization: Ensure the kit components, especially the collection device, are properly sterilized. Sterilization procedures are typically detailed in the kit instructions. Improper sterilization can introduce contaminants, potentially affecting test results.
- Disposal Procedures: Adhere to the recommended disposal procedures for used materials. This is critical for preventing the spread of pathogens and protecting both yourself and others. Improper disposal can lead to environmental contamination.
- Personal Protective Equipment (PPE): Some self-collection kits may recommend the use of gloves to prevent contamination. Always wear gloves during the entire collection process. Gloves act as a barrier, protecting you from potential pathogens and the collected sample from external contaminants.
Importance of Hygiene During Self-Collection
Maintaining impeccable hygiene is paramount during the self-collection process to ensure a clean and uncontaminated sample. A clean collection site minimizes the risk of introducing contaminants that could compromise the accuracy of the test results.
- Handwashing: Thorough handwashing with soap and water before and after collection is essential. This is a fundamental hygiene practice that helps remove any bacteria or viruses from the hands, thus preventing contamination.
- Clean Collection Site: The collection site needs to be thoroughly cleaned to eliminate any potential contaminants. This is often achieved by applying a sterile cleaning solution to the target area.
- Avoiding Touching: Avoid touching the collection device’s collection tip or the inside of the collection container with your hands, except as instructed. This minimizes the risk of contaminating the sample.
Examples of Proper Hygiene Practices
Proper hygiene practices are crucial to the success of self-collection HPV tests. These examples provide a practical guide to maintaining a clean and safe environment for sample collection.
- Before collection: Thoroughly wash your hands with soap and water for at least 20 seconds. Dry your hands completely with a clean towel.
- During collection: Carefully follow the instructions provided with the kit. Avoid touching the collection area or the device unnecessarily. Ensure all the required steps are completed without contamination.
- After collection: Immediately dispose of used materials according to the kit’s instructions. Wash your hands again with soap and water.
Potential Risks and Complications
While generally safe, self-collection can present certain risks. Proper technique and attention to hygiene mitigate these risks.
- Minor discomfort: Some individuals may experience minor discomfort during the collection process. This is usually temporary and resolves without intervention.
- Infection: Contamination of the sample can potentially lead to infection. Maintaining proper hygiene and following instructions minimize this risk.
- False-positive/False-negative results: Inadequate hygiene can lead to inaccurate results, affecting the accuracy of the diagnosis. Following instructions carefully ensures the integrity of the sample and reduces the likelihood of errors.
Important: Always follow the specific instructions provided with your self-collection kit. Maintain proper hygiene throughout the process.
Ethical Considerations and Patient Counseling
Self-collection HPV tests offer a more accessible pathway to screening, but their implementation necessitates careful consideration of ethical implications and effective patient counseling. Ensuring informed consent, addressing potential anxieties, and empowering patients while maintaining the accuracy and reliability of the test are crucial components of this process. Open communication and thorough guidance are paramount to fostering trust and ensuring a positive patient experience.Patient autonomy is paramount in healthcare.
Self-collection empowers individuals to take ownership of their health, but it also requires careful consideration of their comfort level and understanding of the procedure. Ethical practice necessitates respecting patient choices, even if they differ from traditional healthcare models. Providing comprehensive information and addressing concerns are essential to ensuring that patients feel comfortable and confident in their decision to self-collect.
Importance of Patient Counseling Before Self-Collection
Comprehensive patient counseling is vital before initiating self-collection. This pre-collection counseling should go beyond simply explaining the procedure. It should address potential anxieties and concerns about the test’s accuracy, the potential for discomfort, and the importance of following instructions diligently. Counseling should also address the emotional implications of the results and support systems available.
Roles of Healthcare Providers in Guiding Patients
Healthcare providers play a crucial role in guiding patients through the self-collection process. Their role extends beyond simply providing instructions. Providers should act as educators, addressing anxieties and concerns, and facilitating informed consent. They should emphasize the importance of proper technique for accurate results and provide resources for addressing any discomfort. Providers must also be prepared to offer emotional support and connect patients with appropriate mental health services if needed.
Effective Communication Strategies for Counseling Patients
Effective communication strategies are essential to ensure that patients understand the self-collection process and feel comfortable. Clear and concise explanations, use of visual aids, and active listening are key elements. Open dialogue should address potential questions and concerns, fostering a supportive environment. Providing clear and accessible written materials, including detailed instructions and FAQs, can supplement in-person counseling.
Emphasizing the benefits of early detection and the importance of regular screening can further empower patients. Using patient-centered language and validating their emotions can build trust and encourage participation.
Table of Questions Patients May Have About Self-Collection
| Potential Question | Informative Response |
|---|---|
| Is self-collection accurate? | Studies have shown that when performed correctly, self-collection HPV tests can achieve comparable accuracy to clinician-collected samples. However, proper technique and adherence to instructions are critical. |
| What if I’m uncomfortable performing the procedure? | It’s completely understandable to feel some discomfort. We encourage open communication about any concerns or anxieties. Alternative approaches, such as having a partner or friend assist, may be helpful. |
| What if I make a mistake during the collection process? | If you believe you may have made a mistake during the collection process, contact your healthcare provider immediately for guidance. They can provide additional support and address any concerns. |
| What happens if the test result is positive? | A positive result indicates the presence of HPV. Your healthcare provider will discuss the implications of this result and recommend appropriate next steps. This may include further testing, treatment options, and follow-up appointments. |
| How can I prepare emotionally for the results? | Understanding the potential outcomes and preparing for different scenarios can be helpful. Discuss this with your healthcare provider. Resources for emotional support, such as counseling services, are available if needed. |
Future Trends and Advancements: Self Collection Hpv Tests
Self-collection HPV tests are rapidly evolving, driven by the need for increased accessibility and reduced healthcare burden. This evolution is fueled by technological advancements that promise to streamline the testing process, enhance accuracy, and ultimately improve cervical cancer prevention strategies. These advancements hold the key to wider adoption of self-testing and improved patient outcomes.The future of self-collection HPV testing hinges on innovations that simplify the procedure, improve the accuracy of results, and potentially even incorporate predictive biomarkers.
This will empower individuals to take charge of their health and reduce the reliance on traditional clinic visits, while ensuring reliable and high-quality data.
Emerging Technologies in Self-Collection Kits
The development of more user-friendly and precise self-collection kits is a key focus area. These advancements aim to minimize the learning curve for individuals performing the test, while maintaining or improving accuracy.
- Smart collection devices: Imagine a self-collection device equipped with embedded sensors that monitor the collection process in real-time. These sensors could ensure proper sample collection, identify potential errors, and provide immediate feedback to the user. This approach would greatly improve the reliability of results by reducing errors due to improper sampling techniques.
- Miniaturized and portable diagnostic platforms: Future kits may integrate miniaturized diagnostic platforms that perform on-site analysis of the collected sample. This “point-of-care” testing capability would allow for immediate results, reducing the waiting time for test outcomes and potentially enabling prompt interventions.
- AI-powered image analysis: Integrating artificial intelligence (AI) into the analysis of collected samples could further enhance the accuracy of HPV detection. AI algorithms can analyze images of the collected cells with higher precision and sensitivity than traditional methods, improving the identification of HPV-related abnormalities.
Potential Advancements in Procedure and Sample Handling
Innovations in the sample collection and handling procedures are also likely to play a crucial role in improving self-collection testing.
- Improved sampling tools: The design of sampling tools is likely to evolve, focusing on improved ergonomics and user experience. This would involve creating tools that are more comfortable and intuitive to use, ensuring a more efficient and accurate collection process. Consider the possibility of tools designed for specific anatomical variations or age groups.
- Enhanced sample preservation: Methods for preserving the collected sample’s integrity during transport and storage will be further refined. This could involve developing innovative preservation solutions that maintain the sample’s quality for an extended period, allowing for testing at a later time and improving logistical efficiency.
- Optimized sample processing: The processing of collected samples is crucial for accurate analysis. Further refinements to this process, such as automated cell separation techniques, could potentially improve the efficiency and reliability of HPV detection, reducing the need for extensive laboratory processing.
Impact on Healthcare and Public Health
These advancements have the potential to revolutionize cervical cancer prevention efforts.
- Increased accessibility: Self-collection HPV testing can make screening more accessible to individuals in underserved or geographically remote areas, who may have limited access to traditional healthcare facilities. This can lead to earlier detection of precancerous conditions and improved health outcomes.
- Reduced healthcare costs: By reducing the need for clinic visits and laboratory processing, self-collection testing could potentially lower the overall cost of HPV screening programs, making them more sustainable and accessible to a broader population.
- Empowerment and improved patient outcomes: Empowering individuals to take control of their health through self-testing can foster a sense of responsibility and promote proactive health management. This proactive approach can lead to early detection and improved treatment outcomes.
Epilogue

Self-collection HPV tests represent a significant advancement in accessible and convenient healthcare. While offering increased accessibility and potentially lower costs, accuracy remains a key consideration. This guide highlights the crucial aspects of self-collection, including proper procedures, safety measures, and ethical implications. By understanding these factors, individuals can make informed choices about their health and contribute to better health outcomes.