Blood flow through the heart sets the stage for understanding the intricate workings of the human circulatory system. This fascinating journey, from the body’s periphery to the heart and back again, is crucial for maintaining life. It’s a complex process involving chambers, valves, and vessels, all orchestrated to deliver oxygen and nutrients to our cells.
This detailed exploration will trace the path of blood through the heart, highlighting the roles of different structures. We’ll delve into the mechanisms that regulate this vital process, including the impact of exercise and disease. The heart’s remarkable ability to adapt to changing demands and the potential disruptions from disease will be key elements.
Introduction to Cardiovascular System
The human cardiovascular system is a complex network of interconnected vessels and organs that is vital for maintaining life. It efficiently transports oxygen, nutrients, hormones, and waste products throughout the body, ensuring the proper functioning of all tissues and organs. This intricate system is essential for maintaining homeostasis, the body’s internal balance, and its proper functioning. Understanding the components and their roles is crucial for comprehending the importance of this system in overall health.
Fundamental Components of the Circulatory System
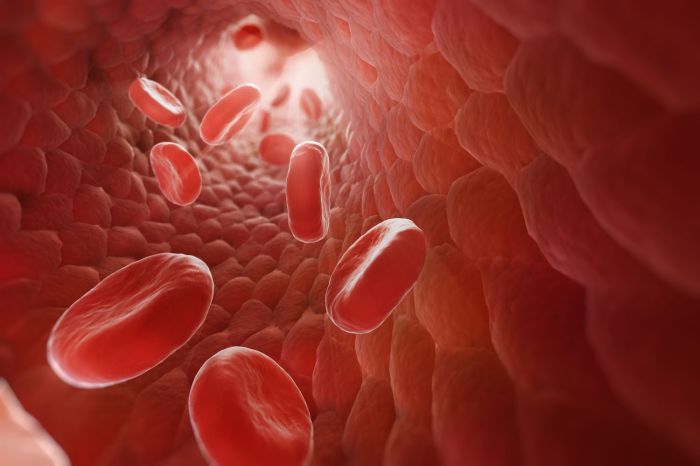
The circulatory system consists of the heart, blood vessels, and blood. These components work in concert to ensure the continuous movement of blood, facilitating the delivery of essential substances and the removal of waste products. The heart acts as the pump, driving blood through the vessels, while the blood vessels serve as conduits, carrying the blood to all parts of the body.
Blood, composed of various cells and plasma, carries vital substances, maintaining the body’s overall health.
| Component | Function | Location within the Circulatory System |
|---|---|---|
| Heart | The heart is the muscular pump that propels blood throughout the circulatory system. It rhythmically contracts and relaxes, creating pressure gradients that move blood through the arteries, capillaries, and veins. | Located in the thoracic cavity, between the lungs. |
| Blood Vessels (Arteries, Veins, Capillaries) | Blood vessels form a network of tubes that transport blood throughout the body. Arteries carry oxygenated blood away from the heart, veins return deoxygenated blood to the heart, and capillaries facilitate the exchange of nutrients and waste products between the blood and tissues. | Arteries branch from the heart, forming a network of vessels throughout the body. Veins collect blood from tissues and return it to the heart. Capillaries form a dense network in tissues, enabling the exchange of substances between blood and cells. |
| Blood | Blood is the fluid that circulates throughout the body, carrying oxygen, nutrients, hormones, and waste products. It is composed of red blood cells, white blood cells, platelets, and plasma. | Blood is constantly flowing through the heart and blood vessels, circulating throughout the body. |
Significance of Blood Flow in Maintaining Homeostasis
The continuous movement of blood is critical for maintaining homeostasis. Blood carries oxygen and nutrients essential for cellular respiration, providing energy for various bodily functions. It also transports hormones, which regulate various bodily processes, and removes waste products, preventing their accumulation and potential toxicity. Disruptions in blood flow can lead to a range of health issues, emphasizing the critical role of this continuous process in maintaining optimal health.
Structure of the Heart: Blood Flow Through The Heart
The heart, a marvel of biological engineering, is a muscular pump that tirelessly circulates blood throughout our bodies. Understanding its intricate structure is crucial to grasping how it performs this vital function. Its chambers, valves, and associated vessels work in concert to ensure efficient and unidirectional blood flow. This meticulous design is essential for maintaining life.The heart’s anatomy, while complex, can be broken down into manageable components.
Each part plays a specific role in the overall process of pumping blood, and understanding these components is key to comprehending the heart’s function.
Chambers of the Heart
The heart is divided into four chambers: two atria and two ventricles. The atria are the receiving chambers, collecting blood returning to the heart from the body and lungs. The ventricles are the pumping chambers, responsible for propelling blood out of the heart to the lungs and the rest of the body. This distinct separation of function is vital for maintaining the proper flow of blood.
Valves of the Heart
The heart’s valves act as one-way doors, ensuring that blood flows in the correct direction. Four valves—the mitral, tricuspid, pulmonary, and aortic valves—prevent backflow of blood, crucial for maintaining the unidirectional blood flow. Their precise function is essential for the heart’s efficient operation.
Major Vessels
The heart is connected to the rest of the body through a network of major vessels. The superior and inferior venae cavae return deoxygenated blood from the body to the right atrium. The pulmonary arteries carry deoxygenated blood to the lungs, and the pulmonary veins return oxygenated blood to the left atrium. The aorta carries oxygenated blood from the left ventricle to the rest of the body.
These vessels form a critical part of the circulatory system, ensuring a continuous flow of blood.
Structural Features for Unidirectional Blood Flow
The heart’s structure is meticulously designed to facilitate unidirectional blood flow. The valves, as previously mentioned, prevent backflow, and the arrangement of the chambers ensures that blood progresses through the heart in a consistent, controlled manner. This unidirectional flow is critical for efficient oxygen delivery and waste removal throughout the body.
Illustration of the Heart’s Internal Structure
Imagine a three-dimensional model of the heart. The right atrium, located on the heart’s right side, is the first chamber encountered. Blood enters from the superior and inferior venae cavae. A muscular wall, the interatrial septum, separates the right and left atria. The tricuspid valve connects the right atrium to the right ventricle, ensuring that blood flows only from the atrium to the ventricle.
Next is the right ventricle, which pumps blood through the pulmonary valve to the pulmonary arteries, bound for the lungs. The left atrium, located on the heart’s left side, receives oxygen-rich blood from the pulmonary veins. The mitral valve, similar to the tricuspid valve in function, connects the left atrium to the left ventricle. The left ventricle, the heart’s most muscular chamber, pumps oxygenated blood through the aortic valve into the aorta, the body’s main artery.
The interventricular septum, another muscular wall, divides the ventricles. The intricate arrangement of these components ensures that blood always flows in one direction.
Comparison of Atria and Ventricles
| Feature | Atria | Ventricles |
|---|---|---|
| Structure | Thin-walled, receiving chambers | Thick-walled, pumping chambers |
| Function | Collect blood returning to the heart | Pump blood out of the heart |
| Muscle Thickness | Thinner | Thicker |
| Valve Connection | Connected to the ventricles via atrioventricular valves (tricuspid and mitral) | Connected to major arteries via semilunar valves (pulmonary and aortic) |
This table highlights the key structural and functional differences between the atria and ventricles, emphasizing their specialized roles in the cardiac cycle.
Understanding how blood flows through your heart is crucial for overall health. Think about it like a powerful pump, constantly circulating life-giving oxygen. And while a healthy heart is essential, did you know that supporting healthy hair growth might also play a role? Certain nutrients can contribute to healthy hair growth, such as those found in chia seed oil for hair growth , which can promote strong and lustrous locks.
Ultimately, maintaining a healthy circulatory system, like the blood flow through the heart, is key to overall well-being.
Pathways of Blood Flow
Blood flows through the heart in a precise, cyclical manner, ensuring the efficient delivery of oxygen and nutrients to the body’s tissues. This intricate system of vessels and valves allows for the separation of oxygenated and deoxygenated blood, preventing mixing and maintaining a unidirectional flow. Understanding these pathways is crucial for grasping the heart’s vital role in circulation.
Understanding blood flow through the heart is crucial for overall health. It’s a fascinating process, but sometimes other factors can affect our bodies, like wondering if magnesium supplements could be causing digestive issues like diarrhea. For more information on whether magnesium can cause diarrhea, check out this helpful resource: can magnesium cause diarrhea. Regardless of magnesium intake, a healthy heart and consistent blood flow remain vital for our well-being.
Tracing Blood Flow Through the Heart
The heart acts as a pump, pushing blood through a complex network of vessels. Oxygen-poor blood returns to the heart and is pumped to the lungs for oxygenation, while oxygen-rich blood is circulated to the rest of the body. This process is continuous and ensures a constant supply of oxygen and nutrients to the tissues.
Role of Heart Valves
Heart valves are crucial components of the cardiovascular system, ensuring one-way blood flow. They act as gates, opening and closing in response to pressure changes within the heart chambers. This regulated opening and closing prevents backflow, maintaining the efficient circulation of blood. The four heart valves—tricuspid, pulmonary, mitral, and aortic—play distinct roles in this process.
Step-by-Step Blood Flow Through the Heart
The following sequence Artikels the path of blood through the heart:
- Deoxygenated blood enters the right atrium from the superior and inferior vena cava.
- The right atrium contracts, pushing blood through the tricuspid valve into the right ventricle.
- The right ventricle contracts, forcing blood through the pulmonary valve into the pulmonary artery.
- The pulmonary artery carries the deoxygenated blood to the lungs for oxygenation.
- Oxygenated blood returns from the lungs via the pulmonary veins to the left atrium.
- The left atrium contracts, pushing blood through the mitral valve into the left ventricle.
- The left ventricle contracts, forcing blood through the aortic valve into the aorta.
- The aorta distributes the oxygenated blood to the rest of the body.
Relationship Between Cardiac Cycle and Blood Flow
The cardiac cycle, encompassing the rhythmic contraction and relaxation of the heart, is intricately linked to blood flow. Each phase of the cycle—atrial systole, ventricular systole, and diastole—contributes to the forward movement of blood. The coordinated action of the heart chambers, regulated by electrical impulses, ensures a continuous and efficient blood flow. The rhythmic contraction and relaxation of the heart chambers, driven by the cardiac cycle, create the pressure gradient necessary to move blood through the circulatory system.
Regulation of Blood Flow
The delicate dance of blood flow through our cardiovascular system isn’t a random process. Precise mechanisms govern heart rate, blood pressure, and overall blood flow to ensure the body’s needs are met. This intricate regulation is crucial for maintaining homeostasis and responding to changes in demand, from a leisurely stroll to intense exercise. Understanding these control mechanisms allows us to appreciate the complexity and efficiency of our circulatory system.The regulation of blood flow is a dynamic interplay between various factors, primarily the autonomic nervous system and hormones.
Understanding how blood flows through the heart is fascinating, right? But did you know that sometimes, dealing with menstrual cramps can throw a wrench into your body’s systems? It’s a common question: do bananas help with cramps? Checking out this resource might offer some insights: do bananas help with cramps. Regardless of the answer, the intricate network of blood vessels and chambers within the heart continues its vital work, keeping everything running smoothly.
These systems work in concert to adjust heart rate and blood pressure, ensuring an adequate supply of oxygen and nutrients to all tissues. The precise control allows the body to respond rapidly to changing needs, like increased physical activity, and maintain a stable internal environment.
Heart Rate Control Mechanisms
The heart’s rhythmic contractions, or heart rate, are meticulously controlled by the autonomic nervous system. This system, comprised of the sympathetic and parasympathetic branches, acts as a fine-tuning mechanism for cardiovascular function.
Autonomic Nervous System Regulation of Cardiac Output
The autonomic nervous system plays a critical role in modulating cardiac output, the volume of blood pumped by the heart per minute. The sympathetic nervous system, known for its “fight-or-flight” response, increases heart rate and contractility, boosting cardiac output. Conversely, the parasympathetic nervous system, associated with “rest-and-digest” functions, slows heart rate, decreasing cardiac output. This balanced interplay ensures that heart rate adapts to the body’s changing needs.
Hormonal Influences on Blood Flow
Hormones, chemical messengers in the body, also influence blood flow. Epinephrine (adrenaline) and norepinephrine, released during stress or exercise, stimulate the sympathetic nervous system, leading to increased heart rate and blood pressure. Other hormones, such as thyroid hormones, can influence metabolic rate, which, in turn, impacts the body’s need for blood flow. For example, increased metabolic rate might require an increase in blood flow to supply the body’s increased energy needs.
Sympathetic vs. Parasympathetic Nervous System Effects
| Characteristic | Sympathetic Nervous System | Parasympathetic Nervous System |
|---|---|---|
| Effect on Heart Rate | Increases heart rate | Decreases heart rate |
| Effect on Blood Vessels (generally) | Causes vasoconstriction (narrowing) in most blood vessels, except those supplying skeletal muscles | Causes vasodilation (widening) in some blood vessels |
| Effect on Blood Pressure | Increases blood pressure | Decreases blood pressure |
| Effect on Bronchioles (airways) | Causes bronchodilation (widening) | Causes bronchoconstriction (narrowing) |
| Dominant State | Fight-or-flight response | Rest-and-digest response |
These opposing effects of the sympathetic and parasympathetic systems create a dynamic balance, allowing for rapid adjustments in cardiovascular function based on the body’s needs. The interplay between these two systems ensures homeostasis, enabling the body to respond appropriately to changing demands, from a quiet moment of rest to a period of intense physical exertion. This complex regulatory system is crucial for maintaining blood pressure and ensuring an adequate blood supply to all tissues and organs.
Clinical Considerations
The intricate dance of blood flow through the heart is crucial for life. Disruptions to this delicate system can lead to a range of serious health problems. Understanding these conditions, the factors that cause them, and the diagnostic and treatment options available is vital for maintaining cardiovascular health.Common heart conditions that disrupt blood flow are numerous and diverse.
Some involve structural abnormalities, while others stem from functional impairments. These conditions can manifest in various ways, impacting the heart’s ability to pump blood efficiently and consistently.
Common Heart Conditions Affecting Blood Flow
Numerous conditions can disrupt the normal flow of blood through the heart. These conditions can lead to reduced cardiac output, impaired oxygen delivery, and a range of other complications. Understanding the underlying mechanisms of these conditions is key to developing effective diagnostic and therapeutic strategies.
- Coronary Artery Disease (CAD): CAD is characterized by the buildup of plaque in the coronary arteries, the blood vessels that supply the heart muscle with oxygen. This plaque buildup narrows the arteries, reducing blood flow to the heart muscle, potentially leading to angina (chest pain) or a heart attack if the blood supply is completely blocked. This condition is often associated with risk factors such as high blood pressure, high cholesterol, smoking, and diabetes.
Many individuals lead lives free of symptoms, yet experience significant cardiac complications due to plaque buildup in the coronary arteries.
- Valvular Heart Disease: Valvular heart disease occurs when one or more of the heart valves do not function properly. This can be due to stenosis (narrowing of the valve) or regurgitation (leaking of the valve). These conditions can disrupt the normal flow of blood through the heart, leading to symptoms such as shortness of breath, fatigue, and palpitations. Valvular heart disease is often treated with medication, surgery, or a combination of both.
- Congenital Heart Defects: These are structural abnormalities in the heart that are present at birth. They can range from minor issues to severe conditions that require immediate intervention. Examples include septal defects (holes in the heart walls), valve abnormalities, and narrowing of blood vessels. These conditions can disrupt the normal mixing of oxygenated and deoxygenated blood, leading to various circulatory problems.
Proper diagnosis and intervention during infancy and childhood are essential to improve long-term health outcomes.
Factors Disrupting Normal Blood Flow Patterns
Various factors can disrupt the normal flow of blood through the heart. These factors can contribute to the development of various cardiovascular conditions. Understanding these factors is crucial for preventative measures and early intervention.
- High Blood Pressure: Sustained high blood pressure, or hypertension, puts extra strain on the heart and blood vessels. This increased pressure can damage the arteries over time, leading to atherosclerosis (plaque buildup) and potentially causing heart attacks or strokes. Hypertension is a significant risk factor for cardiovascular disease, and lifestyle modifications and medication are often employed to manage it.
- High Cholesterol: High levels of cholesterol in the blood can contribute to the formation of plaque in the arteries, reducing blood flow. This condition can also lead to atherosclerosis and increase the risk of cardiovascular events. Dietary changes, lifestyle adjustments, and medications are often used to manage high cholesterol.
- Smoking: Smoking damages blood vessels, increases blood clotting, and raises blood pressure. These effects increase the risk of developing various cardiovascular conditions, including CAD and stroke. Quitting smoking is crucial for improving cardiovascular health.
Diagnostic Methods for Assessing Blood Flow
Various diagnostic techniques are used to assess blood flow through the heart. These methods provide crucial information about the structure and function of the heart, enabling accurate diagnosis and treatment planning.
- Electrocardiogram (ECG): An ECG measures the electrical activity of the heart. It can detect abnormal rhythms, heart damage, and the presence of certain conditions. It is a non-invasive and relatively quick test.
- Echocardiogram (Echo): An echocardiogram uses ultrasound waves to create images of the heart. It allows visualization of the heart’s structures, valves, and overall function, including blood flow patterns. It’s a valuable tool for diagnosing various heart conditions.
- Cardiac Catheterization: Cardiac catheterization involves inserting a thin tube (catheter) into an artery or vein and guiding it to the heart. It allows direct visualization of the coronary arteries, measurement of blood pressure, and assessment of blood flow. This method provides detailed information about the heart’s structure and function, particularly concerning coronary arteries.
Treatment Options for Conditions Affecting Blood Flow
Various treatment options are available for conditions affecting blood flow through the heart. The chosen approach depends on the specific condition, its severity, and the patient’s overall health.
- Lifestyle Modifications: Dietary changes, regular exercise, and stress management can significantly improve cardiovascular health and reduce the risk of various heart conditions. These modifications are often a crucial component of treatment, particularly for preventing the progression of existing conditions.
- Pharmacological Interventions: Medications such as blood pressure medications, cholesterol-lowering drugs, and anti-platelet agents are commonly used to manage conditions affecting blood flow. These medications help control risk factors and improve overall cardiovascular health.
- Surgical Interventions: Procedures like angioplasty, coronary artery bypass grafting (CABG), and valve replacement are used to address structural abnormalities or blockages affecting blood flow. Surgical interventions are often employed to restore normal blood flow when other methods are ineffective.
Blood Flow and Exercise

Exercise significantly impacts blood flow throughout the body, placing a heightened demand on the cardiovascular system. The heart, as the primary pump, must adapt to deliver increased oxygen and nutrients to working muscles. This adaptation involves a complex interplay of physiological responses, ensuring efficient blood delivery and oxygen utilization.
Effects of Exercise on Heart Rate
Heart rate increases substantially during exercise to meet the elevated oxygen demands of the body. This increase is a direct result of the sympathetic nervous system’s activation, which stimulates the sinoatrial (SA) node, the heart’s natural pacemaker. Higher heart rates facilitate faster blood circulation, delivering more oxygenated blood to the working muscles. For example, during intense aerobic exercise, heart rates can reach 180-200 beats per minute in trained athletes, whereas resting heart rates typically range from 60-80 beats per minute.
Effects of Exercise on Stroke Volume
Stroke volume, the amount of blood pumped by the heart with each beat, also increases during exercise. This is primarily due to enhanced ventricular filling during diastole and a stronger ventricular contraction during systole. Increased venous return, facilitated by muscle contractions and respiratory movements, leads to greater preload, stretching the ventricles and improving their contractile force (Frank-Starling mechanism).
Additionally, sympathetic stimulation strengthens ventricular contractions, further augmenting stroke volume.
Effects of Exercise on Cardiac Output
Cardiac output, the total amount of blood pumped by the heart per minute, is the product of heart rate and stroke volume. Consequently, exercise dramatically elevates cardiac output to match the increased oxygen needs of active tissues. For instance, during vigorous exercise, cardiac output can increase four to seven times its resting value, ensuring adequate oxygen delivery to the working muscles.
Changes in Cardiovascular Parameters During Exercise
The following table Artikels the typical changes in heart rate, stroke volume, and cardiac output during various intensities of exercise:
| Exercise Intensity | Heart Rate (bpm) | Stroke Volume (mL/beat) | Cardiac Output (L/min) |
|---|---|---|---|
| Light | 70-120 | 80-100 | 5.6-12 |
| Moderate | 120-150 | 100-120 | 12-18 |
| Vigorous | 150-180+ | 120-150+ | 18-35+ |
Long-Term Effects of Exercise on Cardiovascular Health
Regular exercise has numerous beneficial long-term effects on cardiovascular health. It strengthens the heart muscle, making it more efficient at pumping blood. This enhanced contractility lowers the resting heart rate and reduces the risk of hypertension and other cardiovascular diseases. Furthermore, exercise promotes the development of a more robust vascular system, with improved blood vessel elasticity and reduced plaque buildup.
For example, individuals who consistently engage in aerobic exercise demonstrate a lower incidence of coronary artery disease and a reduced risk of stroke compared to those who are sedentary.
Blood Flow and Disease
Heart disease, a broad category encompassing various conditions affecting the heart’s structure and function, significantly impacts blood flow. These conditions can lead to reduced blood supply to vital organs, potentially causing serious complications. Understanding the interplay between heart diseases and blood flow is crucial for effective prevention and treatment strategies.
Coronary Artery Disease (CAD), Blood flow through the heart
Coronary artery disease, a leading cause of heart disease, is characterized by the buildup of plaque within the coronary arteries, the blood vessels that supply blood to the heart muscle. This plaque buildup narrows the arteries, reducing blood flow to the heart. This reduced blood flow can lead to angina (chest pain), heart attack, or even sudden cardiac death.
The extent of the narrowing and the location of the blockage directly influence the severity of the symptoms.
Valvular Heart Disease
Valvular heart disease affects the heart’s valves, which regulate the flow of blood through the heart. Damaged or diseased valves can cause blood to leak backward (regurgitation) or obstruct blood flow (stenosis). These issues can strain the heart and lead to symptoms like shortness of breath, fatigue, and swelling in the legs. The specific valve affected and the severity of the dysfunction determine the impact on blood flow.
Impact on the Heart’s Pumping Ability
Heart diseases significantly impair the heart’s ability to pump blood effectively. In CAD, the reduced blood supply deprives the heart muscle of oxygen and nutrients, leading to weakened contractions. Valvular heart disease puts extra strain on the heart as it works harder to overcome the obstructed or leaking blood flow. These impairments can result in reduced cardiac output, meaning less blood is circulated throughout the body.
Physiological Changes
The physiological changes resulting from heart disease are varied and complex. In CAD, the heart muscle can experience ischemia (lack of blood flow), leading to damage and scarring. Valvular disease can cause hypertrophy (enlargement) of the heart chambers as the heart compensates for the increased workload. The degree of these changes correlates with the severity and duration of the disease.
Comparison of Heart Diseases and Their Effects
| Heart Disease | Mechanism of Reduced Blood Flow | Impact on Pumping Ability | Physiological Changes | Symptoms |
|---|---|---|---|---|
| Coronary Artery Disease (CAD) | Plaque buildup narrows coronary arteries, reducing blood supply to the heart muscle. | Reduced cardiac output due to impaired heart muscle function. | Ischemia, damage, and scarring of the heart muscle; possible hypertrophy. | Angina, shortness of breath, fatigue, heart attack, sudden cardiac death. |
| Valvular Heart Disease | Damaged valves cause leakage (regurgitation) or obstruction (stenosis) of blood flow through the heart. | Increased workload on the heart, potentially leading to reduced cardiac output and heart failure. | Hypertrophy of affected heart chambers, valve damage. | Shortness of breath, fatigue, swelling in the legs, palpitations. |
Concluding Remarks
In conclusion, blood flow through the heart is a remarkable feat of biological engineering. From the intricate structure of the heart to the regulatory mechanisms that govern its function, this intricate process is essential for life. Understanding this process is vital for appreciating the delicate balance of the human body and the importance of preventative measures against disease.