Major differences between leukemia and lymphoma are crucial for understanding these blood cancers. While both are serious, they originate from different cells and have distinct characteristics in their symptoms, diagnosis, treatment, and prognosis. This exploration delves into the key distinctions between these often-confused diseases.
Leukemia and lymphoma, though both categorized as blood cancers, represent vastly different cellular origins and disease progressions. This in-depth look will explore the unique biological mechanisms, symptom profiles, diagnostic approaches, and treatment strategies that set them apart. Understanding these variations is essential for effective patient care and improved outcomes.
Introduction to Leukemia and Lymphoma
Leukemia and lymphoma are both cancers of the blood and lymphatic systems, but they differ significantly in their origins, biological mechanisms, and the cells they affect. Understanding these distinctions is crucial for accurate diagnosis and effective treatment. Both conditions involve uncontrolled cell growth, but the specific cell types involved and the way these cells spread through the body distinguish them.These blood cancers, though sharing the common thread of uncontrolled cell growth, originate from different types of blood cells and exhibit distinct patterns of progression.
Their varying biological mechanisms and the types of cells involved lead to unique symptoms and treatment approaches. This difference in cellular origins and behaviors is crucial to recognizing and differentiating these diseases.
Origins and Classifications of Leukemia and Lymphoma, Major differences between leukemia and lymphoma
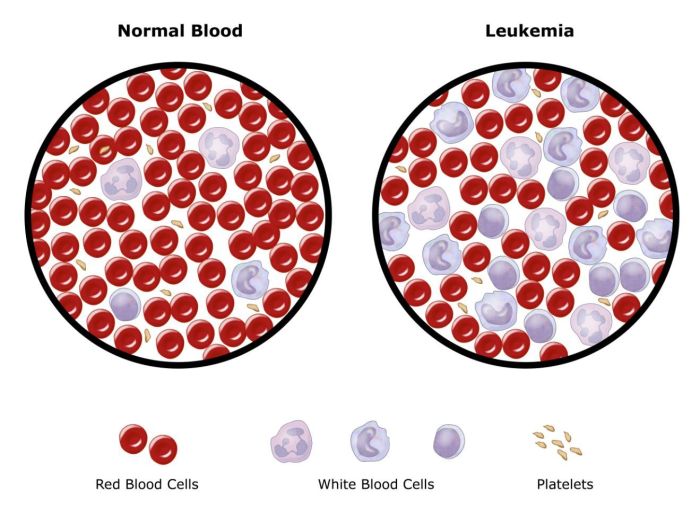
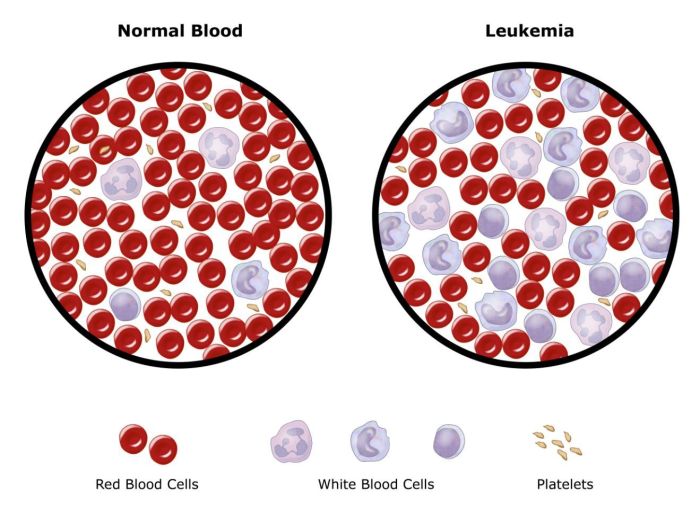
Leukemia arises from the hematopoietic stem cells in the bone marrow, leading to the uncontrolled proliferation of white blood cells, red blood cells, or platelets. Lymphoma, conversely, originates from lymphocytes, a type of white blood cell crucial for the immune system, within the lymphatic system. This distinction in origin dictates the different locations where the cancers might first manifest and the types of symptoms that may be observed.
Biological Mechanisms Differentiating Leukemia and Lymphoma
Leukemia is characterized by the proliferation of abnormal blood cells within the bone marrow, which then spill into the bloodstream, often affecting multiple organs. Lymphoma, on the other hand, involves the uncontrolled growth of lymphocytes, often forming solid tumors in lymph nodes or other lymphatic tissues. This difference in cellular proliferation and spread mechanisms impacts the presentation and treatment of each condition.
Cell Types Involved in Leukemia and Lymphoma
Leukemia involves a wide array of blood cells, including myeloid and lymphoid cells, which may mature into various types of blood cells, leading to varied clinical presentations. Lymphoma, however, primarily affects lymphocytes, a specialized type of white blood cell that plays a critical role in the immune system’s response to pathogens. The specific type of lymphocyte involved can also impact the disease’s progression and response to treatment.
Comparison of Origins
| Leukemia | Lymphoma |
|---|---|
| Originates from hematopoietic stem cells in bone marrow. | Originates from lymphocytes within the lymphatic system. |
| Characterized by abnormal blood cell proliferation in the bone marrow, often spreading to other tissues. | Characterized by the uncontrolled growth of lymphocytes, often forming tumors in lymph nodes or other lymphatic tissues. |
| May involve multiple types of blood cells (myeloid, lymphoid, etc.). | Primarily affects lymphocytes (B-cells or T-cells). |
Symptoms and Presentation: Major Differences Between Leukemia And Lymphoma
Understanding the symptoms of leukemia and lymphoma is crucial for early diagnosis and appropriate treatment. Both diseases can manifest in a variety of ways, and recognizing these patterns can significantly impact patient outcomes. Symptoms often overlap, making differentiation challenging without proper medical evaluation.Early detection is often key to successful treatment. This section details the common presenting symptoms of both diseases, highlighting how these symptoms might differ based on the specific subtype.
Common Presenting Symptoms of Leukemia
Leukemia typically develops insidiously, with initial symptoms often subtle and easily mistaken for other conditions. Early signs can include fatigue, weakness, and unexplained weight loss. These general symptoms can be indicators of a variety of health issues.
- Fatigue and Weakness: Persistent tiredness and a general lack of energy are frequently reported. This can stem from reduced red blood cell production, impacting oxygen delivery throughout the body.
- Unexplained Weight Loss: Significant weight loss without dietary changes or increased activity levels is a potential sign. This may be related to the body’s inflammatory response to the cancerous cells.
- Frequent Infections: The immune system is often compromised, making individuals more susceptible to infections, such as colds, flu, or other illnesses. This is a result of the cancerous cells crowding out healthy immune cells.
- Bleeding and Bruising: Easy or unusual bruising and bleeding can be a result of abnormal blood cell production. This is a consequence of the bone marrow being overrun by cancerous cells.
- Swollen Lymph Nodes: While less common in leukemia compared to lymphoma, swollen lymph nodes in the neck, armpits, or groin can sometimes be present, indicating the involvement of the lymphatic system.
Common Presenting Symptoms of Lymphoma
Lymphoma, unlike leukemia, often presents with noticeable symptoms related to the lymphatic system, including swollen lymph nodes.
- Swollen Lymph Nodes: Enlarged lymph nodes, particularly in the neck, armpits, or groin, are a hallmark symptom. The size and location of the affected nodes can vary depending on the type of lymphoma.
- Persistent Fever and Chills: Unexplained fevers and chills, often recurring, can indicate the disease’s activity and inflammation.
- Night Sweats: Excessive sweating during sleep, often accompanied by chills, is another frequent symptom. This can be a result of the body’s response to the disease.
- Unexplained Weight Loss: Like leukemia, significant weight loss without a change in diet or exercise can be an indicator of the disease’s presence.
- Fatigue and Weakness: Similar to leukemia, fatigue and weakness are common symptoms of lymphoma, arising from the body’s struggle to combat the cancerous cells.
Comparison of Symptom Presentation
The table below summarizes the common presenting symptoms for leukemia and lymphoma, highlighting the differences and overlaps.
| Symptom | Leukemia | Lymphoma |
|---|---|---|
| Fatigue and Weakness | Common, often early sign | Common, often as disease progresses |
| Unexplained Weight Loss | Common | Common |
| Frequent Infections | Common, due to immune compromise | Less common, but can occur |
| Bleeding and Bruising | Common | Less common, but possible |
| Swollen Lymph Nodes | Less common | Common, often a key initial sign |
| Persistent Fever and Chills | Less common | Common |
| Night Sweats | Less common | Common |
Variation in Symptoms by Subtype
The specific subtype of leukemia or lymphoma can influence the presentation of symptoms. For instance, acute lymphoblastic leukemia (ALL) often presents with more aggressive symptoms early on, compared to chronic lymphocytic leukemia (CLL). Similarly, Hodgkin lymphoma often has different symptom patterns than non-Hodgkin lymphoma.
Diagnostic Procedures
Pinpointing the difference between leukemia and lymphoma relies heavily on precise diagnostic procedures. These procedures help distinguish the distinct characteristics of these blood cancers, allowing for tailored treatment plans. A crucial element in successful patient management is the accurate identification of the specific type of cancer.
Blood Tests
Blood tests are fundamental initial screenings for both leukemia and lymphoma. Complete blood counts (CBCs) provide critical information about the levels of different blood cells, revealing potential abnormalities indicative of either condition. Variations in white blood cell counts, red blood cell counts, and platelet counts can suggest the presence of cancerous cells. Biochemistry panels assess liver and kidney function, which can be affected by the presence of cancer.
These panels provide additional clues for further investigations.
Bone Marrow Aspiration and Biopsy
Bone marrow aspiration and biopsy are crucial procedures for diagnosing leukemia. Bone marrow is the spongy tissue within bones that produces blood cells. In leukemia, abnormal cells accumulate in the bone marrow, displacing healthy cells. Aspirating a small sample of bone marrow fluid allows for a visual examination of the cells. A bone marrow biopsy, on the other hand, involves extracting a small core sample of bone marrow tissue.
The cells from both the aspirate and the biopsy are examined under a microscope by hematopathologists to identify the presence of cancerous cells, their characteristics, and their level of maturity. This crucial procedure is vital for distinguishing between various types of leukemia and assessing the aggressiveness of the disease.
Lymph Node Biopsy
Lymph node biopsies are critical in the diagnosis of lymphoma. Lymph nodes are small, bean-shaped structures throughout the body that play a role in the immune system. In lymphoma, these nodes can become enlarged and contain abnormal lymphocytes (a type of white blood cell). A lymph node biopsy involves removing a lymph node and examining it under a microscope.
The presence of cancerous cells, their characteristics, and the pattern of their growth are evaluated to determine the type of lymphoma. This procedure helps identify the type of lymphoma and assess its stage, guiding treatment decisions.
Diagnostic Tests Comparison
| Test | Leukemia | Lymphoma |
|---|---|---|
| Complete Blood Count (CBC) | Significant abnormalities in white blood cell, red blood cell, and platelet counts; often showing a high white blood cell count or low red blood cell count. | May show mild abnormalities or normal results, depending on the stage and type. |
| Bone Marrow Aspiration and Biopsy | Essential for identifying the presence of abnormal cells, determining their type, and assessing their maturity. | Generally not the first-line diagnostic test, but may be performed in cases of suspicion or to assess the extent of the disease. |
| Lymph Node Biopsy | Not typically used as a primary diagnostic tool; usually, a lymph node biopsy is not a primary test in leukemia cases. | Essential for confirming the diagnosis, identifying the type of lymphoma, and assessing its stage. |
| Biochemistry Panels | Can reveal liver or kidney dysfunction related to the disease or its treatment. | Can reveal liver or kidney dysfunction related to the disease or its treatment. |
Diagnostic Accuracy and Sensitivity
The accuracy and sensitivity of diagnostic tests vary depending on the specific test and the individual patient’s situation. For example, a CBC might indicate a possibility of leukemia, but further tests like bone marrow aspiration are necessary for confirmation. Similarly, while lymph node biopsies are crucial for lymphoma diagnosis, additional imaging studies might be needed to assess the extent of the disease.
In some cases, a combination of tests may be necessary to arrive at a definitive diagnosis. It’s important to remember that no single test is perfect, and a thorough evaluation by healthcare professionals is crucial for accurate diagnosis and appropriate treatment.
Treatment Approaches
Cancer treatment, whether leukemia or lymphoma, is a complex and personalized journey. It’s not a one-size-fits-all approach; treatment plans are tailored to the specific type and stage of the cancer, as well as the patient’s overall health. Understanding the different treatment modalities and their roles in each type of cancer is crucial for informed decision-making.The primary goals of treatment are to eliminate the cancerous cells, minimize damage to healthy tissues, and maximize the patient’s quality of life.
Different treatment strategies, ranging from chemotherapy to targeted therapies, are employed to achieve these goals. The effectiveness and suitability of each strategy are assessed on an individual basis.
General Treatment Approaches for Leukemia
Leukemia, characterized by the uncontrolled proliferation of white blood cells, often requires a multi-pronged approach. Treatment typically involves a combination of therapies, often starting with induction therapy to bring the cancer into remission. This is followed by consolidation therapy to eradicate any remaining cancer cells and then maintenance therapy to prevent relapse.
Standard Treatment Options for Lymphoma
Lymphoma treatment varies based on the specific type of lymphoma. Hodgkin lymphoma, for example, often responds well to radiation therapy, while non-Hodgkin lymphoma may be treated with chemotherapy, radiation, or a combination of both. In some cases, stem cell transplantation may be considered for aggressive or relapsed lymphomas. The choice of treatment depends on the stage, subtype, and overall health of the patient.
Comparison of Treatment Strategies
While both leukemia and lymphoma can be treated with chemotherapy, radiation therapy, and targeted therapies, the specific approaches and their effectiveness vary significantly. The aggressive nature of leukemia often necessitates more intensive and potentially more prolonged treatment regimens compared to lymphoma. The location and spread of the cancer also play a critical role in determining the most suitable treatment plan.
Treatment Comparison Table
| Treatment Type | Leukemia | Lymphoma |
|---|---|---|
| Chemotherapy | Frequently used, often in combination regimens for induction, consolidation, and maintenance. | Used in various combinations, depending on the lymphoma type and stage. May be the primary treatment or part of a multi-modal approach. |
| Radiation Therapy | May be used in some cases, often in localized forms of leukemia or in conjunction with other therapies. | Commonly used, particularly for localized lymphoma, and often combined with chemotherapy for more advanced stages. |
| Targeted Therapies | Emerging as important treatment options, particularly for specific leukemia subtypes, targeting specific molecular pathways. | Used in certain lymphoma subtypes, targeting specific genetic mutations or proteins involved in cancer growth. |
| Stem Cell Transplantation | Potentially curative for some leukemia types, especially in cases of relapse or aggressive forms. | Considered for aggressive or relapsed lymphomas, offering a potential cure for some. |
Role of Chemotherapy, Radiation, and Targeted Therapies
Chemotherapy drugs work by killing rapidly dividing cells, including cancer cells. In leukemia, chemotherapy is often a cornerstone of treatment, aiming to reduce the cancer burden and achieve remission. Radiation therapy targets cancer cells with high-energy beams, effective in shrinking tumors and destroying cancer cells, particularly useful in lymphoma, especially Hodgkin lymphoma. Targeted therapies, on the other hand, target specific molecular pathways driving cancer growth, offering precision treatment options.
Their use is often tailored to specific genetic characteristics of the cancer.
While understanding the key differences between leukemia and lymphoma is crucial for diagnosis and treatment, it’s also important to maintain a healthy lifestyle. Did you know that incorporating smoothies with seeds into your diet can significantly impact glycemic control? Smoothies with seeds glycemic control are a delicious and potentially beneficial addition to a balanced approach to health.
Ultimately, staying informed about health conditions like leukemia and lymphoma remains vital for preventative care and treatment.
Prognosis and Survival Rates
Understanding the prognosis, or expected outcome, of leukemia and lymphoma is crucial for patients and their families. It allows for informed decision-making regarding treatment options and helps manage expectations. The prognosis varies significantly based on several factors, including the specific type of cancer, its stage at diagnosis, and the individual’s overall health.The survival rates for both leukemia and lymphoma have improved dramatically in recent decades, largely due to advancements in diagnostic techniques and treatment approaches.
However, the specific prognosis for each patient remains unique and dependent on these factors. This section will delve into the factors that influence survival rates and provide an overview of the expected outcomes for different types of leukemia and lymphoma.
Prognosis for Different Types of Leukemia
Leukemia prognosis varies widely depending on the specific subtype. Acute leukemias, characterized by rapid growth and aggressive behavior, typically have a more challenging prognosis compared to chronic leukemias. For example, acute lymphoblastic leukemia (ALL) in children often has a higher cure rate than in adults, but even then, the specific outcome can depend on factors such as the presence of specific genetic abnormalities.
Chronic myeloid leukemia (CML) with appropriate treatment, including targeted therapies, has a more favorable outlook, with many patients living for many years with the disease in a stable condition.
Prognosis for Different Types of Lymphoma
Lymphoma prognosis also varies significantly based on the type of lymphoma. Hodgkin lymphoma, often diagnosed at an earlier stage, generally has a better prognosis than non-Hodgkin lymphoma. The subtype of non-Hodgkin lymphoma, along with the stage of the disease, greatly influences the expected outcome. Early-stage lymphomas, especially those diagnosed and treated promptly, often have high cure rates.
Comparison of Overall Survival Rates
While advancements in treatment have improved overall survival rates for both leukemia and lymphoma, the specific rates differ significantly based on the type and stage of the disease. Factors such as age, the presence of specific genetic mutations, and other medical conditions can also affect the prognosis. A significant challenge is that even with the best treatments, relapse can occur, impacting long-term survival.
Understanding the key differences between leukemia and lymphoma is crucial for diagnosis and treatment. While both are cancers of the blood and lymphatic systems, they originate in different cell types. For those seeking alternative approaches to managing conditions like multiple sclerosis, exploring the potential benefits of the Wahls Protocol might be worth considering. Reasons to try the Wahls protocol for MS are often discussed in terms of dietary changes and lifestyle modifications.
Ultimately, however, it’s important to remember that consulting with healthcare professionals about any medical concerns is paramount. Knowing the specifics of these blood cancers is essential for effective care.
Variability in Prognosis: A Table
| Type of Cancer | Stage | Survival Rate (approximate) |
|---|---|---|
| Acute Lymphoblastic Leukemia (ALL) – Childhood | Early Stage | 80-90% |
| Acute Myeloid Leukemia (AML) – Adult | Early Stage | 30-40% |
| Chronic Lymphocytic Leukemia (CLL) | Early Stage | 70-80% |
| Hodgkin Lymphoma | Early Stage | 85-95% |
| Non-Hodgkin Lymphoma – Diffuse Large B-cell | Stage III | 50-60% |
Note: Survival rates are approximate and can vary greatly depending on individual factors and treatment responses. These are just examples and are not exhaustive.
Factors Influencing Prognosis
Several factors contribute to the prognosis of leukemia and lymphoma. The stage of the disease at diagnosis is a critical factor, with earlier-stage cancers generally having better prognoses. The specific subtype of the cancer also plays a significant role, with some types having a higher likelihood of remission or cure. Patient characteristics, including age, overall health, and response to treatment, also influence the prognosis.
Risk Factors and Prevention
Understanding the potential triggers for leukemia and lymphoma is crucial for proactive measures. While a definitive cause isn’t always pinpointed, certain factors increase the likelihood of developing these blood cancers. This section explores the known risk factors and potential preventative strategies to minimize the chances of these diseases.
Potential Risk Factors for Leukemia
Certain genetic predispositions significantly elevate the risk of leukemia. Inherited genetic syndromes, like Down syndrome, can predispose individuals to developing acute lymphoblastic leukemia (ALL). Exposure to ionizing radiation, such as from medical treatments or environmental disasters, has been linked to an increased risk of leukemia. Exposure to certain chemicals, including benzene, a component in some industrial solvents, is also associated with an elevated risk.
While leukemia and lymphoma are both cancers affecting the blood, they have key differences. Leukemia involves the abnormal production of white blood cells, often in the bone marrow. Lymphoma, on the other hand, is a cancer of the lymphatic system, affecting the lymph nodes and other tissues. Understanding these distinctions is crucial for diagnosis and treatment. This understanding, like knowing the difference between systolic and diastolic blood pressure, is vital for navigating complex medical situations.
For a detailed look at blood pressure, check out this resource on systolic and diastolic blood pressure. Ultimately, accurate identification of the type of blood cancer is essential for the most effective treatment plan.
Individuals with a family history of leukemia might have a slightly higher likelihood of developing the disease, although this correlation isn’t always clear-cut. The exact mechanism behind the association with these factors is often complex and not completely understood.
Potential Risk Factors for Lymphoma
A variety of factors can contribute to lymphoma development. Weakened immune systems, as seen in individuals with HIV/AIDS, can increase the risk of lymphoma. Exposure to certain infections, particularly Epstein-Barr virus (EBV) and human immunodeficiency virus (HIV), are often linked to specific lymphoma types. Previous chemotherapy or radiation treatments for other cancers also increase the risk of secondary lymphoma.
Genetic predispositions play a role, with certain syndromes correlating with higher risks. Exposure to environmental carcinogens, while not as definitive as with leukemia, might increase the risk.
Comparison of Risk Factors
While some risk factors overlap, key differences exist. Genetic predisposition is a notable factor in both, but the specific genetic conditions differ. Exposure to ionizing radiation and certain chemicals is more strongly linked to leukemia. Weakened immune systems and specific infections are more strongly linked to lymphoma. The role of environmental factors in both conditions remains an active area of research.
Preventive Measures
Preventive measures, though not guaranteed to eliminate the risk entirely, can significantly reduce the chance of developing either leukemia or lymphoma. There’s no proven method to entirely eliminate risk, but maintaining a healthy lifestyle can mitigate potential factors. Lifestyle choices that support a strong immune system are crucial.
Lifestyle Choices to Potentially Lower Risk
- Maintaining a healthy weight through a balanced diet and regular exercise can support a robust immune system, potentially reducing the risk of various cancers, including leukemia and lymphoma.
- A diet rich in fruits and vegetables provides essential nutrients that support overall health and immune function, potentially reducing the risk of cancer.
- Avoiding tobacco use is crucial. Smoking significantly increases the risk of many cancers, including leukemia and lymphoma.
- Protecting oneself from excessive exposure to sunlight, using sunscreen, and wearing protective clothing can help minimize the risk of skin damage and associated cancers.
- Regular check-ups with healthcare providers are essential. Early detection and prompt medical attention can be critical in managing and potentially preventing various health conditions.
Cellular and Molecular Differences
Leukemia and lymphoma, while both blood cancers, originate from different cell types and exhibit distinct genetic alterations. Understanding these cellular and molecular distinctions is crucial for accurate diagnosis and tailored treatment strategies. This deeper dive into the cellular and molecular landscapes of these cancers will highlight the intricacies of their development.
Cellular Origin of Leukemia and Lymphoma
Leukemias arise from hematopoietic stem cells in the bone marrow, the cellular factories of the body. These stem cells give rise to all types of blood cells. When a hematopoietic stem cell undergoes uncontrolled proliferation and differentiation, leukemia develops. In contrast, lymphomas stem from lymphocytes, a type of white blood cell that plays a critical role in the immune system.
Lymphocytes reside in various lymphoid tissues throughout the body, including lymph nodes, spleen, and tonsils. When lymphocytes become cancerous, lymphoma emerges.
Genetic Alterations in Leukemia and Lymphoma
Genetic alterations are fundamental drivers of both leukemia and lymphoma. These alterations can involve various mechanisms, such as mutations, chromosomal translocations, and epigenetic modifications. Mutations in genes that regulate cell growth, differentiation, and apoptosis (programmed cell death) often contribute to the development of these cancers. Chromosomal translocations, where segments of chromosomes swap places, can create fusion genes that drive abnormal cell behavior.
Epigenetic modifications alter gene expression without changing the DNA sequence itself, further contributing to the cancerous phenotype.
Molecular Pathways Disrupted in Leukemia and Lymphoma
The disruption of various molecular pathways underlies the development of both leukemia and lymphoma. These pathways are complex networks of interactions among genes, proteins, and other molecules that regulate cellular processes. In leukemia and lymphoma, specific pathways, such as the Wnt, Notch, and JAK-STAT pathways, are frequently dysregulated. Dysregulation can result from genetic alterations or epigenetic changes.
This disruption can lead to uncontrolled cell proliferation, impaired differentiation, and resistance to apoptosis, all key hallmarks of cancer.
Cellular Origin Comparison
| Cell Type | Leukemia | Lymphoma |
|---|---|---|
| Hematopoietic stem cells | Origin | Not involved |
| Lymphocytes | Not involved | Origin |
This table summarizes the cellular origins of leukemia and lymphoma. Leukemia originates from hematopoietic stem cells, while lymphoma originates from lymphocytes. This fundamental difference in cellular origin is crucial for distinguishing between these two types of blood cancers.
Examples of Genetic Mutations
Numerous genetic mutations are implicated in leukemia and lymphoma development. One well-known example in leukemia is the Philadelphia chromosome, a reciprocal translocation between chromosomes 9 and 22, which results in the BCR-ABL fusion gene. This fusion gene produces an oncoprotein that drives uncontrolled cell growth. In lymphoma, specific translocations, like the t(8;14) translocation associated with Burkitt lymphoma, are often seen.
These translocations create fusion genes that activate oncogenes and disrupt normal cellular regulation. Furthermore, mutations in genes like TP53, a tumor suppressor gene, can contribute to both leukemia and lymphoma, highlighting the role of these genes in maintaining cellular integrity.
Summary
/leukemia-myeloid-250x-at-35mm-this-type-of-leukemia-has-its-origin-in-the-bone-marrow-myeloid-tissue-it-involves-a-malignant-proliferation-of-immature-white-blood-cells-this-action-can-crowd-out-production-of-rbc-s-and-platelets-leading-to-an--58aca68c3df78c345b81d051.jpg?w=700)
In summary, leukemia and lymphoma, despite both being blood cancers, manifest with distinct cellular origins, symptoms, and treatment protocols. Their different cellular origins and distinct symptoms allow for separate diagnostic approaches, and varied treatment options. Recognizing these differences is paramount for accurate diagnosis and tailored treatment plans, ultimately influencing patient outcomes.