Rectal cancer survival rates are a critical factor for patients and their families. This blog post delves into the intricacies of survival, examining factors like stage at diagnosis, treatment approaches, and even geographical influences. We’ll explore the 5-year survival rates across different stages, discuss the impact of treatment options, and analyze recent advancements in treatment. Understanding these factors is crucial for informed decision-making and hope.
The following sections will provide a detailed breakdown of rectal cancer survival rates, covering various aspects from the general overview to specific treatment strategies and patient experiences. We will present data in a clear and accessible format, making complex information easier to grasp. Expect tables and graphs to help visualize the data, making it more understandable.
Overview of Rectal Cancer Survival Rates
Rectal cancer, while treatable, requires a nuanced understanding of survival rates. These rates are not a simple statistic; they’re influenced by various factors, making it crucial to consider the complexities behind the numbers. A thorough comprehension of these factors allows for a more informed perspective on the prognosis and potential outcomes for those affected by this disease.Understanding survival rates provides a valuable framework for patients, their families, and healthcare professionals.
The knowledge of how factors like stage at diagnosis and treatment approach impact survival can empower patients to make informed decisions and guide healthcare providers in developing tailored treatment plans.
Factors Influencing Survival Rates
Survival rates for rectal cancer are significantly influenced by the stage of the cancer at diagnosis. Early detection and treatment are crucial, as the cancer’s spread directly impacts the likelihood of successful treatment. The type of treatment also plays a critical role. Advanced treatment modalities, including surgery, chemotherapy, and radiation therapy, are often combined to optimize outcomes.
Individual responses to treatment vary, and the effectiveness of these approaches depends on various patient-specific factors.
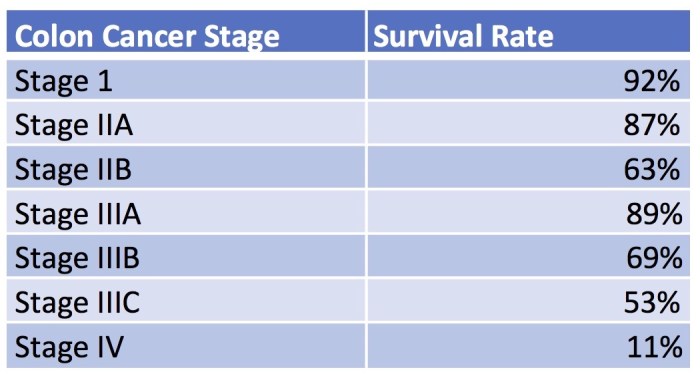
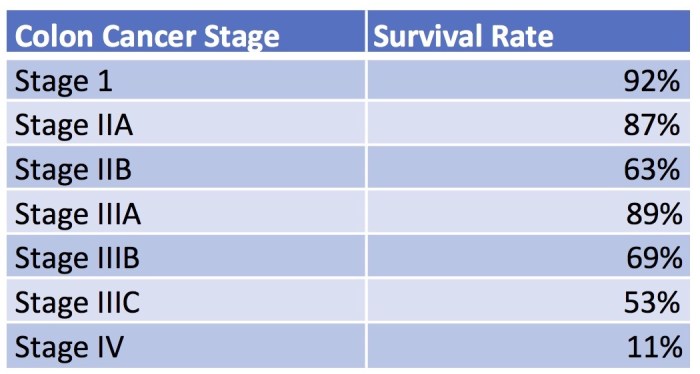
Five-Year Survival Rates by Stage
The five-year survival rate is a common metric used to assess the long-term outcome of cancer treatment. It represents the proportion of patients who are still alive five years after their diagnosis. A higher five-year survival rate generally indicates a better chance of long-term survival. The table below illustrates the varying survival rates across different stages of rectal cancer.
| Stage | Five-Year Survival Rate (Approximate) |
|---|---|
| Stage 0 | 90-95% |
| Stage I | 80-85% |
| Stage II | 70-75% |
| Stage III | 50-60% |
| Stage IV | 10-20% |
Note: These are approximate figures and can vary depending on the specific treatment plan and other individual factors.
Factors Affecting Survival
Rectal cancer, while treatable, presents a complex interplay of factors influencing survival outcomes. Understanding these factors is crucial for both patients and healthcare professionals in developing personalized treatment strategies and improving overall prognoses. The journey towards successful outcomes hinges on early detection, effective treatment protocols, and consideration of patient-specific characteristics.The fight against rectal cancer requires a multi-faceted approach, encompassing not only the biological aspects of the disease but also the individual circumstances of the patient.
Factors like age, socioeconomic status, and access to quality healthcare can significantly impact a patient’s ability to receive timely and appropriate treatment. This, in turn, directly affects their chances of survival and quality of life.
Impact of Early Detection
Early detection of rectal cancer is paramount for improved survival rates. The earlier the diagnosis, the more likely the cancer is to be confined to the local area, making surgical removal a viable option. Furthermore, less extensive treatment may be required, potentially minimizing side effects and improving the patient’s overall well-being. For instance, a patient diagnosed with early-stage rectal cancer may require only surgery, whereas a patient with advanced-stage disease might need a combination of surgery, chemotherapy, and radiation therapy.
Rectal cancer survival rates are definitely encouraging these days, but understanding the nuances of different treatment approaches is key. For instance, exploring the distinctions between naturopath and naturopathic doctor roles can offer valuable insights into holistic healthcare options, and how these might impact long-term outcomes. Knowing the naturopath naturopathic doctor differences could lead to more informed decisions when navigating the complex landscape of cancer care.
Ultimately, a deeper understanding of all available treatment options can contribute to more favorable survival rates for those facing this challenge.
Role of Treatment Modalities
Treatment modalities play a significant role in influencing survival outcomes. Surgery, chemotherapy, and radiation therapy are frequently used in conjunction or individually to address rectal cancer. Surgical resection, aimed at removing the cancerous tissue, is often the initial approach. Chemotherapy, a systemic treatment, targets cancer cells throughout the body, while radiation therapy aims to destroy cancer cells in specific areas.
The choice and combination of these treatments are determined by factors such as the stage of the cancer, the patient’s overall health, and potential side effects.
Influence of Patient Demographics
Patient demographics, including age, socioeconomic status, and access to healthcare, can impact survival rates. Younger patients, for example, often have better overall health and may respond more favorably to treatment, compared to older patients. Socioeconomic status can influence access to quality healthcare, including timely diagnosis and appropriate treatment. Patients with limited access to healthcare may face delays in diagnosis and treatment, which can negatively impact survival.
Access to quality care, including experienced surgeons, oncologists, and support staff, is also crucial. In some cases, socioeconomic status may also affect adherence to treatment plans.
Comparative Effectiveness of Treatment Protocols
Different treatment protocols can yield varying outcomes. A structured comparison is challenging due to numerous variables, but general trends are observed. The effectiveness of a protocol depends on factors such as the specific type of rectal cancer, the patient’s general health, and the quality of the treatment provided.
| Treatment Protocol | Description | Potential Impact on Survival |
|---|---|---|
| Surgery alone | Surgical removal of the tumor. | Generally effective for early-stage cancers, potentially leading to higher survival rates. |
| Surgery + Chemotherapy | Surgical removal followed by systemic chemotherapy. | Often used for more advanced cancers, offering a greater chance of tumor eradication. |
| Surgery + Radiation | Surgical removal combined with radiation therapy. | Used to eliminate any remaining cancer cells after surgery. |
| Surgery + Chemotherapy + Radiation | Combination approach targeting cancer cells throughout the body and in the localized area. | Usually reserved for advanced stages, offering the highest chance of eradication. |
Survival Rates by Stage: Rectal Cancer Survival Rates
Understanding rectal cancer survival rates is crucial for patients and their families. Knowing the likelihood of long-term survival, and how that likelihood changes based on the stage of the cancer, allows for informed decision-making about treatment options and expectations. It’s important to remember that these are general trends, and individual outcomes can vary significantly.Rectal cancer, like many cancers, is often categorized into stages, reflecting the extent of the disease.
Each stage represents a different level of tumor growth and spread. The 5-year survival rate, a common measure, indicates the percentage of patients who are alive five years after diagnosis. Factors like the stage of the cancer, the patient’s overall health, and the effectiveness of treatment all play a role in determining this rate.
5-Year Survival Rates for Rectal Cancer
The 5-year survival rate for rectal cancer patients varies significantly depending on the stage at diagnosis. These rates are based on statistical analysis of large patient populations and represent probabilities, not guarantees. Variations in individual outcomes are possible.
| Stage | 5-Year Survival Rate (%) | Typical Treatment Protocols |
|---|---|---|
| I | 90-95 | Surgery is often the primary treatment. Radiation therapy or chemotherapy may be used adjunctively to reduce the risk of recurrence. |
| II | 70-85 | Surgery is usually the first-line treatment. Radiation therapy and chemotherapy are commonly used, either before or after surgery, to improve the chances of cure. The specifics depend on the exact characteristics of the tumor. |
| III | 50-70 | Surgery is generally the initial treatment. Often, chemotherapy and radiation therapy are administered before or after surgery to reduce the chance of cancer recurrence. The precise combination of therapies will be determined by factors such as the size and location of the tumor. |
| IV | 10-30 | Surgery may be an option if the cancer is localized, but chemotherapy and radiation therapy are typically the primary treatments. Targeted therapies may also be used, often in combination with chemotherapy. Treatment focuses on managing symptoms and prolonging life. |
Comparison of Survival Trajectories
The survival trajectories for rectal cancer patients diagnosed at different stages demonstrate a clear correlation between the stage and prognosis. Patients diagnosed at earlier stages (I and II) have significantly higher 5-year survival rates compared to those diagnosed at later stages (III and IV). This is largely due to the extent of the cancer’s spread and the associated challenges in treatment.Stage I rectal cancer, with its localized nature, typically responds well to surgery, often resulting in high 5-year survival rates.
In contrast, Stage IV rectal cancer, characterized by widespread metastasis, presents more significant treatment challenges and lower survival rates. The treatment approaches for each stage reflect these differences in the extent of the disease. Early detection and prompt treatment are crucial factors in improving survival rates across all stages.
Treatment and Survival Outcomes
Rectal cancer treatment involves a multifaceted approach tailored to the specific stage and characteristics of the tumor. The goal is to eradicate the cancer while minimizing harm to the patient. Effective treatment often combines different modalities, each with its own strengths and potential side effects. Understanding these options is crucial for informed decision-making alongside healthcare professionals.The effectiveness of a treatment strategy is often evaluated by its impact on survival rates.
While complete eradication is the ultimate goal, achieving prolonged survival with an acceptable quality of life is also highly valued. Factors beyond the treatment itself, such as the patient’s overall health and adherence to the treatment plan, also influence the outcome. A combination of therapies may prove more effective than any single approach.
Treatment Options for Rectal Cancer
Various treatment options are available for rectal cancer, ranging from surgery to radiation therapy and chemotherapy. The choice of treatment is typically based on the stage and location of the tumor, the patient’s overall health, and preferences.
Rectal cancer survival rates are definitely a concern, but it’s important to remember that proactive health choices can play a huge role. For example, exploring natural treatments for conditions like ankylosing spondylitis, like those discussed in this article about ankylosing spondylitis natural treatment , could potentially improve overall well-being and, consequently, impact related health outcomes. Ultimately, understanding various health approaches is crucial when considering factors that affect rectal cancer survival rates.
- Surgery is often the primary treatment for rectal cancer, involving the removal of the tumor and surrounding tissues. Different surgical approaches, such as laparoscopic or robotic surgery, may be considered based on the specific circumstances. The extent of the surgery can vary, depending on the location and size of the tumor.
- Radiation therapy uses high-energy rays to damage cancer cells. It can be used before or after surgery to shrink the tumor or to reduce the risk of recurrence. External beam radiation therapy is a common method, focusing radiation beams on the affected area. Internal radiation therapy (brachytherapy) involves placing radioactive material directly into the tumor.
- Chemotherapy uses drugs to kill cancer cells. It can be administered before, during, or after surgery or radiation therapy. Various chemotherapy regimens are available, and the choice depends on the specific type of rectal cancer and the patient’s response to treatment.
Effectiveness of Treatment Combinations
The combination of different treatments often leads to better outcomes than using a single approach. For example, preoperative chemotherapy followed by surgery may reduce the tumor size, making surgical removal easier and potentially improving long-term survival. Postoperative radiation therapy can further decrease the risk of recurrence in certain cases.
- Combining chemotherapy and radiation therapy can enhance the effectiveness of both treatments, resulting in a higher response rate and better survival outcomes.
- Targeted therapies, which focus on specific molecular targets within cancer cells, are increasingly used in combination with other treatments. These treatments aim to enhance the effectiveness of standard treatments and improve the quality of life for patients.
Treatment Strategies and Survival Rates
A direct comparison of survival rates across different treatment strategies is complex and requires careful consideration of multiple factors. The data below provides a general overview of the potential effectiveness of different approaches. Note that these figures represent averages and individual outcomes can vary significantly.
| Treatment Strategy | Potential Survival Outcomes (Approximate, in years) | Factors Affecting Outcomes |
|---|---|---|
| Surgery alone | 5-10 years | Tumor stage, size, location, patient’s overall health |
| Surgery + Preoperative Chemotherapy | 7-15 years | Tumor stage, response to chemotherapy, patient’s overall health |
| Surgery + Postoperative Radiation Therapy | 6-12 years | Tumor stage, response to radiation, patient’s overall health |
| Surgery + Chemotherapy + Radiation | 8-15 years | Tumor stage, response to treatments, patient’s overall health |
Impact on Long-Term Survival Prospects, Rectal cancer survival rates
The choice of treatment strategy significantly impacts long-term survival prospects. Patients with early-stage rectal cancer often have a higher chance of long-term survival with a single modality of treatment, such as surgery. More advanced stages may require a combination of therapies for optimal outcomes. Patients should discuss their individual treatment plan and potential survival outcomes with their healthcare team.
Recent Trends and Advancements
Rectal cancer, while a serious illness, is increasingly treatable thanks to ongoing advancements in medical science. New therapies and technologies are significantly impacting survival rates and quality of life for patients. This section explores the most recent breakthroughs and their implications for improved outcomes.Rectal cancer treatment is constantly evolving, with researchers continually refining existing methods and developing innovative approaches.
Targeted therapies, for instance, are demonstrating promising results in specific patient populations, while new surgical techniques and radiation therapies are improving precision and minimizing side effects.
Advancements in Surgical Techniques
Surgical procedures for rectal cancer have seen significant improvements. Minimally invasive techniques, like laparoscopic surgery and robotic surgery, are becoming more commonplace. These procedures offer several advantages, including reduced pain, shorter hospital stays, and faster recovery times. The enhanced precision of these techniques allows surgeons to remove tumors more effectively while preserving healthy tissue, leading to better long-term outcomes for patients.
Minimally invasive surgery also reduces the risk of infection and complications associated with traditional open surgery.
Targeted Therapies and Their Impact
Targeted therapies are revolutionizing the treatment landscape for various cancers, including rectal cancer. These therapies focus on specific molecular targets within cancer cells, disrupting their growth and survival pathways. While not a universal solution, targeted therapies show promise in specific subtypes of rectal cancer, particularly those with certain genetic mutations. Their efficacy is often evaluated in clinical trials, and their use is frequently combined with other therapies to maximize effectiveness.
Rectal cancer survival rates are improving thanks to advancements in treatment. However, understanding factors like hormone imbalances, such as those associated with androgens and PCOS excess levels, androgens and pcos excess levels what it means , could potentially offer further insights into improving these rates. This is a fascinating area of research that could ultimately lead to more effective prevention and treatment strategies for rectal cancer.
Emerging Research Areas
Several research areas hold significant potential for improving rectal cancer survival. One promising area is the development of personalized therapies tailored to the unique genetic characteristics of each patient’s tumor. Researchers are also investigating the use of immunotherapy to boost the body’s own immune response against cancer cells. The exploration of novel drug combinations and the development of more accurate diagnostic tools also hold considerable potential.
These advancements aim to enhance treatment effectiveness, reduce side effects, and improve overall patient outcomes.
Impact of New Technologies
New technologies are impacting rectal cancer treatment in several ways. Advanced imaging techniques, such as MRI and PET scans, provide detailed information about the tumor’s location, size, and extent, enabling more precise surgical planning and treatment strategies. Furthermore, advancements in radiation therapy, like intensity-modulated radiation therapy (IMRT), allow for more targeted delivery of radiation, reducing damage to surrounding healthy tissues.
These technological improvements are pivotal in achieving higher cure rates and preserving quality of life.
Survival Rates Over Time
Rectal cancer survival rates have significantly improved over the past few decades. This progress reflects advancements in early detection, surgical techniques, and chemotherapy regimens. Understanding the historical trends provides valuable context for evaluating current survival rates and projecting future progress.Improvements in diagnostic tools, screening practices, and patient awareness have led to earlier detection of rectal cancer. This earlier diagnosis often translates to a more favorable prognosis, as tumors are typically smaller and less likely to have spread at the time of diagnosis.
This crucial factor is one of the drivers behind the increase in survival rates.
Historical Context of Rectal Cancer Survival
Prior to the mid-20th century, rectal cancer survival rates were considerably lower. Limited treatment options, including surgical resection alone, often resulted in poor outcomes. The disease was frequently diagnosed at advanced stages, making effective treatment challenging. Radiation therapy and chemotherapy were still in their nascent stages of development and application.
Factors Contributing to Improved Survival
The increase in survival rates is largely attributed to a combination of factors. Improved diagnostic techniques, such as colonoscopies and advanced imaging, have enabled earlier detection, leading to earlier intervention.
- Enhanced Treatment Modalities: The development and refinement of surgical procedures, including minimally invasive techniques, have improved surgical outcomes. The addition of chemotherapy and targeted therapies to the treatment arsenal has dramatically increased treatment effectiveness.
- Improved Patient Care: Enhanced patient support systems, including access to specialized care teams and palliative care, have played a significant role in improving overall quality of life and outcomes.
Evolution of Treatment Strategies
The evolution of treatment strategies for rectal cancer has been a cornerstone of the improved survival rates. Surgical approaches have transitioned from extensive resections to less invasive procedures, minimizing trauma and improving recovery times.
- Targeted Therapies: Targeted therapies have emerged as a powerful tool for treating rectal cancer, specifically targeting the molecular pathways that drive tumor growth. This has led to a significant improvement in treatment response, particularly in advanced or metastatic disease.
- Combination Therapies: The use of combination therapies, such as chemotherapy combined with radiation or surgery, has demonstrated improved outcomes compared to single-agent treatments.
Trends in Survival Rates
A graph depicting the change in rectal cancer survival rates over time would show a clear upward trend. The x-axis would represent the year, and the y-axis would represent the survival rate (e.g., 5-year survival rate). The graph would visually illustrate the increasing survival rates, indicating the positive impact of advancements in diagnosis and treatment. Data from various studies and clinical trials would be used to construct the graph.
For example, a graph showing a 5-year survival rate of 50% in the 1970s rising to 70% or higher in the 2020s would clearly illustrate the improvement.
Survival Rates by Geographic Location
Rectal cancer survival rates vary significantly across the globe. Factors such as access to advanced medical care, screening programs, and overall healthcare infrastructure play a crucial role in determining outcomes. This disparity highlights the need for global initiatives to improve access to effective treatments and preventative measures.
Geographic Variations in Survival
Differences in survival rates for rectal cancer are evident when comparing developed and developing nations. This disparity is often attributed to variations in access to early detection, advanced treatment options, and overall healthcare quality. Access to sophisticated diagnostic tools, experienced surgical teams, and comprehensive chemotherapy regimens are often more readily available in developed countries, which can directly impact survival probabilities.
Developed vs. Developing Countries
Survival rates for rectal cancer in developed countries tend to be higher compared to those in developing countries. This difference is a complex issue with numerous contributing factors. These include the availability of advanced diagnostic techniques, the quality of surgical procedures, the accessibility of sophisticated chemotherapy regimens, and the promptness of treatment initiation. Furthermore, factors like socioeconomic status and access to nutrition can influence the patient’s overall well-being and response to treatment.
Potential Reasons for Disparities
Several factors contribute to the variations in rectal cancer survival rates across geographical regions. Differences in healthcare infrastructure, access to advanced medical technologies, and socioeconomic disparities are major contributors. Early detection rates are often lower in regions with limited access to screening programs and healthcare resources. This delayed diagnosis can significantly impact the effectiveness of treatment and ultimately, survival outcomes.
Table of Survival Rates by Region
| Region | Estimated 5-Year Survival Rate | Notes |
|---|---|---|
| North America | 60-70% | High access to advanced care, screening programs, and treatment options. |
| Western Europe | 65-75% | Similar to North America in terms of healthcare infrastructure and resources. |
| East Asia | 50-60% | Varying access to advanced care; some regions show improvements. |
| South Asia | 40-50% | Limited access to advanced care and diagnostic tools. |
| Sub-Saharan Africa | 30-40% | Lowest survival rates due to limited resources and access to treatment. |
Note: These figures are estimates and can vary based on specific stage of diagnosis, treatment approaches, and other individual patient factors.
Patient Experience and Quality of Life
Facing a rectal cancer diagnosis is undoubtedly a challenging experience. Beyond the medical treatments, patients confront a complex interplay of physical, emotional, and social adjustments. Understanding how survival rates intersect with quality of life, the impact of treatment, and the crucial role of support systems is essential for holistic patient care.The experience of rectal cancer, encompassing diagnosis, treatment, and recovery, significantly influences a patient’s overall well-being.
This extends beyond mere survival statistics; it encompasses the ability to maintain a fulfilling life, engage in desired activities, and manage potential side effects. Ultimately, a patient’s quality of life is a multifaceted concept deeply intertwined with the course of their disease and the available support structures.
Impact of Survival Rates on Quality of Life
Survival rates, while crucial indicators of progress in cancer treatment, don’t fully capture the richness of the patient experience. A longer survival time, though desirable, doesn’t automatically translate to an improved quality of life. Factors such as the severity of the disease, the effectiveness of treatment, and the individual’s resilience play a significant role. Patients with longer survival times may experience lingering physical and emotional side effects, potentially impacting their ability to work, socialize, and participate in activities they once enjoyed.
For example, a patient achieving a five-year survival may still struggle with fatigue, digestive issues, or body image concerns.
Impact of Treatment on Quality of Life
Rectal cancer treatments, while vital for survival, can also have significant consequences on a patient’s quality of life. Chemotherapy, radiation, and surgery can cause fatigue, nausea, loss of appetite, and bowel or bladder dysfunction. These side effects can significantly impact a patient’s ability to perform daily tasks, maintain relationships, and enjoy life’s simple pleasures. Furthermore, the psychological toll of these treatments, such as anxiety, fear, and depression, is often overlooked but must be addressed.
Support groups and counseling can play a critical role in mitigating these challenges.
Psychosocial Effects of Diagnosis and Treatment
The diagnosis and treatment of rectal cancer trigger a cascade of psychosocial effects. Anxiety, fear, and depression are common responses to the diagnosis, often accompanied by feelings of isolation and uncertainty about the future. The physical changes resulting from surgery can also lead to body image concerns and a loss of self-esteem. Patients may also grapple with the emotional burden of discussing their condition with loved ones and adjusting to potential changes in their relationships.
Role of Support Systems in Improving Quality of Life
Strong support systems are vital in enhancing the quality of life for rectal cancer patients. These systems can encompass family, friends, support groups, and healthcare professionals. Family and friends can provide emotional support, practical assistance, and a sense of belonging. Support groups offer a safe space for sharing experiences, coping mechanisms, and providing mutual encouragement. Healthcare professionals, including oncologists, nurses, and social workers, play a critical role in guiding patients through the treatment process, addressing their emotional needs, and providing access to resources.
These support systems help patients navigate the challenges of the disease and treatment, improving their emotional well-being and overall quality of life.
Outcome Summary
In conclusion, rectal cancer survival rates are a multifaceted issue, significantly influenced by various factors. Early detection, effective treatment, and ongoing research play pivotal roles. The data presented here highlights the importance of personalized approaches and emphasizes the ongoing need for advancements in treatment and support systems. Understanding these survival rates empowers patients and their families to make informed decisions, and fosters a sense of hope and resilience.