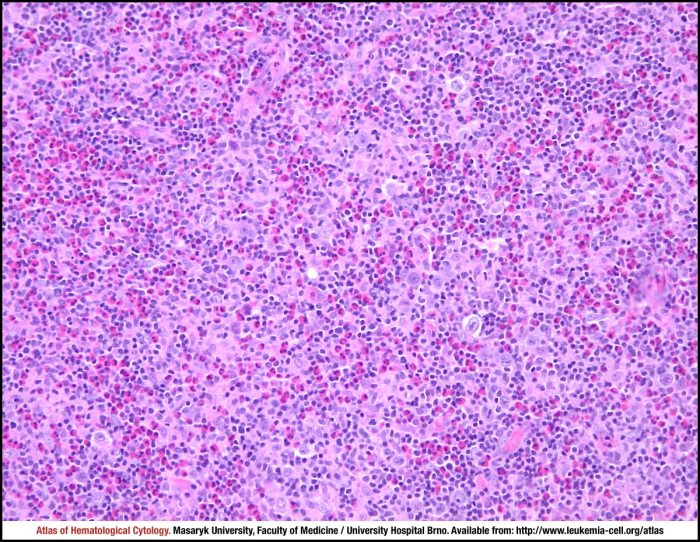
Mixed cellularity hodgkins lymphoma – Mixed cellularity Hodgkin lymphoma (MCHL) is a type of blood cancer that requires careful understanding. It’s characterized by the presence of specific abnormal cells, called Reed-Sternberg cells, and other unique histological features. Diagnosing and treating MCHL involves a multifaceted approach, encompassing various diagnostic procedures, treatment strategies, and considerations of prognosis…
Tag: cancer
Overview of Chronic Myeloid Leukemia A Comprehensive Look
Overview of chronic myeloid leukemia is a complex blood cancer, and understanding its intricacies is crucial for those affected and those seeking to learn more. This introduction will explore the various facets of CML, from its defining characteristics and underlying pathophysiology to the available treatment strategies and future research directions. Chronic myeloid leukemia (CML) is…
CLL When to Treat A Comprehensive Guide
CLL when to treat is a crucial question for patients and healthcare providers alike. This in-depth exploration delves into the complexities of chronic lymphocytic leukemia (CLL), examining the factors that influence treatment decisions, from patient characteristics to genetic mutations. We’ll explore the various treatment options available, their effectiveness, and potential side effects, ultimately providing a…
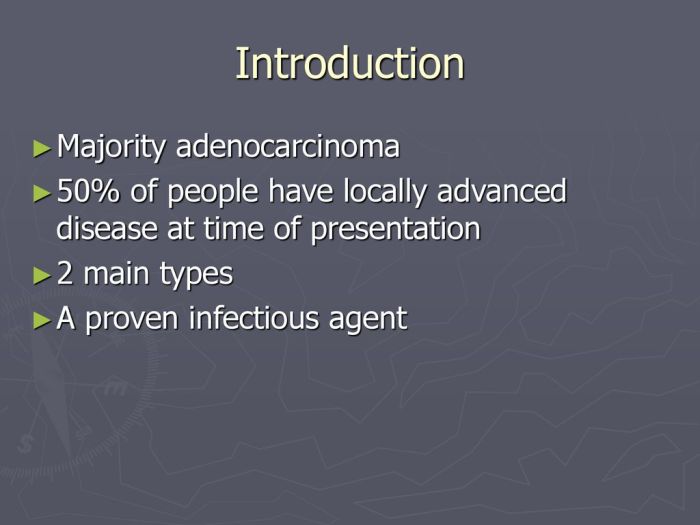
Metastatic Adenocarcinoma Overview and More
Metastatic adenocarcinoma overview and more delves into the complexities of this aggressive cancer. We’ll explore its defining characteristics, the often-devastating journey of diagnosis and treatment, and the vital support systems available for patients and families. From understanding the different stages to examining treatment options and prognosis, this comprehensive guide aims to equip readers with a…
What is the Most Common Cancer in the US?
What is the most common cancer in the US? This crucial question delves into the leading causes of cancer, highlighting the factors that influence its prevalence. We’ll explore the key statistics, examining incidence rates, mortality figures, and the role of demographics, lifestyle choices, and environmental factors in shaping these trends. Understanding the most common cancer…
What is a Carcinogen Understanding the Dangers
What is a carcinogen? It’s a substance that can cause cancer. This exploration delves into the science behind these harmful compounds, from their various classifications to the long-term health effects they can trigger. We’ll uncover the mechanisms by which carcinogens damage DNA, examine the sources of exposure, and discuss strategies for prevention and mitigation. Understanding…
Hair Dye and Cancer Safety Risks Unveiled
Hair dye and cancer effects hair care safety risks is a complex issue, raising concerns about the potential health consequences of coloring our hair. This deep dive explores the potential hazards, examining the chemicals in dyes, their possible links to cancer, and crucial safety practices to minimize risks. We’ll also look at safer alternatives and…
Do Wireless Bluetooth Headphones Cause Cancer?
Do wireless Bluetooth headphones cause cancer? This question sparks considerable debate, raising concerns about the potential health risks associated with RF radiation emitted by these devices. Understanding the science behind RF radiation, examining existing research, and exploring regulatory standards is crucial to form a balanced perspective on this issue. This exploration delves into the scientific…
The p53 Gene Its Crucial Role in Cancer
The p53 gene its role in cancer – The p53 gene, its role in cancer, is a pivotal area of research, exploring the gene’s intricate function in normal cellular processes and its dramatic impact on cancer development and progression. This gene acts as a crucial guardian, ensuring cellular health and preventing uncontrolled cell growth. Understanding…
New Hair, New Look After Chemo A Guide
New hair new look after chemo – New hair, new look after chemo sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with personal stories. This journey delves into the emotional and practical aspects of embracing a new hairstyle during and after chemotherapy,…