Facts about irritable bowel syndrome: Understanding this common digestive disorder is crucial for effective management. IBS affects millions worldwide, causing a range of uncomfortable symptoms. This guide delves into the complexities of IBS, exploring its types, potential causes, diagnostic methods, treatment options, and lifestyle modifications. We’ll also discuss coping strategies, potential complications, and the latest research in this area.
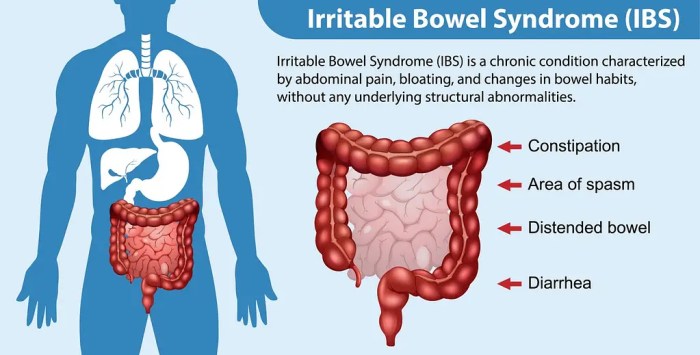
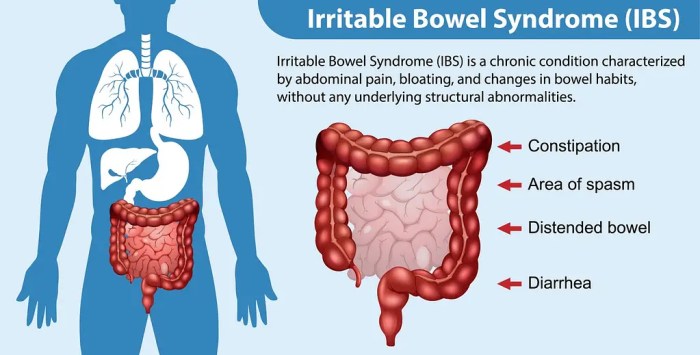
Irritable bowel syndrome (IBS) is a chronic condition that impacts the large intestine. Common symptoms include abdominal pain, bloating, gas, diarrhea, and constipation. Different types of IBS, such as IBS-C (constipation-predominant), IBS-D (diarrhea-predominant), and IBS-M (mixed), exhibit varying symptom profiles. This article will provide a comprehensive overview of the condition, empowering readers with knowledge to better understand and manage their IBS.
Irritable Bowel Syndrome (IBS) Explained
Irritable bowel syndrome (IBS) is a common chronic gastrointestinal disorder affecting the large intestine. It’s characterized by recurring abdominal pain and changes in bowel habits, often accompanied by other symptoms. While the exact cause of IBS remains elusive, various factors, including diet, stress, and gut bacteria, are believed to play a role. Understanding the different types of IBS and their associated symptoms is crucial for effective management and treatment.
Defining Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder, meaning there’s no detectable structural damage to the digestive tract. It’s a complex condition involving disturbances in bowel motility and sensation, leading to a range of symptoms. The hallmark of IBS is recurring abdominal pain or discomfort accompanied by changes in bowel habits.
Did you know that Irritable Bowel Syndrome (IBS) can be tricky to manage? While diet plays a big role, some folks find that swapping out their tea preferences, like comparing black tea vs green tea, black tea vs green tea , might offer some relief. Different types of tea can affect digestion in various ways, so it’s worth exploring potential connections.
Ultimately, understanding the specific facts about IBS is crucial for finding the best solutions for your individual needs.
Common Symptoms of IBS
IBS manifests in a variety of ways, but common symptoms include abdominal pain, bloating, gas, and changes in bowel movements. These symptoms can vary in intensity and frequency from person to person. These symptoms can significantly impact daily life, affecting work, social activities, and overall well-being.
Types of IBS
IBS is broadly categorized into subtypes based on the predominant bowel habit changes. These subtypes include IBS with constipation (IBS-C), IBS with diarrhea (IBS-D), and IBS with mixed bowel habits (IBS-M).
Comparing IBS Subtypes
| IBS Type | Common Symptoms | Other Symptoms (Optional) |
|---|---|---|
| IBS-C | Straining during bowel movements, hard or lumpy stools, feeling like you haven’t completely emptied your bowels, infrequent bowel movements (fewer than 3 per week), feeling of abdominal fullness or bloating. | Feeling of urgency to defecate, abdominal pain that is often relieved by defecation, mucus in the stool. |
| IBS-D | Loose or watery stools, frequent bowel movements (more than 3 per week), urgency to defecate, abdominal pain that is often relieved by bowel movements, bloating, and gas. | Cramps, feeling of incomplete emptying, mucus in the stool. |
| IBS-M | Alternating periods of constipation and diarrhea, experiencing both loose and hard stools, abdominal pain that varies in location and intensity, bloating, gas. | Feeling of abdominal fullness, feeling of urgency to defecate, fatigue, nausea, and headaches. |
Causes and Risk Factors of IBS

Irritable bowel syndrome (IBS) is a complex disorder affecting the digestive system, and while its exact cause remains elusive, various factors contribute to its development and manifestation. Understanding these factors is crucial for developing personalized management strategies and improving the quality of life for those affected. This exploration will delve into potential causes, risk factors, and the interplay of genetics and environment in the context of IBS.The precise mechanisms underlying IBS are not fully understood, but it’s generally believed to involve a combination of factors rather than a single cause.
These factors interact in complex ways, potentially triggering or exacerbating symptoms. This section will illuminate these interwoven aspects.
Potential Causes of IBS
Multiple factors are thought to play a role in the development of IBS. These include:
- Gut Microbiome Imbalance: The gut microbiome, the vast community of microorganisms residing in the digestive tract, plays a crucial role in digestion and overall health. An imbalance in this microbial community, often termed dysbiosis, may contribute to IBS symptoms. For instance, certain types of bacteria may produce compounds that irritate the gut lining, potentially leading to inflammation and pain.
- Food Sensitivities/Intolerances: Certain foods, such as lactose or gluten, can trigger digestive distress in individuals with sensitivities or intolerances. These foods may cause symptoms like bloating, gas, and abdominal pain in susceptible individuals, which could be mistaken for IBS symptoms.
- Stress and Anxiety: Stress and anxiety are recognized as significant triggers for IBS symptoms. The nervous system plays a vital role in gut function, and heightened stress levels can disrupt this balance, leading to increased motility, pain, and other symptoms.
- Infections: Certain infections, such as gastroenteritis, can alter the gut microbiome and potentially contribute to the development or exacerbation of IBS symptoms. These infections can cause inflammation in the gut and lead to symptoms that mimic IBS.
Risk Factors for IBS
Various factors can increase the likelihood of developing IBS. Identifying these risk factors is important for preventive measures and tailored interventions.
- Family History: A family history of IBS can increase an individual’s risk of developing the condition. Genetic predispositions may play a role in this increased susceptibility.
- Previous Gastrointestinal Issues: Experiencing previous gastrointestinal issues, such as infections or surgeries, may increase the risk of developing IBS. These experiences can disrupt the normal functioning of the gut and increase susceptibility to IBS symptoms.
- Stressful Life Events: Significant life stressors, such as job loss, relationship problems, or financial difficulties, can increase the risk of developing or exacerbating IBS symptoms. These stressors can affect the gut-brain axis, contributing to symptoms.
- Dietary Habits: Certain dietary habits, such as a diet high in processed foods or low in fiber, may increase the risk of IBS. This is due to the fact that a balanced diet is important for maintaining a healthy gut microbiome.
Genetics and Environmental Factors in IBS
The interplay of genetics and environmental factors plays a crucial role in the development of IBS. While genetics may predispose an individual to IBS, environmental factors can trigger or exacerbate symptoms.
- Genetic Predisposition: Certain genes may increase the risk of developing IBS. This means that individuals with a family history of IBS may be more susceptible to the condition. However, genetics alone do not determine the development of IBS.
- Environmental Influences: Environmental factors, such as diet, stress, and infections, can interact with genetic predispositions to influence the development and manifestation of IBS. These interactions are often complex and not fully understood.
Table of Risk Factors and Potential Impact
| Risk Factor | Potential Impact | Supporting Evidence (Optional) |
|---|---|---|
| Family history of IBS | Increased susceptibility to developing IBS. | Studies show a correlation between family history and IBS prevalence. |
| Previous gastrointestinal infections | Disruption of gut microbiome, potentially increasing IBS risk. | Evidence suggests infections can alter gut flora and trigger symptoms. |
| Stressful life events | Increased stress hormones can disrupt gut motility and lead to IBS symptoms. | Research indicates a link between psychological stress and IBS exacerbation. |
| Diet high in processed foods/low in fiber | Potential imbalance in gut microbiome and increased risk of digestive discomfort. | Studies suggest a correlation between dietary habits and IBS prevalence. |
Diagnosis and Treatment of IBS
Irritable bowel syndrome (IBS) is a chronic condition that affects the digestive system. Accurate diagnosis and personalized treatment plans are crucial for managing symptoms and improving quality of life. While a cure for IBS isn’t available, effective strategies can significantly reduce discomfort and disruptions to daily life.
Diagnostic Process for IBS
Diagnosing IBS involves a multi-faceted approach, combining medical history, physical examination, and sometimes specific tests. A thorough understanding of the patient’s symptoms, including the frequency, duration, and characteristics of bowel movements, is essential. This information helps to distinguish IBS from other digestive disorders.
Common Methods for Diagnosing IBS
A detailed medical history is the first step in the diagnostic process. The physician will ask about the patient’s symptoms, diet, lifestyle, and any relevant medical conditions. A physical examination will be conducted to rule out other potential causes of abdominal pain and discomfort. In some cases, further investigations may be necessary.
Diagnostic Tests for IBS
Occasionally, further tests may be required to rule out other conditions. These tests may include blood tests to check for infections or other underlying medical problems. In certain situations, stool tests might be conducted to identify any potential infections or abnormalities. Imaging tests, such as X-rays or ultrasounds, are rarely necessary for IBS diagnosis.
Treatment Options for IBS
Effective management of IBS involves a combination of lifestyle modifications and, if necessary, medications. Personalized treatment plans are tailored to individual needs and symptom severity.
Medications Used to Manage IBS
Various medications are used to alleviate IBS symptoms. These include antispasmodics to reduce abdominal cramps, laxatives to address constipation, and antidiarrheal medications to manage diarrhea. Over-the-counter medications, such as probiotics, are sometimes recommended to support gut health. Specific medication choices depend on the predominant symptom pattern (constipation, diarrhea, or mixed).
Therapies Used to Manage IBS
Beyond medication, various therapies can play a significant role in managing IBS symptoms. Dietary modifications are crucial, often focusing on identifying and avoiding trigger foods. Stress management techniques, such as relaxation exercises or mindfulness, can also be helpful. Cognitive behavioral therapy (CBT) can help patients manage their thoughts and feelings related to their symptoms, improving their overall well-being.
Irritable bowel syndrome (IBS) is a common digestive issue, and understanding its various causes and symptoms is key. While IBS often focuses on gut health, it’s interesting to consider how other conditions can impact the body, such as facts about chronic kidney disease. Ultimately, though, it’s important to remember that IBS can significantly impact daily life, and learning more about it can help manage symptoms and improve quality of life.
Treatment Options and Their Potential Effectiveness
| Treatment Option | Description | Potential Benefits | Potential Side Effects |
|---|---|---|---|
| Dietary Modifications | Identifying and avoiding trigger foods, adjusting portion sizes, and adopting a balanced diet. | Reduced symptom frequency and severity, improved overall digestive health. | Potential for nutritional deficiencies if not carefully managed. |
| Antispasmodics | Medications that relax the muscles in the digestive tract, reducing spasms and cramping. | Relief from abdominal pain and cramping. | Drowsiness, dry mouth, and dizziness in some cases. |
| Laxatives | Medications that stimulate bowel movements, addressing constipation. | Relief from constipation and bloating. | Dehydration, abdominal cramping, and dependence in some cases. |
| Antidiarrheal Medications | Medications that slow down bowel movements, addressing diarrhea. | Relief from diarrhea and urgency. | Constipation, bloating, and gas. |
| Probiotics | Live microorganisms, often found in yogurt or supplements, that can improve gut health. | Potential to reduce symptom severity and improve gut balance. | Gas, bloating, and diarrhea in some cases. |
| Stress Management Techniques | Techniques like relaxation exercises, meditation, and mindfulness. | Reduction in stress-related symptoms, improved overall well-being. | No direct side effects, but individual response may vary. |
| Cognitive Behavioral Therapy (CBT) | Therapy that helps identify and change negative thoughts and behaviors related to IBS. | Improved symptom management, enhanced coping mechanisms, and improved overall well-being. | Potential for emotional distress during initial sessions; individual response may vary. |
Lifestyle Modifications for IBS Management
Managing Irritable Bowel Syndrome (IBS) effectively often involves more than just medication. Lifestyle modifications, including dietary adjustments and stress management techniques, play a crucial role in alleviating symptoms and improving overall well-being. These strategies can significantly reduce the frequency and severity of IBS episodes, enabling individuals to lead more fulfilling lives.
Dietary Adjustments for IBS
Dietary changes are fundamental in managing IBS symptoms. Different foods affect individuals differently, and identifying trigger foods is crucial. A personalized approach is key to success. Understanding how specific foods affect your digestive system can help you avoid problematic foods. This requires careful monitoring and attention to how your body responds to various dietary choices.
| Dietary Recommendation | Potential Effect on IBS | Examples |
|---|---|---|
| Reduce or Eliminate Trigger Foods | May decrease abdominal pain, bloating, and diarrhea/constipation | Processed foods, spicy foods, caffeine, alcohol, high-fat foods, and certain fruits (e.g., apples, pears) |
| Increase Fiber Intake Gradually | May improve bowel regularity and reduce constipation or diarrhea | Fruits, vegetables, whole grains, legumes, and oats |
| Consume Smaller, More Frequent Meals | May prevent large fluctuations in gut motility and lessen bloating | Instead of three large meals, have 5-6 smaller meals |
| Hydrate Regularly | Improves digestion and can alleviate constipation. | Water, herbal teas, and clear broths |
| Limit Gas-Producing Foods | May help reduce bloating and discomfort. | Beans, cabbage, broccoli, onions, and carbonated drinks |
Stress Management Techniques for IBS
Stress significantly impacts IBS symptoms. Chronic stress can worsen inflammation and digestive issues. Stress management techniques are not only important for managing IBS but also for overall well-being. Practicing these techniques can help individuals cope with stress effectively.
- Mindfulness and Meditation: Mindfulness practices, such as meditation and deep breathing exercises, help calm the mind and body, reducing stress hormones. Regular practice can help manage anxiety and improve focus.
- Yoga and Tai Chi: These practices combine physical postures and breathing techniques to promote relaxation and reduce stress. They can improve flexibility, balance, and overall physical well-being, indirectly contributing to IBS symptom management.
- Regular Exercise: Physical activity can help reduce stress and improve mood. Even moderate exercise can significantly impact stress levels and contribute to better overall health.
- Sufficient Sleep: Adequate sleep is essential for overall health and well-being. It helps regulate the body’s stress response and can improve the body’s ability to cope with digestive issues. Aim for 7-9 hours of quality sleep each night.
- Time Management and Prioritization: Effective time management can reduce feelings of overwhelm and stress. Prioritizing tasks and setting realistic goals can reduce stress and improve overall well-being.
Living with IBS
Navigating Irritable Bowel Syndrome (IBS) can be challenging, but with the right strategies, individuals can significantly improve their quality of life and effectively manage symptoms. Understanding the nuances of coping mechanisms, building a strong support system, and prioritizing emotional well-being are crucial components in this journey. This section delves into practical techniques and available resources to empower those living with IBS.Living with IBS involves a multifaceted approach that goes beyond simply treating symptoms.
It necessitates a holistic understanding of the condition and proactive strategies to improve overall well-being. By addressing emotional aspects, fostering strong support systems, and implementing practical coping mechanisms, individuals can actively manage their IBS and reclaim a fulfilling life.
Improving Quality of Life
Effective management of IBS extends beyond medication and dietary changes. Individuals can actively enhance their quality of life by integrating lifestyle modifications and mental health strategies. This includes regular exercise, stress reduction techniques, and maintaining a balanced diet.
Importance of Support Systems
Having a strong support system is invaluable for individuals living with IBS. This encompasses family, friends, support groups, and healthcare professionals. Sharing experiences, receiving empathy, and gaining practical advice from others who understand the challenges can significantly reduce feelings of isolation and provide invaluable encouragement. This support network provides emotional validation and practical solutions, fostering a sense of community and shared understanding.
Did you know that irritable bowel syndrome (IBS) can sometimes manifest with unusual muscle spasms in the gut? Understanding the interplay between the digestive system and the musculoskeletal system, like the musculoskeletal system what is it , is crucial to comprehending the full picture of IBS. While the exact mechanisms are still being explored, the connection between these two systems highlights the complexity of this condition and the importance of a holistic approach to managing it.
Practical Coping Strategies
Managing IBS symptoms effectively requires practical coping strategies. These include identifying triggers, practicing relaxation techniques, and maintaining a consistent routine. Identifying specific dietary triggers and adjusting the diet accordingly can significantly alleviate symptoms. Regular exercise, relaxation techniques like deep breathing or meditation, and consistent sleep patterns can also mitigate stress, which often exacerbates IBS symptoms. Time management and prioritizing tasks can reduce stress and improve overall well-being.
Emotional Well-being, Facts about irritable bowel syndrome
Emotional well-being plays a pivotal role in managing IBS. Stress, anxiety, and depression can exacerbate symptoms. Strategies to manage emotional well-being include mindfulness practices, cognitive behavioral therapy (CBT), and stress-reduction techniques. These methods can equip individuals with tools to manage stress and improve their emotional response to IBS symptoms, leading to a more balanced and positive outlook on life.
Resources and Support Groups
Numerous resources and support groups are available to help individuals cope with IBS. Connecting with others who share similar experiences can provide validation, encouragement, and practical tips. Online forums, support groups, and local organizations offer valuable platforms for sharing experiences, receiving advice, and building a sense of community.
Table of IBS Support Resources
| Resource Type | Description | Contact Information (Optional) |
|---|---|---|
| National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) | Provides information and resources on IBS, including research updates and clinical trials. | https://www.niddk.nih.gov/ |
| The IBS Network | Offers support groups, educational materials, and a community forum for individuals with IBS. | https://www.ibsnetwork.org/ |
| American Gastroenterological Association (AGA) | Provides information on digestive health, including IBS, and connects individuals with gastroenterologists. | https://www.gastro.org/ |
| Local Support Groups | Many local organizations and community centers offer support groups for individuals with chronic conditions, including IBS. | Search online for “IBS support groups” + your city/region. |
Potential Complications and Long-Term Considerations
Living with irritable bowel syndrome (IBS) can be challenging, but understanding potential complications and adopting proactive long-term management strategies can significantly improve quality of life. This section delves into the possible complications of IBS, emphasizing the importance of ongoing care and preventive measures. A proactive approach to IBS management, encompassing lifestyle changes and medical interventions, is key to minimizing potential long-term issues.
Potential Complications of IBS
IBS, while often manageable, can sometimes lead to complications if not properly addressed. These complications can range from exacerbating existing symptoms to developing new health concerns. Careful monitoring and appropriate medical interventions are crucial for managing these complications effectively.
Importance of Long-Term Management
Consistent management of IBS is vital for preventing potential complications and maintaining overall well-being. Long-term strategies should focus on symptom control, dietary adjustments, stress management, and regular medical check-ups. By proactively addressing IBS, individuals can minimize the risk of more serious health issues arising from the condition.
Factors to Consider for Preventing Complications
Several factors contribute to the prevention of complications related to IBS. Maintaining a balanced diet low in trigger foods, managing stress effectively, and engaging in regular physical activity are key components. Regular communication with healthcare providers, seeking prompt medical attention for any concerning symptoms, and adherence to prescribed treatment plans are also essential for successful long-term management.
Warning Signs in Long-Term IBS Management
Recognizing warning signs is crucial for early intervention and preventing potential complications. Sudden and significant changes in bowel habits, persistent abdominal pain, unexplained weight loss, or blood in the stool should be reported immediately to a healthcare professional. These signs might indicate the development of more serious conditions, requiring prompt medical attention.
Potential Complications and Management
| Potential Complication | Description | Prevention Strategies |
|---|---|---|
| Dehydration | Frequent diarrhea or loose stools can lead to significant fluid loss, potentially resulting in dehydration. Symptoms include dizziness, headache, and fatigue. | Staying well-hydrated by drinking plenty of fluids throughout the day, especially during periods of increased IBS symptoms. Consider electrolyte drinks if diarrhea is severe. |
| Nutritional Deficiencies | Malabsorption due to chronic diarrhea or dietary restrictions can lead to deficiencies in essential vitamins and minerals. This can manifest as fatigue, weakness, or skin problems. | Eating a balanced diet rich in essential nutrients. Consulting a registered dietitian for personalized dietary recommendations tailored to individual needs. |
| Anxiety and Depression | Chronic IBS symptoms can significantly impact mental health, increasing the risk of anxiety and depression. This can further exacerbate IBS symptoms in a vicious cycle. | Practicing stress-reducing techniques like yoga, meditation, or deep breathing exercises. Seeking professional help from a therapist or counselor if mental health concerns arise. |
| Anal Fissures | Frequent straining during bowel movements can cause small tears in the anal tissue, leading to pain and bleeding. | Maintaining a regular bowel routine, avoiding constipation through dietary changes and adequate hydration. Using stool softeners or laxatives as directed by a doctor. |
| Ulcerative Colitis or Crohn’s Disease | In rare cases, IBS can be mistaken for or be a precursor to other inflammatory bowel diseases (IBD) like ulcerative colitis or Crohn’s disease. Distinguishing between these conditions requires a comprehensive medical evaluation. | Regular medical check-ups and adherence to a prescribed treatment plan. Reporting any significant changes in bowel habits or symptoms to a healthcare provider promptly. |
Research and Future Directions in IBS: Facts About Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) continues to be a significant health concern, affecting millions worldwide. While our understanding of the condition has improved dramatically, there are still many unanswered questions about its underlying mechanisms and optimal management strategies. Ongoing research is crucial to advancing treatments and improving the lives of those living with IBS.Current research in IBS is multifaceted, exploring various avenues to gain a deeper understanding of the disorder.
Researchers are investigating the complex interplay of genetic predisposition, environmental factors, and the gut microbiome’s role in IBS development. This exploration aims to identify specific biomarkers and develop personalized approaches to diagnosis and treatment.
Current Research Landscape
The current research landscape in IBS encompasses a wide range of investigations. Studies are analyzing the impact of dietary interventions, such as specific diets and prebiotics/probiotics, on IBS symptoms. Researchers are also exploring the potential of psychological therapies, such as cognitive behavioral therapy (CBT), to manage IBS-related anxiety and stress. The role of gut microbiota in IBS is being extensively investigated, with studies exploring the composition and function of the gut microbiome in different IBS subtypes.
Emerging Therapies and Treatments
Emerging therapies for IBS aim to target specific mechanisms involved in the condition. One promising area is the development of targeted medications that modulate the gut’s inflammatory response or regulate gut motility. Researchers are also investigating the potential of neuromodulatory therapies, such as transcranial magnetic stimulation (TMS), to influence the brain-gut axis and reduce IBS symptoms. Furthermore, studies are exploring the use of fecal microbiota transplantation (FMT) as a potential treatment option for specific IBS subtypes characterized by gut dysbiosis.
Areas Requiring Further Research
Despite advancements, several areas require further investigation to fully unravel the complexities of IBS. Understanding the intricate relationship between the gut microbiome and the immune system in IBS is crucial. More research is needed to develop accurate diagnostic tools that can distinguish IBS subtypes and personalize treatment strategies. Identifying biomarkers to predict treatment response and tailoring therapies to individual patient needs are also important areas for future research.
The long-term effects of various interventions, including dietary modifications and specific medications, need further evaluation.
Importance of Research for Future Advancements
Research into IBS is essential for developing more effective treatments and improving the quality of life for those affected. The development of targeted therapies and personalized approaches will allow for a more precise and effective management of IBS symptoms. Increased understanding of the underlying mechanisms of IBS will ultimately lead to the development of preventative strategies. Furthermore, research provides the scientific basis for evidence-based clinical practice guidelines, enabling healthcare professionals to make informed decisions about the best treatment options for their patients.
Summary
In conclusion, facts about irritable bowel syndrome highlight the importance of understanding this prevalent digestive disorder. From its diverse manifestations to the array of treatment options and lifestyle adjustments, this comprehensive guide equips individuals with the necessary knowledge to navigate their IBS journey. Remember, seeking professional medical advice is always crucial for accurate diagnosis and personalized treatment plans.
By adopting a proactive approach to self-care and management, individuals with IBS can significantly improve their quality of life.