Eggplant carbs and glycemic index are key factors for anyone interested in incorporating this versatile vegetable into their diet, especially those concerned with blood sugar management. This comprehensive guide explores the nutritional profile of eggplant, its carbohydrate content, and its impact on the glycemic index. We’ll also look at how eggplant fits into various diets, compare it to other vegetables, and delve into potential health benefits and drawbacks.
Get ready to discover the surprising insights about this delicious and potentially healthy food!
Understanding the amount of carbohydrates and the glycemic index is crucial for anyone seeking to make informed dietary choices. This exploration of eggplant’s nutritional profile, carbohydrate content, and glycemic index will empower you to appreciate its potential role in a balanced diet. We’ll examine how cooking methods influence these factors, and discuss the potential effects on blood sugar management.
Nutritional Profile of Eggplant
Eggplant, a versatile and flavorful vegetable, offers a surprising array of nutrients. Its mild taste and tender texture make it a popular addition to countless dishes, from simple salads to elaborate stir-fries. Beyond its culinary appeal, eggplant boasts a surprisingly impressive nutritional profile, making it a healthy choice for those seeking a balanced diet.Eggplant is primarily composed of water, making it a low-calorie food.
Its nutritional benefits extend beyond its minimal calorie count, as it provides essential vitamins, minerals, and fiber, contributing to overall health and well-being. Its relatively low calorie content makes it a suitable component for weight management strategies, while its high fiber content promotes digestive health.
Nutritional Composition
Eggplant is remarkably rich in various nutrients, including vitamins, minerals, and fiber. It’s a good source of vitamin C, important for immune function and collagen production, and vitamin B6, which plays a role in red blood cell formation and other metabolic processes. It also contains potassium, a crucial mineral for maintaining healthy blood pressure. The presence of these nutrients underscores the importance of incorporating eggplant into a diverse and balanced diet.
- Vitamins: Eggplant provides a decent amount of vitamin C, contributing to immune function and overall health. Vitamin B6, another important vitamin found in eggplant, is essential for various bodily functions. Although not a primary source, it contributes to the overall nutrient intake.
- Minerals: Potassium is a significant mineral in eggplant, playing a vital role in maintaining healthy blood pressure. It also contains small amounts of other essential minerals, further contributing to its nutritional value.
- Fiber: Eggplant contains dietary fiber, which is beneficial for digestive health. Soluble fiber can help regulate blood sugar levels, while insoluble fiber aids in digestion and promotes regularity.
Calorie Count Per Serving
The calorie count of eggplant varies slightly depending on the size and preparation method. A typical medium-sized eggplant, when cooked and prepared without substantial amounts of oil or other high-calorie ingredients, provides approximately 25-35 calories per serving.
Preparation Methods and Nutritional Impact
The preparation method can slightly alter the nutritional value of eggplant. Roasting, grilling, and sautéing, for instance, can affect the water content and vitamin retention. Roasting eggplant with minimal oil, for example, can maintain a good level of nutrients. While frying eggplant in excessive oil can significantly increase the calorie count and potentially reduce some of the nutritional value.
- Roasting: Roasting with a small amount of olive oil or other healthy fats preserves many of the nutrients while adding flavor.
- Grilling: Grilling retains moisture and allows for a smoky flavor, often with minimal added fat, preserving nutritional value.
- Sautéing: Sautéing eggplant with a small amount of oil can quickly cook it while maintaining some of its nutritional content.
Comparison to Other Vegetables
The following table provides a comparative overview of the nutritional values of eggplant relative to other common vegetables:
| Vegetable | Calories (approx.) | Vitamin C (mg) | Potassium (mg) | Fiber (g) |
|---|---|---|---|---|
| Eggplant | 25-35 | 5-10 | 200-300 | 2-3 |
| Spinach | 7 | 28 | 240 | 2 |
| Broccoli | 30 | 50 | 150 | 3 |
| Carrot | 40 | 5 | 180 | 2 |
Carbohydrate Content in Eggplant
Eggplant, a versatile and popular vegetable, boasts a surprisingly low carbohydrate count. Understanding its carbohydrate composition, including fiber and sugars, and how preparation methods affect it, is key to incorporating it into a balanced diet. This section delves into the details of eggplant’s carbohydrate content and its glycemic index.
Carbohydrate Composition
Eggplant is predominantly composed of water, with carbohydrates representing a smaller portion of its overall nutritional profile. These carbohydrates primarily consist of fiber and sugars. Dietary fiber, a crucial component for digestive health, is present in eggplant. This fiber contributes to satiety and can aid in regulating blood sugar levels. Simple sugars, like fructose and glucose, are also present in smaller amounts.
The combination of these elements makes eggplant a relatively low-glycemic food.
Glycemic Index of Eggplant
The glycemic index (GI) of eggplant is generally low. This means that eggplant’s carbohydrates are digested and absorbed slowly, leading to a gradual rise in blood sugar levels. This characteristic is beneficial for individuals managing their blood sugar. The exact GI value can vary slightly based on preparation methods, with raw eggplant having a slightly lower GI than cooked.
Impact of Preparation Methods
The preparation method significantly influences the carbohydrate content of eggplant. For example, roasting eggplant often results in a slight increase in carbohydrate availability due to the breakdown of cell structure, which makes it more digestible. Boiling or steaming eggplant tends to preserve its natural structure and maintain a lower carbohydrate availability. Methods like frying or adding sugary sauces to eggplant significantly increase the overall carbohydrate content.
This is largely due to the addition of extra sugars and potentially starches from the preparation process.
Carbohydrate Content Across Serving Sizes
The following table demonstrates the approximate carbohydrate content in different serving sizes of eggplant. These values are estimations and can vary based on factors such as the specific eggplant variety and growing conditions.
| Serving Size (grams) | Approximate Carbohydrate Content (grams) |
|---|---|
| 50 grams | 2 grams |
| 100 grams | 4 grams |
| 150 grams | 6 grams |
| 200 grams | 8 grams |
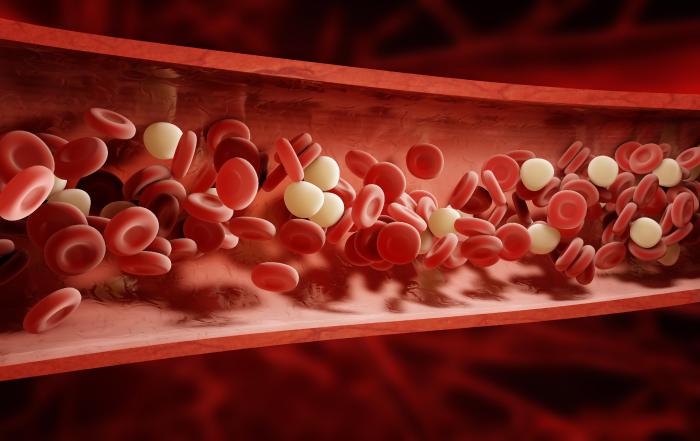
Glycemic Index of Eggplant
Eggplant, a versatile and nutritious vegetable, is often a staple in many cuisines worldwide. Understanding its impact on blood sugar levels is crucial for individuals managing their health and dietary choices. This section delves into the glycemic index of eggplant, exploring its relationship with blood sugar, factors influencing its GI, comparisons with other vegetables, and the effect of cooking methods.The glycemic index (GI) is a ranking of carbohydrates based on how quickly they raise blood sugar levels after consumption.
Foods with a low GI are digested and absorbed more slowly, leading to a gradual increase in blood sugar, which is generally better for metabolic health. Foods with a high GI cause a rapid spike in blood sugar, followed by a potential crash.
Factors Influencing Eggplant’s Glycemic Index
The glycemic index of eggplant is influenced by several factors, including its maturity, ripeness, and preparation method. These factors impact the starch content and fiber levels, directly affecting the rate of digestion and subsequent blood sugar response.
Comparison to Other Vegetables
Eggplant’s glycemic index typically falls within the low range, which places it favorably compared to many other vegetables. For instance, compared to potatoes or corn, eggplant tends to have a lower glycemic index, indicating a slower rise in blood sugar levels. A lower GI is generally associated with a more gradual release of glucose into the bloodstream, promoting better metabolic control.
Eggplant, surprisingly, has a relatively low glycemic index, meaning it doesn’t drastically spike your blood sugar. While focusing on healthy eating is important for overall well-being, understanding the role of nutrition in managing various health conditions like those involving unresectable tumors, is also crucial. Learning more about the reasons behind treatment options for such cases can be insightful, as detailed in this helpful article on unresectable tumors reasons treatment.
Ultimately, knowing your eggplant’s carb count and glycemic index can help you make informed dietary choices.
Impact of Cooking Methods on Eggplant’s Glycemic Index
Cooking methods play a significant role in altering the glycemic index of eggplant. Cooking can affect the structure of the plant’s starches and fibers, influencing how quickly they are digested. Generally, cooked eggplant has a slightly higher glycemic index than raw eggplant, but the difference is often minimal. The extent of this increase depends on the specific cooking method employed.
Raw vs. Cooked Eggplant Glycemic Index
Generally, raw eggplant has a lower glycemic index compared to cooked eggplant. This is due to the cooking process potentially breaking down some of the fiber and increasing the starch’s accessibility to digestive enzymes. However, the differences are often small, and the overall glycemic impact of eggplant, even when cooked, remains relatively low.
Eggplant and Blood Sugar Management
Eggplant, a versatile and flavorful vegetable, has garnered attention for its potential role in managing blood sugar levels. Its nutritional composition, particularly its fiber content, might play a crucial part in this process. Understanding how eggplant interacts with blood sugar control is important for individuals looking to incorporate this vegetable into a healthy diet, especially those with diabetes or prediabetes.Eggplant’s relatively low glycemic index (GI) suggests a minimal impact on blood glucose levels after consumption.
Ever wondered about eggplant’s carb count and its impact on blood sugar? It turns out eggplant is surprisingly low in carbs, making it a good option for those watching their glycemic index. While researching this, I stumbled upon a really helpful resource for those looking to self-diagnose atopic dermatitis – ask an expert self diagnose atopic dermatitis.
This comprehensive guide was incredibly informative and, honestly, a bit of a lifesaver. Regardless, eggplant’s low carb profile makes it a smart choice for a balanced diet.
This, combined with its high fiber content, contributes to a slower absorption of sugars into the bloodstream. While further research is needed to fully elucidate the mechanisms, preliminary findings point towards eggplant’s potential benefits in blood sugar management.
Potential Role in Blood Sugar Regulation
Eggplant’s fiber content, primarily soluble fiber, helps slow down the digestion and absorption of carbohydrates. This gradual release of glucose into the bloodstream minimizes spikes in blood sugar levels, which is a key factor in managing blood sugar. The presence of other nutrients, such as antioxidants, might also contribute to overall metabolic health, indirectly supporting blood sugar regulation.
Research on Eggplant and Blood Sugar Control
Limited research directly examines eggplant’s effect on blood sugar control in humans. However, studies on the effects of other vegetables with similar nutritional profiles, like other high-fiber vegetables, often indicate a positive association with improved glycemic control. These studies highlight the importance of dietary fiber in managing blood sugar. Further clinical trials focusing specifically on eggplant’s impact are necessary to solidify these preliminary findings.
Benefits of Incorporating Eggplant into a Diabetic Diet
Incorporating eggplant into a diabetic diet can offer several potential benefits. Its low calorie density and high fiber content contribute to a feeling of fullness, potentially aiding in weight management, a crucial factor in blood sugar control. The presence of various vitamins and minerals further enhances the nutritional value of the diet. However, it is essential to consider potential limitations.
Limitations of Eggplant in a Diabetic Diet, Eggplant carbs and glycemic index
While eggplant offers potential benefits, it’s crucial to consider potential limitations. Individual responses to eggplant, like any food, can vary. Furthermore, the impact of eggplant on blood sugar is not universally conclusive, and more research is necessary. Careful portion control and mindful dietary planning are essential to optimize the benefits of eggplant while adhering to specific dietary needs.
Summary Table: Potential Effects of Eggplant Consumption on Blood Sugar Levels
| Factor | Potential Effect |
|---|---|
| Low Glycemic Index | Minimizes rapid blood sugar spikes |
| High Fiber Content | Slows down carbohydrate absorption |
| Nutrient Density | Potential contribution to overall metabolic health |
| Limited Research | Further clinical trials needed for conclusive evidence |
Eggplant in Different Diets
Eggplant, a versatile and flavorful vegetable, easily integrates into various dietary plans. Its low calorie count and nutritional profile make it a suitable addition to vegetarian, vegan, and even low-carb diets. Understanding how to incorporate eggplant into your meals can lead to delicious and healthy options.
Vegetarian and Vegan Diets
Eggplant is a staple in many vegetarian and vegan cuisines. Its mild flavor allows it to absorb various seasonings and complements a wide range of dishes. It’s a great source of fiber, vitamins, and minerals, making it a valuable addition to a plant-based diet. For example, roasted eggplant with herbs and spices can be a satisfying and nutritious side dish, while stuffed eggplant boats provide a hearty and flavorful main course.
Low-Carb Diets
Eggplant’s low carbohydrate content makes it a welcome addition to low-carb diets. Its relatively low glycemic index means it won’t significantly impact blood sugar levels. This characteristic allows for its inclusion in low-carb meals without major concerns about carbohydrate intake. For example, eggplant parmesan, often associated with higher carb intake, can be adapted with low-carb substitutes, like cauliflower “rice,” for a lower-carb alternative.
Eggplant in Weight Management
Eggplant’s low calorie density contributes to weight management efforts. Its high fiber content promotes satiety, helping to reduce overall calorie intake. This can be a useful tool in managing weight by helping to curb cravings and promote fullness. Moreover, eggplant is a nutrient-rich vegetable, providing essential vitamins and minerals without excessive calories.
Eggplant as a Recipe Substitute
Eggplant can effectively substitute other ingredients in recipes, providing similar textures and flavors while often reducing calories and carbohydrates. This versatility allows for adaptation and creativity in the kitchen. For example, eggplant can replace zucchini in frittatas or stuffed bell peppers.
Potential Eggplant Substitutes
While eggplant is a versatile ingredient, there might be instances where a suitable alternative is needed. The following table presents some potential substitutes, keeping in mind their respective characteristics and nutritional profiles.
| Eggplant Substitute | Potential Use Cases | Nutritional Considerations |
|---|---|---|
| Zucchini | Sauteed dishes, frittatas, roasted vegetables | Slightly lower in fiber, similar in moisture content |
| Cauliflower | Rice substitutes, roasted vegetables, soups | Lower in calories and carbohydrates, but different texture |
| Mushrooms | Sauteed dishes, casseroles, stir-fries | Rich in nutrients, can vary in moisture content |
| Bell Peppers | Stuffed dishes, salads, stir-fries | Higher in Vitamin C, lower in carbohydrates |
Comparison with Other Vegetables
Eggplant, often overlooked, offers a unique nutritional profile compared to other common vegetables. Understanding its carbohydrate content and glycemic index alongside similar vegetables like zucchini, bell peppers, and tomatoes provides a clearer picture of its place in a balanced diet. This comparison reveals not only nutritional similarities but also subtle differences that can influence dietary choices. By exploring recipes and potential health benefits, we can better appreciate the diverse role each vegetable plays in a healthy lifestyle.
Eggplant, surprisingly, has a relatively low glycemic index, making it a good choice for those watching their carb intake. However, the recent executive order to restrict gender affirming care executive order to restrict gender affirming care highlights a concerning trend of limiting choices and potentially impacting health outcomes for many. This, in turn, raises questions about the wider implications of such restrictions, even when it comes to seemingly simple dietary choices like eggplant carbs and their glycemic impact.
Carbohydrate Content and Glycemic Index Comparison
A key aspect of comparing vegetables is their carbohydrate content and how quickly those carbohydrates are digested (glycemic index). These factors directly impact blood sugar levels. The table below provides a concise comparison of eggplant with zucchini, bell peppers, and tomatoes, showcasing their respective carbohydrate counts and glycemic index values. These values can vary slightly depending on factors like growing conditions and ripeness.
| Vegetable | Carbohydrates (per 100g, approximate) | Glycemic Index (approximate) |
|---|---|---|
| Eggplant | 3-4g | 15-20 |
| Zucchini | 4-5g | 15-25 |
| Bell Peppers (red) | 5-6g | 10-15 |
| Tomatoes | 3-4g | 10-15 |
Recipe Examples
These vegetables, despite minor differences in carbohydrate content and glycemic index, are all incredibly versatile. Here are a few examples of recipes showcasing their culinary possibilities:
- Eggplant Parmesan: A classic Italian dish featuring slices of eggplant, breaded and baked, layered with tomato sauce and mozzarella cheese. The eggplant provides a hearty, flavorful base to the dish.
- Stuffed Zucchini Boats: Zucchini halves are hollowed out and filled with a savory mixture of rice, herbs, and vegetables. This offers a light and nutritious option, making zucchini an excellent choice for a side dish or main course.
- Roasted Bell Pepper and Tomato Salad: Roasted bell peppers and tomatoes combine to create a vibrant and flavorful salad. The sweet and savory flavors of these vegetables create a delicious combination. This salad can be served as a side dish or as a light meal.
- Tomato Basil Soup: A refreshing and flavorful soup, made with ripe tomatoes, basil, and other vegetables. The sweet and savory flavor profile is enhanced by the addition of basil.
Nutritional Similarities and Differences
All these vegetables are excellent sources of vitamins and minerals, contributing to overall health. Crucially, they are all low in calories and high in fiber. While the carbohydrate content and glycemic index vary slightly, these differences are often negligible in the context of a balanced diet.
Potential Health Benefits
The health benefits associated with these vegetables are numerous. They are rich in antioxidants, contributing to cell protection and overall well-being. Eggplant, in particular, contains compounds that may help regulate blood sugar levels. Zucchini and bell peppers are also known for their vitamin C content, strengthening the immune system. Tomatoes are rich in lycopene, a powerful antioxidant linked to heart health.
Potential Health Benefits and Drawbacks

Eggplant, a versatile and flavorful vegetable, offers a wide range of potential health benefits beyond its impact on blood sugar levels. From its antioxidant properties to its role in supporting digestive health, eggplant could be a valuable addition to a balanced diet. However, like any food, it’s essential to understand its potential drawbacks and interactions with other factors to ensure responsible consumption.
This section explores the nuanced aspects of eggplant consumption, providing a comprehensive overview of its potential benefits and drawbacks.Understanding the potential benefits and drawbacks of eggplant consumption allows for informed choices about its inclusion in a balanced diet. Recognizing potential interactions with medications or other dietary components is crucial for optimizing its health benefits and mitigating any potential negative impacts.
Potential Health Benefits
Eggplant is rich in various nutrients that contribute to overall health. Its high fiber content promotes healthy digestion, aiding in the prevention of constipation and supporting a feeling of fullness. The presence of antioxidants, like vitamin C and various flavonoids, helps protect cells from damage caused by free radicals. This antioxidant activity may contribute to a reduced risk of chronic diseases.
- Digestive Health: The high fiber content in eggplant can promote regularity and prevent constipation. Fiber acts as a bulking agent, softening stool and stimulating bowel movements. This is particularly important for individuals with digestive issues or those seeking to maintain healthy bowel function.
- Antioxidant Properties: Eggplant contains a variety of antioxidants, including vitamin C and various flavonoids. These compounds help neutralize free radicals, which can damage cells and contribute to the development of chronic diseases like heart disease and cancer. Studies have shown that the antioxidant content in eggplant may also contribute to protecting the body against cell damage.
- Blood Pressure Regulation: Some research suggests that the potassium content in eggplant may contribute to maintaining healthy blood pressure levels. Potassium helps regulate fluid balance and can counter the effects of sodium, potentially reducing the risk of hypertension.
Potential Drawbacks and Considerations
While eggplant generally presents a low risk of adverse effects, some considerations are important. Individual sensitivities or allergies to certain vegetables can occur. Moreover, eggplant’s potential interaction with certain medications warrants attention.
- Allergies and Sensitivities: Like other vegetables, some individuals may experience allergic reactions or sensitivities to eggplant. Symptoms can range from mild skin rashes to more severe reactions. If you have a known allergy to nightshade plants (like tomatoes, potatoes, and peppers), you may want to exercise caution when consuming eggplant.
- Medication Interactions: While not extensively studied, some medications, particularly those affecting blood sugar or blood pressure, might interact with the components of eggplant. It’s crucial to consult with a doctor or pharmacist if you are taking any medications and considering incorporating eggplant into your diet. This ensures no unwanted interactions occur.
- Potential for Oxalate Content: Eggplant contains a small amount of oxalates. High oxalate intake might be problematic for individuals with kidney stones. However, the amount in eggplant is generally not a significant concern for most people.
Summary Table
| Aspect | Potential Health Benefits | Potential Drawbacks |
|---|---|---|
| Digestive Health | Promotes regularity, prevents constipation | Possible allergic reactions or sensitivities in some individuals |
| Antioxidant Properties | Neutralizes free radicals, potentially reducing risk of chronic diseases | Potential interaction with certain medications |
| Blood Pressure Regulation | May contribute to healthy blood pressure | Potential oxalate content (minimal concern for most people) |
Illustrative Examples of Eggplant Dishes

Eggplant, a versatile vegetable, lends itself beautifully to a wide array of culinary creations. From simple preparations to elaborate dishes, eggplant’s delicate flavor and adaptable texture allow for a diverse range of tastes and experiences. This exploration showcases several eggplant dishes, highlighting their nutritional profiles and potential impact on blood sugar levels.
Eggplant Parmesan
This classic Italian dish features slices of eggplant, breaded and fried, layered with mozzarella cheese and tomato sauce. The preparation method involves breading the eggplant slices to create a crispy exterior and a tender interior, adding a flavorful depth to the dish. The coating of breading significantly alters the dish’s nutritional profile, increasing the calorie and fat content.
While the tomato sauce provides essential vitamins and minerals, the cheese adds fat and sodium. The impact on blood sugar levels is moderate. The carbohydrates from the breading and tomato sauce will raise blood sugar, but the protein and fiber from the eggplant and cheese help to moderate this response.Visualize a golden-brown, crispy eggplant slice, glistening with melted mozzarella.
The rich, tomato-based sauce adds a vibrant red hue, contrasted by the creamy white cheese. The fragrant aroma of herbs, like oregano and basil, permeates the air. The crispy exterior of the eggplant and the soft, melting cheese create a delightful textural contrast.
Eggplant Curry
This flavorful dish, common in Indian cuisine, typically involves simmering eggplant in a rich, aromatic curry sauce. The eggplant is often diced or sliced and cooked in a mixture of spices, including turmeric, ginger, and garlic. The curry sauce adds a substantial amount of flavor and often contains ingredients like coconut milk, which can increase the fat content of the dish.
The spices and herbs offer various vitamins and minerals. The nutritional profile of this dish depends greatly on the specific ingredients used in the curry. The impact on blood sugar levels is generally moderate. The carbohydrates from the eggplant and any added starchy vegetables will influence blood sugar, but the protein and fiber in the dish will moderate the response.Imagine a vibrant dish with deep purples and yellows.
The eggplant, tender and slightly caramelized, is nestled within a rich, fragrant curry sauce. The aroma of spices like cumin, coriander, and turmeric fills the air, creating a warm and inviting sensory experience. The texture of the dish is a harmonious blend of smooth sauce and tender eggplant.
Roasted Eggplant with Herbs
This simple yet elegant dish features roasted eggplant, seasoned with a medley of fresh herbs. The eggplant is typically sliced and roasted until tender and slightly caramelized. The preparation method allows the eggplant to retain its natural flavors and nutritional profile, minimizing the addition of extra fats and carbohydrates. The roasted eggplant provides vitamins, minerals, and fiber. The impact on blood sugar levels is generally low, as the dish is low in carbohydrates.Visualize glistening eggplant slices, beautifully browned and tinged with the vibrant hues of roasted vegetables.
The aroma of herbs like thyme, rosemary, and oregano fills the air, creating a delightful sensory experience. The tender, slightly smoky texture of the eggplant complements the freshness of the herbs.
Eggplant Kofta
This Middle Eastern dish features ground eggplant mixed with spices and herbs, formed into patties and pan-fried or baked. The preparation involves mixing the eggplant with other ingredients, such as breadcrumbs or bulgur, which can affect the nutritional profile of the dish. The presence of spices and herbs provides various vitamins and minerals. The impact on blood sugar levels will depend on the ingredients and preparation method.Imagine tender, flavorful eggplant patties, golden brown on the outside and moist within.
The aroma of spices and herbs wafts from the dish, creating a rich and inviting sensory experience. The slightly firm texture of the kofta, combined with the moist interior, offers a delightful balance.
Conclusion: Eggplant Carbs And Glycemic Index
In conclusion, eggplant, despite its relatively low carbohydrate count and generally moderate glycemic index, offers a variety of potential benefits, particularly for those managing blood sugar levels. The key takeaway is that eggplant’s nutritional value, especially its fiber content, plays a role in blood sugar regulation. By understanding its carbohydrate profile and glycemic index, along with its potential health benefits and drawbacks, you can confidently incorporate eggplant into your diet in a way that aligns with your overall health goals.
So, next time you’re planning a meal, remember the delicious and potentially nutritious eggplant!