Polycythemia and coronavirus covid 19 risks complications considerations – Polycythemia and coronavirus COVID-19 risks complications considerations are a critical area of focus. This exploration delves into the intricate interplay between these conditions, examining the potential risks, complications, and management strategies. We’ll define polycythemia vera, understand the mechanisms of COVID-19, and analyze the unique challenges faced by individuals with both conditions.
From understanding the pathophysiology of polycythemia vera to exploring potential long-term effects of COVID-19, this comprehensive overview aims to equip readers with a deeper understanding of the complexities involved. We’ll also discuss management strategies, prevention, and present illustrative hypothetical case studies to solidify our understanding.
Defining Polycythemia Vera
Polycythemia vera (PV) is a chronic myeloproliferative neoplasm characterized by an abnormally high production of red blood cells, white blood cells, and platelets. This overproduction leads to an increase in blood volume and viscosity, potentially causing various health complications. Understanding PV requires a deep dive into its causes, symptoms, and diagnostic methods, as well as the intricate pathophysiology underlying this condition.
Causes of Polycythemia Vera
The precise cause of polycythemia vera remains unknown. However, research suggests that genetic mutations, particularly in the JAK2 gene, play a significant role in the development of this condition. These mutations lead to uncontrolled cell growth and proliferation within the bone marrow. Environmental factors might also contribute to the onset of PV, but their exact impact is still under investigation.
Symptoms of Polycythemia Vera
Individuals with polycythemia vera often experience a range of symptoms, some of which are directly related to the increased blood volume and viscosity. These symptoms can vary in severity and presentation. Common symptoms include headaches, dizziness, blurred vision, and an increased risk of blood clots. Some patients may also experience fatigue, pruritus (itching), and an enlarged spleen (splenomegaly).
Early detection and management are crucial to minimize the potential complications associated with the disease.
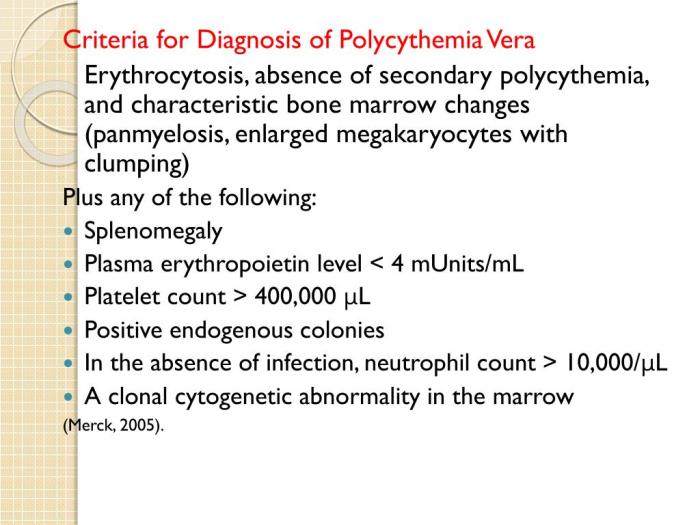
Diagnostic Criteria for Polycythemia Vera
Diagnosis of polycythemia vera involves a multi-faceted approach. Physicians rely on a combination of blood tests, bone marrow biopsies, and genetic analysis to confirm the diagnosis. Elevated red blood cell count, hemoglobin, and hematocrit levels are key indicators. Furthermore, the presence of JAK2 mutations is highly suggestive of PV. The diagnostic process aims to distinguish PV from other hematological conditions with similar symptoms.
Pathophysiology of Polycythemia Vera
The pathophysiology of PV centers around the dysregulation of blood cell production within the bone marrow. The uncontrolled proliferation of hematopoietic stem cells leads to an overproduction of red blood cells, white blood cells, and platelets. This overproduction results in an increase in blood volume and viscosity, potentially leading to several complications. The JAK2 mutation is thought to be a crucial driver of this abnormal cell proliferation.
Types of Polycythemia
Polycythemia encompasses several related conditions, each with distinct characteristics. While polycythemia vera is a myeloproliferative neoplasm, other forms of polycythemia exist, including secondary polycythemia. Secondary polycythemia arises from factors external to the bone marrow, such as chronic lung disease or living at high altitudes. Differentiating between these types is crucial for accurate diagnosis and targeted treatment.
Comparison of Polycythemia Vera with Other Hematological Disorders
| Feature | Polycythemia Vera | Secondary Polycythemia | Essential Thrombocythemia | Myelofibrosis |
|---|---|---|---|---|
| Red Blood Cell Count | Elevated | Elevated | Normal or slightly elevated | Variable |
| Platelet Count | Elevated | Normal | Significantly elevated | Variable |
| White Blood Cell Count | Elevated | Normal | Normal or slightly elevated | Variable |
| JAK2 Mutation | Frequently present | Absent | Frequently present | Variable |
| Cause | Genetic mutation (JAK2) | External factors (e.g., lung disease) | Genetic mutation (JAK2) | Genetic mutation and other factors |
This table provides a concise comparison of polycythemia vera with other hematological disorders, highlighting key distinctions in their diagnostic features. Recognizing these differences is essential for accurate diagnosis and appropriate management.
Understanding Coronavirus (COVID-19)
The coronavirus disease 2019 (COVID-19), caused by the SARS-CoV-2 virus, has had a profound impact on global health. Understanding its mechanisms of infection, immune response, and potential long-term effects is crucial for both prevention and management. This exploration will delve into the key aspects of COVID-19, emphasizing the complexities of this viral infection.The SARS-CoV-2 virus primarily infects the respiratory system, often causing mild to moderate respiratory illness.
The virus gains entry into host cells through the ACE2 receptor, a protein commonly found on the surface of cells in the lungs and other tissues. Once inside, the virus replicates, leading to inflammation and damage within the infected tissues.
Mechanisms of Infection and Progression
The SARS-CoV-2 virus enters the body primarily through the respiratory system, often via inhalation of infected droplets. Initial infection may manifest as mild symptoms, including fever, cough, and fatigue. In severe cases, the virus can cause a more pronounced inflammatory response, leading to acute respiratory distress syndrome (ARDS), multi-organ failure, and even death. The progression of the disease varies significantly depending on individual factors like age, pre-existing conditions, and immune system strength.
Immune Response to COVID-19
The human immune system responds to the SARS-CoV-2 infection with a complex cascade of events. Initially, innate immune cells, such as macrophages and neutrophils, recognize and attempt to neutralize the virus. Subsequently, adaptive immune responses, including the production of antibodies and activation of T cells, contribute to the elimination of the virus. However, an overactive or dysregulated immune response can lead to severe inflammation and tissue damage, contributing to complications like ARDS and blood clots.
Understanding polycythemia and its potential complications with COVID-19 is crucial. One aspect of managing this condition involves diet, and knowing which fruits provide essential nutrients like magnesium is important. For example, discovering which fruits are rich in magnesium could help you make healthier choices. what fruit has magnesium Knowing this can support overall well-being, particularly when dealing with conditions like polycythemia and its potential interactions with coronavirus.
A balanced diet, including magnesium-rich foods, may be a beneficial strategy in managing polycythemia and its related COVID-19 risks.
Understanding this complex immune response is crucial for developing effective treatments and preventative measures.
Long-Term Effects of COVID-19, Including Cardiovascular Implications
Beyond the acute phase of infection, many individuals experience long-term health consequences, often referred to as “long COVID.” These effects can range from persistent fatigue and breathing difficulties to neurological symptoms and cardiovascular issues. Studies have highlighted a correlation between COVID-19 and an increased risk of heart inflammation (myocarditis) and blood clots, potentially leading to long-term cardiovascular complications, such as heart failure and stroke.
Further research is needed to fully understand the long-term effects and develop effective strategies for managing these issues.
Stages of COVID-19 Infection
| Stage | Description |
|---|---|
| Incubation Period | The time between exposure to the virus and the appearance of symptoms. This period can vary from 1 to 14 days, and during this time, the individual may be contagious. |
| Early Infection | Symptoms such as fever, cough, and fatigue typically manifest during this phase. The severity of symptoms can range from mild to severe. |
| Severe Infection | Individuals with severe infection may experience difficulty breathing, chest pain, and other concerning symptoms. This stage requires prompt medical intervention. |
| Recovery | This stage involves the gradual resolution of symptoms, although some individuals may experience long-term effects (long COVID). |
Polycythemia and COVID-19
Navigating the complexities of polycythemia vera (PV) alongside the novel coronavirus disease 2019 (COVID-19) presents unique challenges. Understanding the potential interactions between these two conditions is crucial for developing effective strategies to manage and mitigate risks for individuals with PV. This exploration delves into the possible ways PV can impact COVID-19 responses, potential exacerbating factors, and the implications of COVID-19 treatments on PV patients.The interplay between PV and COVID-19 is multifaceted, demanding careful consideration.
Elevated red blood cell counts, a hallmark of PV, can potentially affect the body’s immune response to the virus. This intricate relationship necessitates a thorough understanding of the interplay to optimize treatment approaches and ensure the best possible outcomes for patients with both conditions.
Potential Impact of PV on COVID-19 Response
PV’s impact on COVID-19 response is complex. The elevated red blood cell count and hematocrit in PV can potentially lead to increased blood viscosity. This thickened blood can hinder oxygen delivery to tissues, potentially exacerbating the effects of COVID-19, particularly if lung involvement is present. Furthermore, the inflammatory state often associated with PV could potentially worsen the inflammatory response to the virus.
Exacerbating Factors of COVID-19 in PV Patients
Several factors can exacerbate COVID-19 in PV patients. The elevated blood viscosity, as previously discussed, can hinder oxygen transport, potentially leading to hypoxia and worsening respiratory complications. Additionally, the already-present inflammatory state in PV could increase the body’s susceptibility to the inflammatory response triggered by COVID-19. Pre-existing cardiovascular conditions, which are sometimes associated with PV, could further complicate the situation, making patients more vulnerable to cardiovascular complications related to COVID-19.
Potential Effects of COVID-19 Treatment on PV Patients
The impact of COVID-19 treatments on PV patients is another area of concern. Some antiviral medications used to treat COVID-19 may interact with the medications commonly used to manage PV. Careful monitoring of the patient’s response to both treatments is crucial to prevent adverse drug interactions.
Summary Table of Potential Interactions
| Factor | Potential Impact on COVID-19 | Potential Impact on PV |
|---|---|---|
| Elevated Blood Viscosity | Impaired oxygen delivery, potential exacerbation of respiratory complications. | May lead to increased risk of thrombosis. |
| Pre-existing Inflammation | Potentially worsened inflammatory response to COVID-19. | May increase the risk of complications. |
| Antiviral Medications | Potential drug interactions with PV medications. | Potential exacerbation of existing side effects or emergence of new ones. |
| Immunosuppressive Agents | Potentially increased risk of severe COVID-19. | Potential for exacerbating PV symptoms. |
Risks Associated with Polycythemia and COVID-19
Polycythemia vera (PV) is a chronic blood disorder characterized by an increased production of red blood cells. Patients with PV often have an elevated risk of blood clots, a serious complication that can lead to various health issues. The coronavirus disease 2019 (COVID-19) pandemic has highlighted the importance of understanding how pre-existing conditions, like PV, can interact with the virus and affect outcomes.
This section explores the heightened risks of complications for PV patients infected with COVID-19.Understanding these risks is crucial for developing tailored management strategies and improving patient care. Early recognition and proactive intervention can significantly reduce the potential severity of COVID-19 in individuals with PV. This is especially important as the virus’s impact on patients with pre-existing conditions can be more pronounced.
Increased Risks of Complications in PV Patients with COVID-19
Patients with polycythemia vera (PV) who contract COVID-19 face a heightened risk of various complications. This stems from the interplay between PV’s characteristic blood abnormalities and the inflammatory response triggered by the virus. The increased red blood cell mass and tendency towards blood clotting in PV patients can exacerbate the complications associated with COVID-19 infection. These factors can contribute to a more severe course of the illness.
Potential for Thrombotic Events in PV Patients with COVID-19
Polycythemia vera significantly increases the risk of blood clots (thrombosis). The combination of PV and COVID-19 infection can synergistically elevate this risk. The inflammatory response to COVID-19 can further activate the clotting cascade, leading to a higher chance of blood clots forming in various parts of the body, including the lungs, heart, and brain. This risk is particularly concerning as blood clots can cause severe complications, including pulmonary embolism, stroke, and deep vein thrombosis.
Furthermore, patients with PV already have a predisposition towards clotting disorders, which is further amplified when combined with the pro-inflammatory and pro-coagulant effects of COVID-19.
Understanding polycythemia and its increased coronavirus COVID-19 risks is crucial. This often leads to complications, and it’s important to consider how lifestyle choices like exercise can impact these risks. For instance, incorporating cardiovascular exercise, like brisk walking or cycling, into a healthy routine can significantly improve overall health, particularly for those with diabetes. This is further highlighted in a recent study on cardiovascular exercise and diabetes , demonstrating the link between physical activity and diabetes management.
Ultimately, understanding how exercise can influence diabetes management can be directly applied to navigating the potential risks of polycythemia and COVID-19.
Increased Risk of Severe COVID-19 Outcomes in PV Patients
Individuals with polycythemia vera (PV) who contract COVID-19 may experience more severe outcomes compared to those without PV. The increased risk of complications, particularly thrombosis, contributes to this elevated severity. The inflammatory response induced by COVID-19 can exacerbate the existing blood clotting tendencies in PV patients, leading to a higher risk of critical complications. The increased viscosity of the blood in PV patients can also hinder oxygen delivery to the tissues, contributing to the severity of the illness.
These combined factors can result in more severe respiratory distress and organ damage in PV patients with COVID-19.
Potential Complications and Likelihood in PV Patients with COVID-19
| Potential Complications | Likelihood (Estimated) |
|---|---|
| Thrombosis (e.g., pulmonary embolism, deep vein thrombosis, stroke) | High |
| Acute respiratory distress syndrome (ARDS) | Moderate |
| Myocardial infarction (heart attack) | Moderate |
| Renal failure | Low to Moderate |
| Sepsis | Moderate |
Note: This table provides an estimated likelihood of complications. Individual outcomes can vary significantly based on several factors, including the severity of the COVID-19 infection, the specific PV management strategies, and the patient’s overall health. Consult with a healthcare professional for personalized advice.
Complications of Polycythemia and COVID-19
Polycythemia vera (PV) is a blood disorder characterized by an increased production of red blood cells. This, coupled with potential underlying inflammatory responses, can significantly impact a patient’s vulnerability to complications if they contract COVID-19. Understanding the interplay between these two conditions is crucial for effective management and patient care. This section will explore the specific complications that can arise, the mechanisms by which PV can worsen these complications, and the potential long-term health consequences.The presence of elevated red blood cell counts in PV patients can lead to a heightened risk of blood clots, impacting various organ systems.
This increased risk, combined with the potential for inflammation and immune dysregulation often associated with COVID-19, creates a complex interplay that can significantly exacerbate complications. Early recognition and aggressive management of these complications are vital to improve patient outcomes.
Specific Complications Arising from PV and COVID-19
PV patients with COVID-19 are at higher risk for a range of complications compared to those without PV. These complications stem from the interplay between the hypercoagulable state of PV and the inflammatory response triggered by COVID-19. Thrombotic events, including pulmonary embolism and deep vein thrombosis (DVT), are of particular concern.
Understanding polycythemia vera and its increased risk of complications during a COVID-19 infection is crucial. While there’s no direct connection between these conditions and how to encourage eating in dementia patients, the shared need for careful management of health conditions highlights the importance of comprehensive care. For example, learning strategies for encouraging food intake in those with dementia can be helpful for anyone working with complex health situations, like navigating the specific challenges of polycythemia vera and COVID-19, especially given the heightened risk of complications.
This comprehensive approach to care is vital for ensuring the best possible outcomes for patients with polycythemia and COVID-19. Check out this resource on how to get dementia patients to eat for practical advice.
Mechanisms of Exacerbation
The increased red blood cell mass in PV contributes to a hyperviscous blood state. This, combined with potential inflammation from COVID-19, can significantly increase the risk of blood clots forming. Moreover, the inflammatory response triggered by the virus can further exacerbate the hypercoagulability associated with PV.
Potential Complications by Organ System
| Organ System | Potential Complications |
|---|---|
| Cardiovascular | Myocardial infarction (heart attack), stroke, pulmonary embolism, deep vein thrombosis (DVT), hypertension |
| Respiratory | Acute respiratory distress syndrome (ARDS), pneumonia, exacerbation of pre-existing respiratory conditions |
| Renal | Acute kidney injury, thrombotic microangiopathy |
| Neurological | Stroke, seizures, encephalopathy |
| Gastrointestinal | Ischemic bowel disease, abdominal pain |
Long-Term Health Consequences
The combined impact of PV and COVID-19 can result in long-term health consequences. Patients may experience persistent cardiovascular issues, including heart damage and impaired vascular function, long-term respiratory problems, and neurological complications. The specific long-term effects vary depending on the severity of both conditions and the individual’s response to treatment. For instance, a patient with severe COVID-19 and pre-existing PV may experience long-term lung scarring (fibrosis) and persistent fatigue, impacting their quality of life significantly.
Considerations for Management
Managing patients with both polycythemia vera (PV) and COVID-19 requires a multifaceted approach that addresses the unique challenges posed by each condition. Careful consideration must be given to the potential interactions between the two diseases, the increased risk of complications, and the specific needs of the patient. This necessitates a personalized strategy, tailored to individual circumstances and disease severity.Effective management involves a combination of medical interventions, supportive care, and close monitoring.
Strategies must prioritize patient safety and well-being, while also aiming to mitigate the risk of severe outcomes associated with either condition. Understanding the specific challenges allows for the development of a comprehensive and effective management plan.
Treatment Options and Precautions
A comprehensive approach to managing patients with both PV and COVID-19 necessitates a careful evaluation of treatment options, taking into account the specific needs of the individual patient. This involves considering the severity of both PV and COVID-19, as well as any pre-existing conditions. Treatments for COVID-19, such as antiviral medications and supportive care, must be implemented cautiously, given the potential impact on PV management.
Similarly, treatment for PV, such as phlebotomy and cytoreductive therapies, needs to be carefully balanced with the need to avoid exacerbating COVID-19 symptoms. Precautions to minimize the risk of infection transmission, such as isolation and hand hygiene, are crucial.
Importance of Close Monitoring
Close monitoring is essential for patients with both PV and COVID-19. Regular assessment of blood counts, oxygen saturation, and vital signs is critical to detect any signs of complications from either condition. This close monitoring allows for early intervention if complications arise, potentially improving outcomes. The frequent monitoring also provides insights into the interaction between the two conditions, enabling adjustments to the treatment plan as needed.
Real-time monitoring of patient response to interventions is critical to optimizing outcomes.
Potential Challenges in Management
Managing patients with both PV and COVID-19 presents several challenges. The potential for blood clotting abnormalities, exacerbated by both conditions, necessitates careful monitoring and management. The need for frequent blood draws and other medical procedures during COVID-19 monitoring can pose challenges in terms of infection control and patient comfort. Furthermore, the complexity of the treatment regimens and the need for coordination among different healthcare providers can be a significant challenge.
Management Strategies Table
| Category | Management Strategy | Rationale |
|---|---|---|
| Initial Assessment | Thorough evaluation of PV and COVID-19 severity, including blood counts, oxygen saturation, and symptom assessment. | Establishing a baseline for treatment and monitoring progress. |
| Treatment | Tailored treatment for both PV and COVID-19, considering the severity of each condition. Consider antiviral medications, supportive care, and appropriate PV therapies. | Addressing the individual needs of the patient and minimizing potential complications. |
| Monitoring | Frequent monitoring of blood counts, oxygen saturation, vital signs, and symptoms. | Early detection of complications and prompt intervention. |
| Precautions | Strict adherence to infection control measures, including isolation and hand hygiene. | Minimizing the risk of infection transmission and complications. |
| Coordination | Close collaboration between hematologists, infectious disease specialists, and other healthcare providers. | Ensuring comprehensive and coordinated care. |
Illustrative Cases (Hypothetical)
Understanding the interplay between polycythemia vera (PV) and COVID-19 requires examining potential scenarios. While real-world patient data is crucial, hypothetical cases can illuminate the complexities of managing these conditions together and highlight potential complications. These examples, though fictional, are constructed based on known medical realities and are intended to illustrate possible outcomes and management approaches.
Case Study 1: Initial Presentation and Complications
This case study focuses on a patient presenting with a severe COVID-19 infection, compounded by underlying PV. The interplay of the two conditions can significantly increase the risk of complications.
| Patient Demographics | Symptoms | Treatment Outcomes |
|---|---|---|
| 55-year-old male with a history of PV diagnosed 5 years prior, well-controlled with phlebotomy. | Developed fever, cough, and shortness of breath within 3 days of exposure to COVID-19. Elevated hematocrit and hemoglobin levels were observed. He exhibited signs of hypoxia and respiratory distress. His PV, exacerbated by the inflammatory response of COVID-19, resulted in increased blood viscosity, potentially contributing to microthrombi formation in the lungs. | Admitted to the intensive care unit (ICU) and treated with supplemental oxygen, antiviral medications, and supportive care. The patient’s PV required careful management, including aggressive hydration and close monitoring of hematocrit levels. He responded favorably to treatment, but experienced a prolonged recovery time due to the severity of the COVID-19 infection. The case highlights the importance of vigilant monitoring for thrombotic complications in patients with PV who contract COVID-19. |
Case Study 2: Treatment and Management
Effective management of PV during a COVID-19 infection requires a multi-faceted approach, addressing both the acute viral illness and the underlying hematological condition.
| Patient Demographics | Symptoms | Treatment Outcomes |
|---|---|---|
| 42-year-old female with PV, diagnosed 2 years prior, maintaining stable hematocrit levels with medication. | Developed mild COVID-19 symptoms, including fever and fatigue, along with increased blood viscosity. PV management was adjusted to reduce the risk of thrombotic complications. | The patient was monitored closely, and her PV medication regimen was adjusted to prevent blood clot formation. Her COVID-19 infection was managed with antiviral therapy, supportive care, and close monitoring of her hematological parameters. The patient recovered fully within a few weeks, with her PV remaining well-controlled. This case illustrates the importance of adjusting PV treatment strategies during a COVID-19 infection. |
Case Study 3: Long-Term Health Impacts
Long-term complications following a COVID-19 infection in patients with PV are a significant concern. These potential impacts necessitate careful consideration and proactive monitoring.
| Patient Demographics | Symptoms | Treatment Outcomes |
|---|---|---|
| 68-year-old male with PV, diagnosed 10 years prior, experiencing some functional decline. | Developed severe COVID-19, requiring mechanical ventilation and ICU admission. Post-COVID-19, the patient experienced fatigue, dyspnea, and cognitive impairment, which may have been influenced by both the infection and his pre-existing PV. | The patient’s recovery was slow, and he experienced persistent fatigue and reduced exercise tolerance. Further assessments were conducted to evaluate the extent of long-term COVID-19 effects. The case highlights the importance of long-term follow-up and rehabilitation for patients with PV who experience severe COVID-19. |
Prevention Strategies: Polycythemia And Coronavirus Covid 19 Risks Complications Considerations
Navigating the complexities of polycythemia vera (PV) and COVID-19 requires a proactive approach to prevention. Understanding the heightened risks associated with PV and the potential for severe COVID-19 complications is crucial for patients and healthcare providers. This section Artikels strategies to mitigate these risks.
Recommendations for Preventing COVID-19 in Patients with PV
Patients with PV should prioritize adherence to established public health guidelines to minimize COVID-19 exposure. These guidelines, while applicable to the general population, warrant particular attention in PV due to the potential for complications.
Importance of Adherence to Public Health Guidelines
Adherence to public health guidelines is paramount in preventing the spread of COVID-19. This includes consistent hand hygiene, wearing masks in public settings, maintaining social distancing, and getting vaccinated. Vaccination, in particular, is a cornerstone of preventative measures.
Potential Barriers to Preventative Measures in this Patient Population
Several factors can hinder the implementation of preventative measures in patients with PV. These may include underlying health conditions, reduced mobility, socioeconomic factors, and limited access to resources. Furthermore, the potential for fatigue and other symptoms associated with PV could impact adherence to preventative measures.
Summary of Preventive Measures, Polycythemia and coronavirus covid 19 risks complications considerations
| Preventive Measure | Effectiveness | Considerations for Patients with PV |
|---|---|---|
| Vaccination | Highly effective in reducing severe illness and death. | Patients with PV should discuss vaccination schedules and potential interactions with their medications with their healthcare providers. |
| Hand Hygiene | Crucial in preventing the spread of the virus. | Patients with PV should be reminded of the importance of hand hygiene, including frequent handwashing with soap and water or use of hand sanitizer. |
| Mask Wearing | Reduces the transmission of respiratory droplets. | Patients with PV should be advised on proper mask usage and comfort levels. They should also be aware of the potential for breathing difficulties. |
| Social Distancing | Limits close contact with others. | Patients with PV should be advised on maintaining safe distances, and consider the limitations of social distancing in daily life. |
| Avoiding Crowded Places | Reduces exposure to the virus. | This can be challenging for some patients, and accommodations may be necessary. |
| Quarantine/Isolation | Essential for preventing transmission. | Patients with PV should understand the importance of isolation when exposed to or diagnosed with COVID-19. Coordination with healthcare providers is essential. |
Ultimate Conclusion
In conclusion, the combination of polycythemia vera and COVID-19 presents a unique set of challenges demanding careful consideration. The potential for increased complications, thrombotic events, and severe COVID-19 outcomes necessitates a proactive approach to management and prevention. Close monitoring, tailored treatment strategies, and adherence to public health guidelines are crucial in mitigating risks and ensuring the best possible outcomes for individuals facing these intertwined conditions.