Monoclonal gammopathy of undetermined significance (MGUS) is a condition where a type of protein called a monoclonal immunoglobulin is produced in excess in the blood. While often asymptomatic, MGUS can sometimes progress into more serious conditions like multiple myeloma. Understanding the characteristics, diagnostics, and management strategies for MGUS is crucial for both patients and healthcare professionals.
This blog post dives into the intricacies of MGUS, exploring its definition, diagnostic criteria, risk factors, management strategies, and potential complications. We’ll also touch on the ongoing research in this field and what the future might hold for individuals diagnosed with MGUS.
Definition and Overview
Monoclonal gammopathy of undetermined significance (MGUS) is a condition characterized by the presence of a monoclonal protein (M protein) in the blood. This M protein is produced by a clone of plasma cells, a type of white blood cell. While the presence of this M protein signifies a potential for a more serious condition, the significance remains uncertain, hence the “undetermined” designation.
It’s crucial to distinguish MGUS from other related conditions like multiple myeloma, Waldenström macroglobulinemia, and amyloidosis, as these have different clinical courses and treatments.
Monoclonal gammopathy of undetermined significance (MGUS) is a condition where your body produces too much of a specific type of antibody. Sometimes, these excess antibodies can be linked to various prescription and otc drugs prescription and otc drugs , potentially contributing to the abnormal protein levels. While the exact causes of MGUS are still being researched, it’s important to be aware of the potential interactions between medications and this condition.
Distinguishing Characteristics of MGUS
MGUS is distinct from other plasma cell dyscrasias due to several key factors. The levels of monoclonal protein are typically lower, and the bone marrow involvement is minimal. Furthermore, patients with MGUS usually exhibit no apparent symptoms or signs of disease, which can sometimes lead to delayed diagnosis. This lack of obvious symptoms is a significant distinguishing factor from more aggressive conditions.
Typical Presentation of MGUS
Patients with MGUS often present with no noticeable symptoms. This asymptomatic nature is common and often leads to the condition being discovered incidentally during routine blood tests or screenings for other conditions. Sometimes, patients may report nonspecific symptoms like fatigue or bone pain, but these are often mild and can be easily attributed to other causes.
Prevalence and Incidence of MGUS
MGUS is relatively common, affecting approximately 3% of adults over the age of 50 in the United States. The prevalence increases with age, indicating a higher risk of developing MGUS in older individuals. The incidence rates are also higher in males compared to females. This higher prevalence underscores the importance of regular health screenings for individuals at risk.
Monoclonal gammopathy of undetermined significance (MGUS) is something I’ve been researching lately. It’s often a silent condition, but it can sometimes lead to complications like skin problems, which are frequently associated with other health issues. For instance, if you have diabetes, certain skin conditions are more common, such as those related to diabetes and skin problems.
Thankfully, MGUS is often managed without significant intervention, but it’s important to be aware of the potential connections to other health concerns.
Potential Clinical Significance of MGUS
While initially asymptomatic, MGUS carries a potential for progression to more aggressive plasma cell dyscrasias, such as multiple myeloma. This progression is slow and not all cases progress. Careful monitoring and regular follow-up are crucial to detect any signs of progression. The risk of progression is influenced by factors such as the level of monoclonal protein, the type of immunoglobulin involved, and the patient’s age.
Key Differences Between MGUS and Multiple Myeloma
| Characteristic | MGUS | Multiple Myeloma |
|---|---|---|
| Monoclonal Protein Level | Low (typically less than 3 g/dL) | High (typically greater than 3 g/dL) |
| Bone Marrow Involvement | Minimal | Significant |
| Symptoms | Usually asymptomatic | Often symptomatic (bone pain, fatigue, etc.) |
| Progression to Myeloma | Potential, but slow | High risk of progression |
| Life Expectancy | Generally normal with careful monitoring | Reduced life expectancy if not treated |
The table above summarizes the critical distinctions between MGUS and multiple myeloma. These differences are essential for appropriate diagnosis and management strategies. It’s vital to remember that these are general guidelines, and individual cases may vary. Consultation with a healthcare professional is essential for accurate diagnosis and personalized management.
Diagnostic Criteria and Procedures
Monoclonal gammopathy of undetermined significance (MGUS) is a condition characterized by the presence of a monoclonal protein (M-protein) in the blood, but without the signs or symptoms of multiple myeloma or other related disorders. Accurate diagnosis is crucial for appropriate management and to differentiate MGUS from more serious conditions. Early detection and monitoring are essential to identify potential progression to a more aggressive form of the disease.
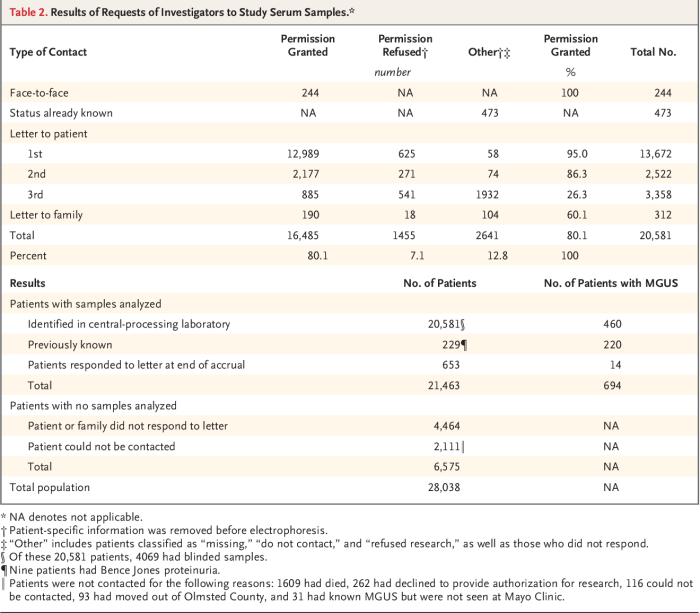
Diagnostic Criteria for MGUS, Monoclonal gammopathy of undetermined significance
MGUS is diagnosed based on specific criteria established by expert consensus. These criteria help clinicians distinguish MGUS from other conditions that might present with similar laboratory findings. These criteria focus on the levels and characteristics of the monoclonal protein in the blood and urine, along with the absence of organ damage. Failure to meet these criteria would indicate further investigation is needed.
Laboratory Tests for MGUS Diagnosis
Several laboratory tests play a crucial role in diagnosing MGUS. These tests are essential to detect the presence of monoclonal proteins, measure their concentration, and assess their characteristics.
- Serum Protein Electrophoresis (SPEP): This is a fundamental test that separates serum proteins based on their electrical charge. An abnormal peak, indicative of an M-protein, is a key indicator. This test helps identify the presence and approximate amount of the monoclonal protein.
- Immunofixation Electrophoresis (IFE): This technique builds on SPEP by further characterizing the M-protein. It identifies the specific type of immunoglobulin (e.g., IgG, IgA, IgM) and the light chain involved (kappa or lambda). This crucial information aids in distinguishing MGUS from other conditions with similar findings.
- Serum and Urine Protein Quantification: Measuring the total amount of protein in the serum and urine helps assess the concentration of the M-protein. Specific quantification of the M-protein is important for meeting diagnostic criteria.
- Complete Blood Count (CBC): This test assesses overall blood cell counts, which can provide insights into the patient’s general health and detect any potential complications related to the condition.
Imaging Techniques in Assessing MGUS
Imaging techniques are typically not the first-line diagnostic tools for MGUS. Their role is primarily in evaluating for complications or organ involvement, and are typically not required for diagnosis. However, these tests may be used to assess the extent of any potential complications.
- Bone X-rays: These are used to evaluate for lytic bone lesions, a hallmark of multiple myeloma. The absence of these lesions in patients suspected of having MGUS is a supportive finding.
- Bone Scans: These scans can detect subtle areas of bone damage not visible on X-rays. Their use is often reserved for cases where there’s a suspicion of bone involvement.
- MRI or CT Scans: These imaging techniques are used to evaluate the soft tissues and organs for involvement. In cases of MGUS, the presence or absence of organ involvement helps distinguish it from other related conditions.
Steps in the Diagnostic Workup for MGUS
The diagnostic workup for a suspected case of MGUS typically involves a systematic approach.
- Detailed Patient History and Physical Examination: A comprehensive history, including symptoms, medical history, and family history, is crucial for understanding the patient’s overall health status and ruling out other possible conditions.
- Laboratory Tests: This step involves performing SPEP and IFE to detect the presence of M-protein. Serum and urine protein quantification are also conducted to determine the exact concentration of the monoclonal protein. Other relevant blood tests, such as a CBC, are also part of the initial assessment.
- Imaging Studies (if indicated): If there are concerns about organ involvement or bone lesions, imaging studies like bone X-rays, bone scans, or CT scans may be performed to evaluate for any abnormalities.
- Bone Marrow Biopsy (if indicated): In some cases, a bone marrow biopsy might be necessary to rule out other conditions or to assess the extent of any underlying disease.
| Diagnostic Criterion | Description |
|---|---|
| Monoclonal protein (M-protein) in serum | Presence of an abnormal protein peak on serum protein electrophoresis (SPEP). |
| Absence of myeloma-defining events | No evidence of organ damage or other features indicative of multiple myeloma. |
| No evidence of other related plasma cell disorders | No signs of other conditions that might explain the presence of the monoclonal protein. |
Risk Factors and Associated Conditions
Monoclonal gammopathy of undetermined significance (MGUS) is a perplexing condition, and while its precise causes remain elusive, certain factors increase the likelihood of its development. Understanding these risk factors is crucial for both prevention and early detection. This section delves into potential predisposing elements, connections to other hematological conditions, and the observed variations in prevalence across different populations.
Potential Risk Factors
Several factors may elevate an individual’s susceptibility to MGUS. Age is a significant contributor, with the risk increasing substantially as individuals age. A strong genetic component is also recognized, suggesting a familial predisposition. Environmental exposures, while not definitively proven, might play a role. Certain lifestyle factors, such as smoking history, could also influence the risk, although more research is needed to fully understand these relationships.
Monoclonal gammopathy of undetermined significance (MGUS) is a condition where your body produces too many of one type of antibody. While often harmless, it’s important to be aware of the potential for it to progress to something more serious. Learning more about similar conditions, like the various facts about parkinsons disease , can be fascinating and shed light on the complexities of the human body.
Understanding these connections helps in managing the potential health concerns related to MGUS.
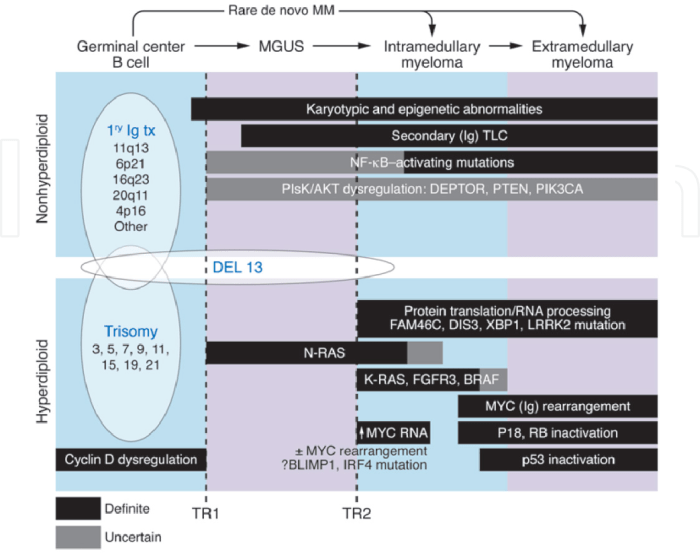
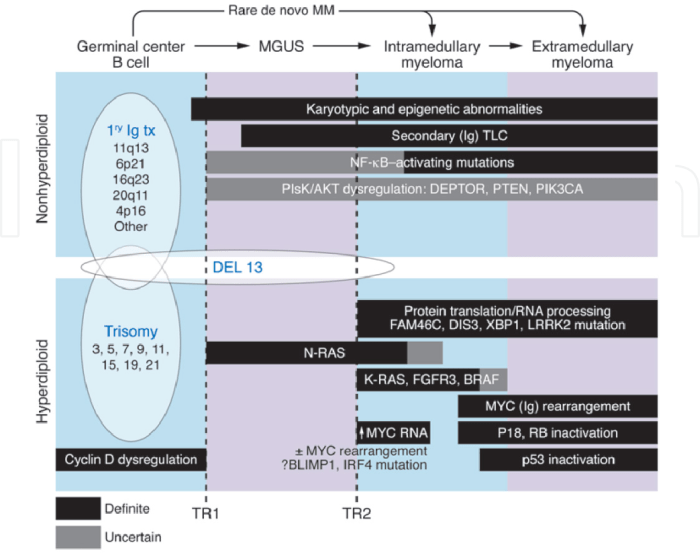
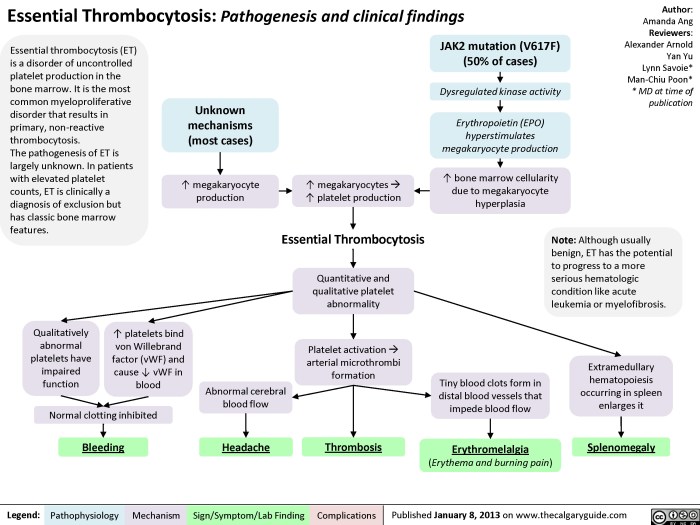
Link Between MGUS and Hematological Malignancies
A crucial aspect of MGUS is its potential progression to more serious hematological malignancies, including multiple myeloma. While MGUS itself is not a malignant condition, a substantial proportion of individuals with MGUS eventually develop multiple myeloma. This progression isn’t uniform; some individuals with MGUS remain stable, while others may experience a transition to a more aggressive form of the disease.
The risk of progression is often assessed based on the characteristics of the monoclonal protein and the overall clinical presentation.
Prevalence in Different Populations
The prevalence of MGUS varies across different populations. Studies have shown that certain ethnic groups may exhibit higher rates compared to others. This variation could be attributed to a combination of genetic predispositions and environmental factors. For instance, a study might reveal a higher prevalence of MGUS in individuals of African descent compared to those of European descent.
However, it’s important to note that these findings are still under investigation, and further research is needed to establish definitive correlations.
Genetic Predisposition
Genetic factors are believed to contribute to the development of MGUS. Family history of MGUS or other related conditions may suggest a hereditary component. Further research into specific genetic markers is ongoing, aiming to identify potential susceptibility genes and potentially offer early diagnostic tools. For example, if a parent has MGUS, their children might have an increased likelihood of developing the condition.
Risk Factor Impact on MGUS Progression
| Risk Factor | Potential Impact on MGUS Progression |
|---|---|
| Age | Increased risk of progression to multiple myeloma. |
| Elevated monoclonal protein levels | Higher risk of progression to multiple myeloma. |
| Presence of specific genetic markers | Potentially increased risk of progression to multiple myeloma. |
| Family history of MGUS or multiple myeloma | Increased risk of developing MGUS or progression to multiple myeloma. |
| Smoking history | Potential but not definitively proven increased risk of progression. |
Management and Prognosis: Monoclonal Gammopathy Of Undetermined Significance
Monoclonal gammopathy of undetermined significance (MGUS) is often a condition that requires careful monitoring rather than aggressive treatment. Understanding the management strategies and the potential for progression is crucial for patients and their healthcare providers. The key is to watch for any signs of progression to a more serious condition like multiple myeloma, while maintaining a good quality of life.
Common Management Strategies for MGUS
MGUS is typically managed by a watchful waiting approach. This involves monitoring the disease and intervening only if it progresses. Regular blood tests and urine tests are vital for detecting any changes in the levels of monoclonal protein. These tests help track the disease’s stability or potential progression. Treatment is not usually initiated unless the condition advances to a more serious form, such as multiple myeloma.
However, certain risk factors, like high levels of monoclonal protein, can influence the management plan.
Monitoring Protocols for MGUS Patients
Regular monitoring is essential for managing MGUS effectively. Monitoring protocols aim to detect early signs of progression to multiple myeloma. The protocols typically involve a combination of blood tests, urine tests, and sometimes, imaging studies. The frequency of these tests depends on the individual patient’s risk factors and the initial levels of monoclonal protein. The goal is to identify any significant changes that may signal progression.
For instance, a significant increase in monoclonal protein levels might necessitate a more intensive monitoring schedule.
Prognosis for Individuals with MGUS
The prognosis for individuals with MGUS is generally good. Most people with MGUS do not develop multiple myeloma. However, the risk of progression does exist, and it’s crucial to understand the factors influencing this progression. The prognosis depends largely on factors such as the level of monoclonal protein and the rate of increase in its level. For example, a patient with a low level of monoclonal protein and stable levels over time has a more favorable prognosis than someone with high levels and increasing protein.
Factors Influencing the Progression of MGUS
Several factors can influence the progression of MGUS to multiple myeloma. High levels of monoclonal protein, rapid increases in protein levels, and the presence of other related conditions can all contribute to a higher risk of progression. Moreover, age and genetic factors play a role, though the exact nature of these influences is still under investigation. Understanding these factors allows for personalized monitoring strategies and better risk assessment.
Summary of Monitoring Intervals for MGUS
| Risk Factor | Initial Monitoring Interval | Monitoring Interval if Protein Levels Increase | Monitoring Interval if Symptoms Appear |
|---|---|---|---|
| Low level monoclonal protein, stable levels | Annually | Every 6 months | Monthly |
| Moderate level monoclonal protein, slow increase | Every 6 months | Quarterly | Bi-monthly |
| High level monoclonal protein, rapid increase | Quarterly | Monthly | Weekly |
Note: This table is a general guideline and individual monitoring intervals may vary based on specific circumstances. Consult with your physician for personalized recommendations.
Treatment Options and Approaches
Monoclonal Gammopathy of Undetermined Significance (MGUS) is often a benign condition, but in some cases, it can progress to more serious diseases like multiple myeloma. Understanding treatment approaches for potential progression is crucial for managing patient care effectively. The key is early detection and proactive management to minimize complications and improve outcomes.Treatment for MGUS, particularly in cases of progression, focuses on slowing or preventing the disease from advancing.
The rationale behind various strategies stems from the understanding of the underlying mechanisms driving the disease’s progression. Crucially, treatment decisions must consider the individual patient’s characteristics, including the stage of disease, overall health, and preferences. This personalized approach ensures the most effective and tolerable treatment plan.
Treatment Approaches for MGUS Progression
The primary goal in treating MGUS progression is to slow the disease’s progression and prevent the development of more aggressive forms of plasma cell disorders. This is achieved through various strategies, each with its own rationale and potential side effects. Crucially, treatment decisions should always be individualized and carefully weighed against the potential benefits and risks.
Rationale Behind Treatment Strategies
Treatment strategies for MGUS progression are driven by the goal of reducing the risk of malignant transformation. Several factors influence the choice of therapy. These include the extent of disease progression, the patient’s overall health status, and the potential side effects of the treatment. The aim is to maximize efficacy while minimizing toxicity. For example, in cases where there is a significant risk of progression, more aggressive treatment may be warranted, even if the potential side effects are greater.
Comparison of Treatment Options Based on Patient Characteristics
Treatment selection for MGUS progression is not a one-size-fits-all approach. The choice of therapy depends on a number of factors, including the patient’s age, overall health, the extent of the disease, and the presence of any other co-morbidities. For example, younger patients with less severe disease may be suitable for less intensive interventions, whereas older patients with more advanced disease may benefit from a more conservative approach.
Potential Side Effects of Treatment Approaches
Any treatment for MGUS progression, especially those targeting plasma cells, can have potential side effects. These may range from mild, temporary discomfort to more serious, long-term complications. Common side effects can include fatigue, nausea, hair loss, and increased risk of infection. Moreover, some treatments can impact bone marrow function, potentially leading to anemia or thrombocytopenia.
Efficacy and Safety Comparison of Treatment Modalities
| Treatment Modality | Efficacy | Safety Profile | Considerations |
|---|---|---|---|
| Immunomodulatory drugs (IMiDs) | Demonstrated effectiveness in reducing plasma cell burden and slowing disease progression in some cases. | Potential for significant side effects, including fatigue, nausea, and peripheral neuropathy. | Generally reserved for cases of significant disease progression. |
| Bortezomib (Velcade) | Showed promising results in reducing plasma cell counts in clinical trials. | May cause peripheral neuropathy, renal impairment, and gastrointestinal issues. | Often considered a more aggressive option, suitable for patients with significant disease burden and a high risk of progression. |
| Thalidomide | Potentially effective in slowing disease progression. | Significant side effects, including peripheral neuropathy and teratogenicity. | Should be used cautiously, and only in specific circumstances. |
| Supportive care | Focuses on managing symptoms and maintaining quality of life. | Generally well-tolerated, with minimal side effects. | Often the primary approach for patients with less aggressive disease or who are not suitable for aggressive therapies. |
Complications and Long-Term Outcomes
Monoclonal Gammopathy of Undetermined Significance (MGUS) is often a benign condition, but it can sometimes lead to complications. Understanding these potential issues and their impact on quality of life is crucial for effective management and patient support. Knowing the possible progression to more serious conditions is key to navigating this situation.While MGUS typically doesn’t cause immediate symptoms, it carries a risk of progression to more serious plasma cell disorders, such as multiple myeloma.
Careful monitoring and understanding of potential complications are vital for individuals diagnosed with MGUS.
Potential Complications of MGUS
MGUS, though initially asymptomatic, can progress to more serious conditions. A crucial aspect of management is recognizing these potential complications and understanding the risk factors associated with their development. This allows for early intervention and potentially better outcomes.
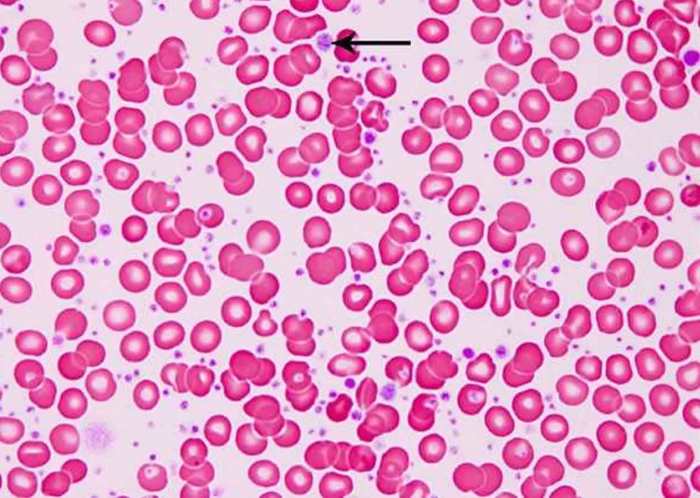
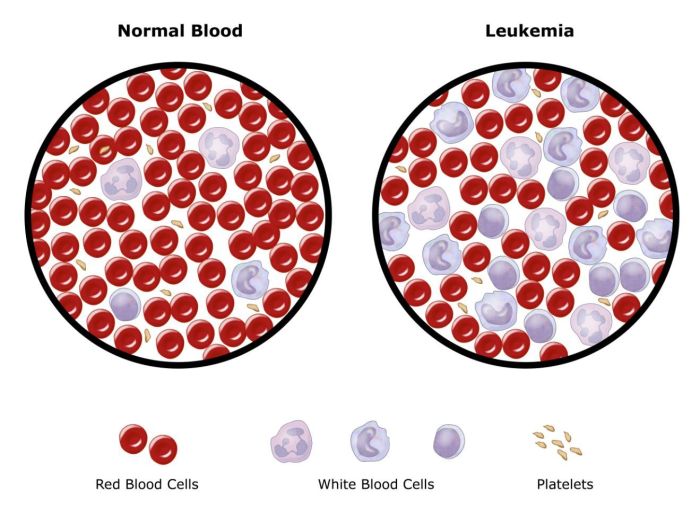
- Progression to Multiple Myeloma: The most significant risk associated with MGUS is its potential progression to multiple myeloma. This malignancy is characterized by the uncontrolled proliferation of plasma cells, leading to bone damage, organ dysfunction, and a range of other complications. While not all individuals with MGUS will develop multiple myeloma, the risk exists and requires careful monitoring.
- Amyloidosis: In some cases, MGUS can lead to amyloidosis, a condition where abnormal proteins called amyloid fibrils accumulate in various organs, causing organ damage. The specific organs affected and the severity of the condition can vary greatly, but amyloidosis can be a serious complication. A real-life example of this complication is a case where a patient with MGUS developed amyloid deposits in their heart, causing significant cardiac dysfunction.
- Bone Disease: The presence of abnormal plasma cells can lead to bone lesions and fractures. The accumulation of abnormal cells in the bone marrow can lead to a variety of complications, ranging from bone pain to pathologic fractures. This can significantly impact mobility and overall quality of life.
- Peripheral Neuropathy: In some instances, the abnormal proteins associated with MGUS can affect the nerves, leading to peripheral neuropathy. This can manifest as numbness, tingling, or pain in the extremities and can significantly impact daily activities.
Long-Term Outcomes for Individuals with MGUS
The long-term outcomes for individuals with MGUS vary greatly depending on several factors. The presence of risk factors, the individual’s overall health, and the aggressiveness of monitoring play a key role in determining the trajectory of the disease.
- Variable Progression: It’s crucial to understand that the progression from MGUS to a more serious condition is not predictable. Some individuals with MGUS may remain stable for years, while others may experience progression more rapidly. This highlights the importance of regular monitoring and personalized management strategies.
- Impact on Quality of Life: The impact of MGUS on quality of life can be significant, particularly as the condition progresses. Factors such as fatigue, pain, and functional limitations can affect a patient’s ability to participate in daily activities and maintain a healthy lifestyle.
Strategies for Mitigating Complications in MGUS
Early detection and regular monitoring are crucial for managing MGUS effectively and mitigating the risk of complications. A proactive approach to management can significantly improve the long-term outcomes.
- Regular Monitoring: Regular blood tests and monitoring of the abnormal protein levels are essential for detecting any changes that might indicate progression to a more serious condition. This allows for early intervention and treatment if needed.
- Personalized Management: Individualized management plans are vital for optimizing care. These plans should take into account the patient’s risk factors, overall health, and preferences. The patient and their healthcare provider should work together to develop a comprehensive plan that balances the need for monitoring with the patient’s lifestyle.
Frequency and Severity of Complications in MGUS
The frequency and severity of complications in MGUS vary widely. It’s crucial to remember that not everyone with MGUS will develop complications. The risk is influenced by multiple factors.
| Complication | Frequency (estimated) | Severity |
|---|---|---|
| Progression to Multiple Myeloma | 1-10% per year | High, potentially life-threatening |
| Amyloidosis | Rare | Potentially life-threatening |
| Bone Disease | Variable | Moderate to severe |
| Peripheral Neuropathy | Rare | Variable |
Research and Future Directions
Monoclonal Gammopathy of Undetermined Significance (MGUS) research is actively exploring the intricate mechanisms driving its development and progression. Understanding these mechanisms is crucial for developing targeted therapies and potentially preventing the progression to more serious conditions like multiple myeloma. This exploration is leading to promising avenues of investigation, which are likely to shape future management strategies for MGUS.
Current Research on MGUS Mechanisms
Current research into the underlying mechanisms of MGUS is focused on identifying specific genetic and environmental factors that contribute to the development and progression of the disease. Researchers are investigating the role of immune dysregulation, genetic mutations, and inflammation in the abnormal proliferation of plasma cells that characterizes MGUS. Studies are also exploring the influence of epigenetic modifications on the expression of genes involved in plasma cell differentiation and survival.
Promising Areas of Research
Several promising research areas hold significant potential for advancing our understanding of MGUS and improving its management. These include:
- Targeting specific molecular pathways: Identifying key molecular pathways involved in the development and progression of MGUS is crucial for the development of targeted therapies. Researchers are investigating the roles of signaling pathways, such as the NF-κB pathway, and growth factors, such as IL-6, in the abnormal proliferation of plasma cells.
- Developing diagnostic tools: More accurate and early diagnostic tools are needed to identify individuals at risk of developing MGUS and monitor disease progression. Researchers are exploring new biomarkers, such as specific protein profiles in blood and urine, that can potentially aid in earlier diagnosis and risk stratification.
- Understanding the role of the microenvironment: The interactions between plasma cells and the surrounding cells in the bone marrow (the microenvironment) play a crucial role in MGUS pathogenesis. Further research into this microenvironment could reveal novel therapeutic targets and improve the prediction of disease progression.
Areas Needing Further Research
Despite progress, several areas require further investigation to fully understand MGUS and develop effective interventions. These include:
- Longitudinal studies: Large-scale longitudinal studies are needed to better understand the natural history of MGUS, including the factors that influence progression to myeloma or other diseases. These studies will help refine risk stratification models and identify individuals who are at higher risk for progression.
- Identifying preventative measures: Research on lifestyle factors, environmental exposures, and other potential preventative measures could potentially contribute to delaying or preventing the development of MGUS.
- Developing effective preventive strategies: Research is needed to explore the possibility of interventions to prevent the progression of MGUS to myeloma, such as immunomodulatory therapies or targeted therapies. This could potentially lead to a paradigm shift in MGUS management.
Potential Future Directions in MGUS Management
Future directions in MGUS management may involve personalized medicine approaches, focusing on identifying individuals at high risk of progression and tailoring interventions accordingly. This personalized approach could include using genetic and molecular profiling to identify specific risk factors and predict the likelihood of progression in each individual patient. This precision medicine approach could also lead to the development of more effective targeted therapies.
Key Areas of MGUS Research
| Research Area | Description | Potential Impact |
|---|---|---|
| Molecular Mechanisms | Identifying key molecular pathways and genetic alterations driving MGUS development and progression. | Development of targeted therapies and biomarkers for early diagnosis. |
| Diagnostic Tools | Development of more sensitive and specific diagnostic tools for early detection and risk stratification. | Improved patient selection for appropriate interventions and better monitoring of disease progression. |
| Microenvironment Interactions | Understanding the interactions between plasma cells and the bone marrow microenvironment. | Identification of novel therapeutic targets and potential preventive strategies. |
| Longitudinal Studies | Large-scale studies to assess the natural history of MGUS and identify factors associated with progression. | Improved risk stratification models and understanding of disease progression. |
Final Wrap-Up
In conclusion, monoclonal gammopathy of undetermined significance (MGUS) presents a complex medical landscape. While often initially benign, its potential to progress necessitates careful monitoring and management. This post has provided a comprehensive overview of the condition, from its definition to potential complications and future research. Understanding the nuances of MGUS is vital for patients, healthcare providers, and anyone interested in this fascinating area of hematology.



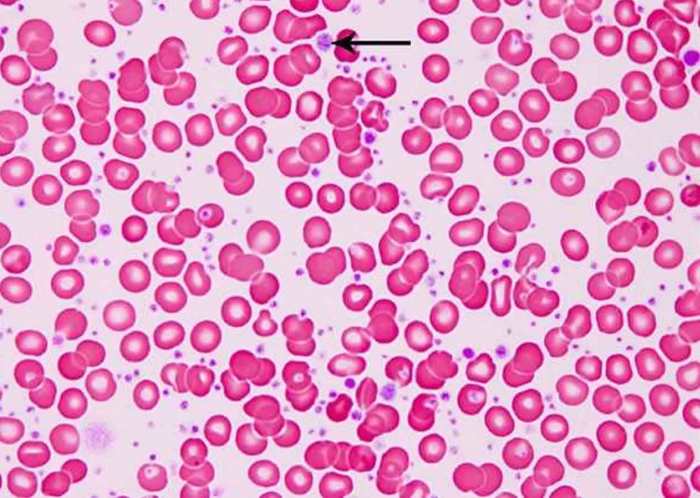
/leukemia-myeloid-250x-at-35mm-this-type-of-leukemia-has-its-origin-in-the-bone-marrow-myeloid-tissue-it-involves-a-malignant-proliferation-of-immature-white-blood-cells-this-action-can-crowd-out-production-of-rbc-s-and-platelets-leading-to-an--58aca68c3df78c345b81d051.jpg?w=700)
