Autoimmunity neuroinflammation in fibromyalgia is a fascinating and complex area of research. This condition, characterized by widespread pain and fatigue, is increasingly understood to involve interactions between the immune system and the nervous system. We’ll delve into the potential mechanisms by which these processes intertwine, exploring the suspected roles of autoimmunity and neuroinflammation in the development and progression of fibromyalgia.
The suspected involvement of both autoimmunity and neuroinflammation in fibromyalgia paints a picture of a multifaceted disorder. This post will explore the potential mechanisms, diagnostic challenges, and potential therapeutic targets for managing this complex condition. We’ll investigate how the immune system might target healthy tissues, examine the inflammatory processes in the nervous system, and analyze the potential overlap between these processes.
Autoimmunity and Neuroinflammation in Fibromyalgia: A Deeper Look
Fibromyalgia, a chronic condition characterized by widespread pain and fatigue, is a complex illness with a still-unclear etiology. While the exact mechanisms driving this debilitating syndrome remain elusive, mounting evidence points towards the involvement of both autoimmunity and neuroinflammation. These processes are not mutually exclusive but rather appear to interact in intricate ways to contribute to the disease’s development and progression.
Understanding these interactions is crucial for developing more effective treatments and management strategies.
Defining Autoimmunity and Neuroinflammation
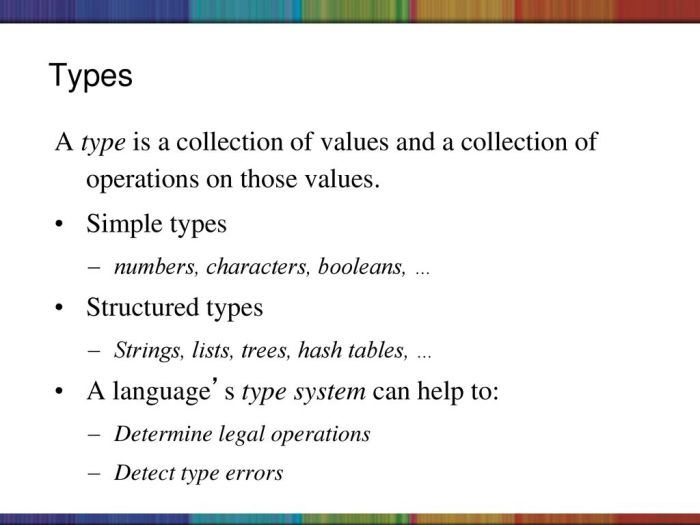
Autoimmunity is an immune system malfunction where the body mistakenly attacks its own tissues and organs. This results in chronic inflammation and tissue damage. Neuroinflammation, on the other hand, is inflammation of the nervous system. It’s a complex process involving the activation of immune cells within the brain and spinal cord, leading to a cascade of events that can damage nerve cells and disrupt normal neurological function.
The Suspected Roles in Fibromyalgia
Research suggests that both autoimmunity and neuroinflammation play critical roles in the development and progression of fibromyalgia. Autoimmune responses, potentially triggered by environmental factors or genetic predispositions, might initiate a cascade of events that contribute to chronic pain and fatigue. This cascade can involve the release of inflammatory cytokines and other molecules, setting the stage for neuroinflammation. Neuroinflammation, in turn, can further exacerbate the pain signals, leading to a vicious cycle of pain, inflammation, and dysfunction.
Studies have shown elevated levels of inflammatory markers in fibromyalgia patients, supporting the involvement of these processes. Furthermore, the central sensitization hypothesis suggests that neuroinflammation can lead to increased pain perception and amplification of pain signals, which aligns with the chronic pain experienced by fibromyalgia patients.
Complex Interplay Between Autoimmunity and Neuroinflammation
The interplay between autoimmunity and neuroinflammation in fibromyalgia is intricate and not fully understood. The precise sequence of events remains a subject of ongoing research. It is hypothesized that autoimmune responses may trigger a cascade of events leading to neuroinflammation, or that neuroinflammation can create an environment that further promotes autoimmune reactions. For instance, chronic inflammation might make the body more susceptible to autoimmune attacks, while ongoing autoimmune processes might in turn exacerbate the inflammatory response within the nervous system.
Key Symptoms Associated with Autoimmunity and Neuroinflammation
| Symptom | Autoimmunity | Neuroinflammation | Fibromyalgia |
|---|---|---|---|
| Pain | Widespread, often localized to specific organs/joints | Chronic, often widespread, can be neuropathic | Widespread, chronic, often described as deep, aching, and fatigue-inducing |
| Fatigue | Variable, can be severe, often accompanied by other symptoms | Variable, can be severe, often related to sleep disruption | Severe, persistent, and often disproportionate to physical activity |
| Muscle Stiffness | Can occur in response to tissue damage | Can result from nerve damage or dysfunction | Common, often described as a feeling of tightness or soreness |
| Cognitive Dysfunction | Possible, depending on the affected organs | Common, including difficulty concentrating, memory problems, and brain fog | Frequent, impacting daily activities and quality of life |
| Sleep Disturbances | Potential, due to pain and other symptoms | Directly related to inflammation and nerve dysfunction | Common, characterized by difficulty falling asleep, staying asleep, or experiencing restorative sleep |
Mechanisms of Autoimmunity in Fibromyalgia: Autoimmunity Neuroinflammation In Fibromyalgia
The intricate dance of the immune system in fibromyalgia remains a significant mystery, though growing evidence points to a potential role for autoimmunity. This exploration delves into the potential mechanisms by which the immune system may target healthy tissues in fibromyalgia, along with potential triggers and comparisons to other chronic pain conditions.The precise mechanisms driving autoimmune responses in fibromyalgia are not fully understood, but various hypotheses are being investigated.
These hypotheses suggest a complex interplay of genetic predisposition, environmental factors, and possibly even infections, contributing to the development of the condition.
Potential Mechanisms of Immune System Misdirection
The immune system normally distinguishes between self and non-self, attacking foreign invaders like bacteria and viruses while leaving healthy tissues alone. However, in fibromyalgia, this delicate balance might be disrupted, leading to the mistaken identification and attack of healthy tissues. This could manifest as the production of autoantibodies, which are antibodies that mistakenly target the body’s own tissues, or through the activation of immune cells that attack and damage these tissues.
Potential Triggers for Autoimmune Responses
Several factors could potentially trigger or contribute to autoimmune responses in fibromyalgia. These may include infections, particularly viral infections, and environmental toxins. Genetic predisposition plays a critical role in susceptibility, as individuals with certain genetic variations may be more prone to developing autoimmune responses. Stress and hormonal imbalances may also contribute to the activation of the immune system.
Comparison with Other Chronic Pain Conditions
While the precise mechanisms differ, some overlap exists between fibromyalgia and other chronic pain conditions, such as rheumatoid arthritis and lupus. These conditions share features like chronic inflammation and immune system dysfunction, though the specific targets and triggers might vary. For example, in rheumatoid arthritis, the immune system primarily targets the joints, while in lupus, a wider range of tissues and organs are affected.
This demonstrates the complex nature of autoimmune responses and the need for further research to fully understand the nuances within each condition.
Immune Cell Involvement in Proposed Autoimmune Responses
Understanding the specific immune cells involved in potential autoimmune responses in fibromyalgia is crucial for developing targeted therapies. The table below summarizes the key immune cell types implicated in the proposed mechanisms.
| Immune Cell Type | Potential Role in Fibromyalgia |
|---|---|
| T cells (especially CD4+ T cells) | These cells can be activated and release inflammatory cytokines, which contribute to tissue damage. They may also play a role in autoantibody production. |
| B cells | These cells produce autoantibodies that target healthy tissues, leading to inflammation and damage. |
| Macrophages | These cells are involved in inflammation and tissue damage. Their activation and release of inflammatory mediators can play a crucial role. |
| Natural Killer (NK) cells | These cells can target and kill cells in the body, potentially leading to tissue damage. |
Note: This table provides a general overview. The specific roles and interactions of these immune cells in fibromyalgia are still being investigated.
Dealing with autoimmunity neuroinflammation in fibromyalgia can be tough, but staying active is key. Building strength, especially in your legs, can really help manage symptoms. For example, incorporating some favorite leg strengthening exercises into your routine can improve your overall well-being and potentially reduce the impact of the inflammation. Ultimately, finding what works best for you is crucial in managing this complex condition.
Mechanisms of Neuroinflammation in Fibromyalgia
Fibromyalgia, a chronic pain condition, is characterized by widespread pain, fatigue, and a range of other symptoms. While the precise mechanisms underlying these symptoms remain incompletely understood, growing evidence points towards a significant role for neuroinflammation in the pathophysiology of fibromyalgia. This process, involving the nervous system’s response to perceived or actual injury, plays a crucial role in shaping the experience of pain and other debilitating symptoms.The nervous system, a complex network of cells, is constantly interacting with the body’s immune system.
When the immune system is activated, various inflammatory molecules, like cytokines, are released. These molecules can directly impact the nervous system, triggering a cascade of events that lead to pain sensitization, altered nerve function, and a persistent state of inflammation. This persistent neuroinflammation contributes to the chronic nature of fibromyalgia, creating a cycle of pain and dysfunction.
Neurotransmitter Dysfunction and Pain Perception
Neurotransmitters, chemical messengers within the nervous system, are vital for regulating pain perception. Neuroinflammation disrupts the delicate balance of these neurotransmitters, leading to alterations in pain processing. Specifically, elevated levels of inflammatory cytokines can interfere with the function of neurotransmitters like norepinephrine, serotonin, and glutamate. This disruption can lead to hypersensitivity to pain stimuli, making even mild sensations feel excruciating.
Furthermore, neuroinflammation can lead to changes in the density and function of pain receptors in the nervous system, increasing the sensitivity to pain.
Cytokine Involvement in Neuroinflammation
Cytokines are proteins that act as messengers within the immune system, orchestrating immune responses. Several studies have highlighted the crucial role of cytokines in the neuroinflammation associated with fibromyalgia. Examples of key cytokines include tumor necrosis factor-alpha (TNF-α), interleukin-1 beta (IL-1β), and interleukin-6 (IL-6). These cytokines can directly influence the nervous system by modulating the activity of glial cells, a type of supporting cell in the nervous system.
Glial cells, particularly microglia and astrocytes, play a critical role in maintaining the health and function of neurons. Their activation, in response to inflammatory cytokines, contributes to the neuroinflammatory process.
Evidence Supporting Neuroinflammation
There is mounting evidence supporting the role of neuroinflammation in the pathophysiology of fibromyalgia. Studies have demonstrated elevated levels of inflammatory markers, including cytokines, in the cerebrospinal fluid and blood of individuals with fibromyalgia compared to healthy controls. These elevated levels suggest a persistent state of neuroinflammation. Furthermore, animal models of fibromyalgia exhibit similar neuroinflammatory patterns, mimicking the pain and other symptoms observed in humans with fibromyalgia.
These findings provide compelling support for the involvement of neuroinflammation in the chronic pain experience of fibromyalgia.
Potential Pathways Contributing to Symptoms
Neuroinflammation can trigger a complex cascade of events, impacting various bodily functions and contributing to the diverse symptoms associated with fibromyalgia. The persistent activation of glial cells, for example, can disrupt the communication between neurons, leading to impaired cognitive function and sleep disturbances. The altered regulation of neurotransmitters, as mentioned earlier, can contribute to mood disorders and fatigue.
The interplay between neuroinflammation, the immune system, and the nervous system creates a complex interplay, making it challenging to isolate specific pathways responsible for each symptom.
Overlap and Interactions
Fibromyalgia is a complex disorder characterized by chronic widespread pain, fatigue, and a multitude of other symptoms. While the exact cause remains elusive, mounting evidence suggests a strong interplay between autoimmune and neuroinflammatory processes. Understanding how these two systems interact is crucial to developing effective treatment strategies. This section delves into the potential overlaps and mechanisms by which these processes influence each other, ultimately contributing to the chronic pain experienced in fibromyalgia.The overlap between autoimmune and neuroinflammatory processes in fibromyalgia is not simply coincidental.
Both pathways share common signaling molecules and cellular players, creating a feedback loop that can exacerbate the symptoms. This intricate dance between the immune and nervous systems may lead to sustained activation of pain pathways, contributing to the chronic and widespread nature of fibromyalgia pain.
Potential Mechanisms of Interaction
The immune system and nervous system are intricately connected, constantly exchanging signals. This intricate communication network is crucial for maintaining homeostasis and responding to threats. In fibromyalgia, this communication seems disrupted, potentially leading to a vicious cycle of inflammation and pain. The release of inflammatory cytokines, for instance, can directly impact nerve function, sensitizing nociceptors (pain receptors) and amplifying pain signals.
Conversely, the nervous system’s response can influence immune cell activity, further escalating the inflammatory cascade.
Immune Cell-Nervous System Interactions
The intricate dance between immune cells and the nervous system is pivotal in understanding fibromyalgia. Various immune cells, including macrophages, T cells, and microglia, play a crucial role in both inflammation and neurotransmission. These cells can interact directly with neurons, influencing their activity and potentially contributing to pain sensitization. Furthermore, these interactions can alter the production and release of neurotransmitters, such as substance P and glutamate, which are essential for pain signaling.
| Immune Cell | Nervous System Component | Potential Interaction |
|---|---|---|
| Macrophages | Nociceptors | Macrophages can release inflammatory cytokines that sensitize nociceptors, increasing pain perception. |
| T cells | Neurons | Activated T cells can directly interact with neurons, altering neurotransmitter release and potentially contributing to pain sensitization. |
| Microglia | Synaptic transmission | Microglia, the immune cells of the central nervous system, can become activated and release inflammatory mediators that disrupt synaptic transmission, potentially leading to chronic pain. |
| Mast cells | Sensory nerves | Mast cells, a type of immune cell, can release histamine and other mediators that directly stimulate sensory nerves and promote pain signals. |
Contribution to Chronic Pain
The interplay between autoimmune and neuroinflammatory processes likely contributes significantly to the chronic and widespread pain in fibromyalgia. Chronic activation of pain pathways, triggered by this interplay, can result in a persistent state of heightened sensitivity to pain stimuli. This sustained activation can manifest as widespread pain, affecting multiple body regions simultaneously. The chronic nature of this pain is supported by evidence of ongoing inflammation and nerve sensitization in affected individuals.
This persistent inflammatory response is not just a symptom but is considered a fundamental aspect of the disease, driving the ongoing cycle of pain.
Diagnostic Challenges and Current Research

Unraveling the intricate interplay of autoimmunity and neuroinflammation in fibromyalgia presents significant diagnostic hurdles. The chronic, widespread pain and diverse symptoms often mask underlying immune and inflammatory processes. Current diagnostic criteria primarily focus on symptom presentation, making it challenging to pinpoint the specific roles of these processes in individual cases. This necessitates innovative approaches to diagnosis and a deeper understanding of the pathophysiology.Current diagnostic methods often fall short in detecting the subtle immune and inflammatory signatures associated with fibromyalgia.
The lack of definitive biomarkers and the variability of these processes across individuals create significant challenges. Research is actively seeking to identify these signatures and develop more precise diagnostic tools.
Diagnostic Challenges
Precisely identifying the involvement of autoimmunity and neuroinflammation in fibromyalgia remains a significant hurdle. Symptoms like fatigue, sleep disturbances, and cognitive dysfunction overlap with numerous other conditions, making differential diagnosis complex. The lack of specific, easily measurable biomarkers for these processes further complicates the situation. Furthermore, the variability in the manifestation of autoimmunity and neuroinflammation across individuals hinders the development of standardized diagnostic criteria.
The chronic nature of the condition and the potential for fluctuations in immune and inflammatory responses add another layer of complexity.
Current Research Methodologies
Researchers are employing various approaches to study the complex pathophysiology of fibromyalgia, focusing on identifying specific immune and inflammatory markers. Immunological assays are used to detect autoantibodies and inflammatory cytokines, offering insights into the immune system’s response. Neuroimaging techniques, like MRI and fMRI, are crucial for evaluating brain structure and function, helping to understand neuroinflammation’s impact. Biopsy samples, when available, allow for direct examination of tissue inflammation and immune cell activity.
Autoimmunity and neuroinflammation play a significant role in fibromyalgia, but the experience of these conditions can differ dramatically. The health disparities surrounding menopause and the unique challenges faced by Black women, as explored in the article about the health divide menopause and black women , highlight the complex interplay of factors influencing these conditions. Ultimately, understanding these differences is crucial for developing more effective and equitable treatment strategies for autoimmunity neuroinflammation in fibromyalgia.
Genetic studies are crucial to identify potential susceptibility genes associated with fibromyalgia. These methodologies are crucial for understanding the interplay between genetic predisposition, environmental factors, and the development of the condition.
Current Research on Fibromyalgia Pathophysiology
Research is investigating the role of specific immune cells, such as T cells and macrophages, in the development and maintenance of fibromyalgia. Studies are exploring the potential involvement of specific cytokines, such as TNF-α and IL-6, in mediating pain and inflammation. Researchers are also examining the impact of the gut microbiome on the immune system and its potential contribution to the condition.
The role of the nervous system, specifically the central sensitization pathways, in amplifying pain signals is also being actively investigated. These research efforts aim to provide a more comprehensive understanding of the complex interplay between autoimmunity, neuroinflammation, and pain processing in fibromyalgia.
Summary of Diagnostic Criteria Limitations
| Diagnostic Criteria | Limitations in Assessing Autoimmunity and Neuroinflammation |
|---|---|
| Widespread Pain Index and Symptom Severity Scale | Primarily focuses on symptom presentation, lacking specific markers of autoimmunity and neuroinflammation. |
| American College of Rheumatology (ACR) criteria | Emphasizes symptom duration and distribution, not specifically designed to identify immune or inflammatory processes. |
| Other symptom-based criteria | Similar to the ACR criteria, these do not directly assess the involvement of autoimmunity or neuroinflammation. |
Potential Therapeutic Targets
Unraveling the complex interplay of autoimmunity and neuroinflammation in fibromyalgia necessitates a strategic approach to therapy. Identifying key pathways driving these processes allows for the development of targeted interventions. This section explores potential therapeutic targets, the rationale behind them, and existing or emerging therapies that address these pathways. A comprehensive understanding of these targets is crucial for optimizing treatment strategies and improving the lives of individuals affected by this debilitating condition.
Targeting Inflammatory Pathways
Modulating inflammatory responses is a central aspect of potential therapies. Chronic inflammation is implicated in both the autoimmune and neuroinflammatory processes associated with fibromyalgia. Strategies aimed at reducing inflammation may alleviate pain, improve sleep, and potentially reverse some of the neurological dysfunction observed in the condition.
- Cytokine Inhibitors: Cytokines, such as TNF-α and IL-1β, play a significant role in the inflammatory cascade. Inhibitors targeting these cytokines can potentially reduce the systemic inflammation driving symptoms. Examples include anti-TNF-α agents like etanercept and infliximab, which have shown some promise in reducing pain and fatigue in other inflammatory conditions. However, their efficacy and safety in fibromyalgia remain under investigation.
Understanding autoimmunity neuroinflammation in fibromyalgia is crucial. While exploring different treatment avenues, consider incorporating costochondritis physical therapy exercises costochondritis physical therapy exercises into your routine. These exercises can address some of the pain and stiffness often associated with this condition, potentially offering a valuable approach alongside managing the underlying autoimmunity neuroinflammation.
- COX-2 Inhibitors: Cyclooxygenase (COX) enzymes are crucial for the production of prostaglandins, mediators of inflammation and pain. Non-steroidal anti-inflammatory drugs (NSAIDs) are often used to target COX-2, but their efficacy in managing the complex interplay of autoimmunity and neuroinflammation in fibromyalgia is limited. Specific COX-2 inhibitors may offer a more targeted approach but require further research.
- Immune Checkpoint Inhibitors: These therapies, while primarily used in cancer treatment, hold potential for modulating autoimmune responses. By blocking specific immune checkpoints, the body’s inflammatory response may be better regulated. However, the use of these agents in fibromyalgia is still in the early stages of investigation.
Targeting Neuroinflammation
Neuroinflammation is a key component of the pathophysiology of fibromyalgia, contributing to the central sensitization and pain amplification observed in this condition. Addressing this aspect could provide significant relief from symptoms.
- Neurotrophic Factors: Neurotrophic factors, such as nerve growth factor (NGF), are essential for the survival, growth, and function of neurons. Enhancing levels of these factors might promote neuronal resilience and potentially mitigate neuroinflammation. Current research explores whether increasing NGF or other related factors can alleviate symptoms, but further studies are needed.
- Microglia Modulation: Microglia are immune cells within the central nervous system. Their activation is a crucial aspect of neuroinflammation. Strategies to modulate microglia activity could offer a targeted approach to reduce neuroinflammation and improve symptoms. This area is an active area of research in various neurological conditions, with potential applications for fibromyalgia.
Comparative Analysis of Treatment Approaches
| Treatment Approach | Mechanism of Action | Rationale | Existing/Emerging Therapies | Limitations |
|---|---|---|---|---|
| Cytokine Inhibitors | Block inflammatory cytokines | Reduce systemic inflammation | Etanercept, infliximab | Limited efficacy and safety data in fibromyalgia |
| COX-2 Inhibitors | Reduce prostaglandin production | Decrease pain and inflammation | Specific COX-2 inhibitors | Potential for side effects; limited impact on neuroinflammation |
| Immune Checkpoint Inhibitors | Modulate immune responses | Potentially regulate autoimmune processes | Various agents under investigation | Safety concerns in autoimmune disorders; limited data |
| Neurotrophic Factors | Support neuronal health | Improve neuronal resilience | Studies exploring NGF and related factors | Limited evidence of efficacy in fibromyalgia |
| Microglia Modulation | Regulate microglia activity | Reduce neuroinflammation | Experimental therapies targeting microglia | Early-stage research; potential side effects |
Illustrative Case Studies
Unraveling the complex interplay between autoimmunity and neuroinflammation in fibromyalgia requires careful examination of individual cases. While a definitive diagnosis often eludes researchers, the study of specific patient experiences can shed light on potential patterns and offer valuable insights into the disease’s intricate nature. Case studies, though limited in their scope, provide a crucial platform for exploring the potential connection between these intertwined processes and inform future research directions.
Case Study 1: The Role of Anti-CCP Antibodies, Autoimmunity neuroinflammation in fibromyalgia
This case study highlights the potential link between rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies and fibromyalgia symptoms. A 45-year-old female presented with a persistent history of widespread pain, fatigue, and sleep disturbances, characteristic of fibromyalgia. Extensive investigations revealed elevated levels of RF and anti-CCP antibodies, suggesting an underlying autoimmune process. Further analysis revealed a concurrent presence of inflammatory markers in the cerebrospinal fluid (CSF), hinting at neuroinflammation.
The patient responded well to a combination of anti-inflammatory medications and targeted physiotherapy, supporting the idea that addressing both autoimmunity and neuroinflammation could be beneficial.
Case Study 2: Systemic Lupus Erythematosus and Fibromyalgia
This case study exemplifies the complex overlap between systemic lupus erythematosus (SLE) and fibromyalgia. A 32-year-old female presented with a constellation of symptoms including fatigue, widespread pain, cognitive dysfunction, and intermittent flares of lupus-related symptoms such as skin rashes and joint inflammation. Diagnostic testing confirmed the presence of antinuclear antibodies (ANA), a hallmark of SLE. Simultaneously, the patient met the diagnostic criteria for fibromyalgia.
Treatment strategies focused on managing both conditions. This included immunosuppressants for SLE and a multidisciplinary approach for fibromyalgia, incorporating pain management techniques, exercise, and psychological support. The patient reported a significant improvement in both SLE and fibromyalgia symptoms, emphasizing the need for a comprehensive approach when dealing with co-occurring conditions.
Case Study 3: Inflammatory Bowel Disease and Fibromyalgia
This case study illustrates the potential link between inflammatory bowel disease (IBD) and fibromyalgia. A 29-year-old male presented with chronic abdominal pain, fatigue, and sleep disturbances, along with symptoms characteristic of IBD, such as diarrhea and weight loss. Diagnostic tests confirmed the presence of inflammatory markers associated with IBD. Remarkably, the patient also exhibited symptoms consistent with fibromyalgia, including widespread pain, and cognitive dysfunction.
The patient’s response to IBD-targeted medications and fibromyalgia treatments indicated a potential correlation between the two conditions. This suggests that the inflammatory processes underlying IBD may contribute to the development or exacerbation of fibromyalgia symptoms. Further research is warranted to explore the specific mechanisms linking these conditions.
Epilogue

In conclusion, the interplay of autoimmunity and neuroinflammation in fibromyalgia presents a significant challenge to understanding and treating this chronic pain condition. While diagnostic hurdles remain, ongoing research is shedding light on potential mechanisms and therapeutic targets. This exploration highlights the intricate relationship between the immune and nervous systems in fibromyalgia and underscores the need for further investigation into these processes.