How long does it take for HIV to progress to AIDS? This complex question delves into the intricacies of HIV infection, from initial exposure to the development of AIDS. Understanding the stages, factors influencing progression, and the crucial role of treatment is key to comprehending this disease. This exploration will cover the science behind HIV, the impact of various factors, and the importance of early detection and monitoring.
The progression of HIV to AIDS isn’t a simple timeline; it’s influenced by numerous elements. This in-depth look will provide a clear overview of the various factors that affect this timeline, from individual immune responses to access to healthcare and treatment. We’ll examine how different strains of HIV, co-infections, and treatment access all play a part in the rate of progression.
Defining HIV and AIDS Progression
Human Immunodeficiency Virus (HIV) and Acquired Immunodeficiency Syndrome (AIDS) are closely related but distinct conditions. HIV is a virus that attacks the immune system, specifically targeting and destroying CD4+ T cells, a crucial component of the body’s defense against infection. AIDS represents the most advanced stage of HIV infection, characterized by a severely compromised immune system, making the body vulnerable to opportunistic infections.Understanding the progression of HIV infection is crucial for effective management and prevention.
The stages of infection, from initial exposure to the development of AIDS, involve a gradual decline in immune function, making the individual susceptible to various diseases. This progression is directly linked to the virus’s ability to replicate and the immune system’s struggle to combat it. The following sections will detail these stages and the mechanisms involved.
While the time it takes for HIV to progress to AIDS varies significantly, understanding the complexities of other health issues like hidradenitis suppurativa (HS) is equally crucial. Knowing how to diagnose HS, for instance, is key to effective treatment, and resources like how to diagnose hidradenitis suppurativa can provide valuable insights. Ultimately, focusing on proactive health management, whether for HIV or other conditions, is important.
This involves understanding potential timelines and seeking appropriate medical guidance.
HIV Infection Stages
HIV infection progresses through distinct stages, each marked by different symptoms and levels of immune system damage. The stages reflect the virus’s replication and the immune system’s response, ranging from the initial infection to the development of AIDS.
| Stage | Symptoms | CD4+ T Cell Count (cells/mm³) |
|---|---|---|
| Acute HIV Infection (Flu-like illness) | Fever, fatigue, sore throat, headache, muscle aches, swollen lymph nodes, rash. These symptoms often appear within a few weeks of infection, sometimes resembling the flu. | > 500 |
| Chronic HIV Infection (Latency Period) | Often asymptomatic, although some individuals may experience persistent fatigue, swollen lymph nodes, or mild infections. The virus continues to replicate, but at a slower rate, often undetected by the individual. | 200-500 |
| AIDS | Severe immune deficiency, marked by the development of opportunistic infections (e.g., pneumonia, tuberculosis, certain cancers), and wasting syndrome. The individual becomes highly susceptible to life-threatening illnesses. | <200 |
Role of the Immune System
The human immune system plays a critical role in combating HIV infection. CD4+ T cells are a key target of the virus, as they coordinate the immune response. As HIV replicates, it progressively depletes the number of CD4+ T cells, weakening the immune system’s ability to fight off infections. This decline in immune function is a hallmark of HIV progression.
Viral Mechanisms
HIV’s ability to replicate and evade the immune system is critical to its progression. The virus infects CD4+ T cells, using its genetic material to replicate within the host cell. This process often damages the infected cells, further contributing to the depletion of the immune system. HIV’s high mutation rate also allows it to escape the body’s immune response, making it challenging to develop a cure.
HIV replicates through a complex process involving reverse transcription, integration of viral genetic material into the host cell’s DNA, and the production of new viral particles. This replication cycle significantly weakens the immune system over time.
Factors Influencing Progression Time
Understanding the factors that influence the rate of HIV progression to AIDS is crucial for developing effective prevention and treatment strategies. Different individuals experience varying timelines, impacting the overall course of the disease. This complexity stems from a multitude of interacting variables, including the specific strain of HIV, co-infections, access to healthcare, and individual immune responses.HIV’s journey from infection to AIDS is not a uniform path.
The time it takes for the virus to weaken the immune system varies greatly, depending on these influencing factors. This understanding is paramount to tailoring interventions that address the specific needs of affected individuals.
Impact of HIV Strains
Different strains of HIV, categorized into subtypes, exhibit varying levels of virulence. Some subtypes are associated with a faster rate of immune system decline. This difference in progression speed is attributed to variations in the virus’s genetic makeup, impacting its ability to replicate and evade the immune response. For instance, some subtypes may have a higher viral load, which means a greater number of HIV particles circulating in the body, potentially accelerating the progression to AIDS.
Role of Co-infections
Co-infections, such as other sexually transmitted infections (STIs), significantly impact HIV progression. STIs, like syphilis or herpes, can exacerbate inflammation and weaken the immune system, creating a synergistic effect that accelerates the progression of HIV. This is because these infections often create an environment that allows the HIV virus to replicate more easily. For example, individuals with both HIV and syphilis have been observed to experience faster declines in CD4+ T-cell counts, a critical measure of immune function.
Influence of Access to Healthcare and Treatment
Access to timely and appropriate healthcare, including antiretroviral therapy (ART), is a critical factor in determining the progression of HIV. ART helps to suppress HIV replication, allowing the immune system to recover and function more effectively. Individuals with consistent access to ART often experience a slower progression rate and a longer period of health and well-being. Conversely, those without access to treatment face a significantly higher risk of developing AIDS.
The availability of treatment, therefore, acts as a critical protective factor.
Comparison of Progression Times in Different Scenarios
| Scenario | Typical Progression Time (without treatment) | Typical Progression Time (with treatment) | Notes |
|---|---|---|---|
| HIV subtype B | 8-10 years | Potentially decades | Generally considered less aggressive |
| HIV subtype C | 5-7 years | Potentially decades | More prevalent globally and often associated with a faster progression rate |
| HIV infection with syphilis | Reduced | Potentially reduced, but varies | Co-infection accelerates HIV progression |
| HIV infection with consistent ART access | N/A | Prolonged period of health | ART significantly slows the progression of HIV |
Note: Progression times are estimates and can vary significantly depending on individual factors. The table provides a general comparison and should not be used for personal medical guidance. Always consult a healthcare professional for personalized advice.
Early Detection and Monitoring

Knowing your HIV status and actively monitoring your health are crucial for managing the infection effectively. Early detection allows for prompt treatment, which significantly impacts the progression of the disease and overall health outcomes. This proactive approach empowers individuals to take control of their well-being and work closely with healthcare providers to maintain optimal health.
Methods of Diagnosing HIV Infection
Accurate diagnosis is the cornerstone of effective HIV management. Various methods are used to identify the presence of HIV antibodies or viral components in the body. Blood tests are the most common and reliable methods. These tests detect antibodies produced by the immune system in response to the HIV virus. Rapid tests are also available, providing results within minutes.
These rapid tests are particularly useful in resource-limited settings or for individuals who may have difficulty accessing traditional laboratory services.
Importance of Early Detection and Regular Monitoring
Early detection of HIV infection allows for immediate initiation of antiretroviral therapy (ART). This crucial step can dramatically slow the progression of HIV and prevent the development of AIDS. Regular monitoring, including frequent testing and evaluations, is essential to assess the effectiveness of treatment and adjust strategies as needed. Early intervention and consistent monitoring minimize the impact of HIV on the body and help maintain a healthy quality of life.
Knowing how long HIV takes to progress to AIDS is crucial, but it’s also important to understand other health conditions. For example, angina, a condition characterized by chest pain, has significant prevalence and affects many people. Checking out angina facts and statistics can provide more insights into the condition’s impact. Ultimately, understanding the timeline for HIV progression remains vital for effective management and care.
Tests Used to Track HIV Progression and Immune Function
Several tests are used to monitor the progression of HIV and the health of the immune system. These tests assess the levels of HIV in the blood (viral load) and the number of CD4 cells, which are crucial components of the immune system. Monitoring these markers helps healthcare professionals understand the impact of HIV on the immune system and the effectiveness of treatment.
These tests are vital for adjusting treatment strategies and providing personalized care.
Typical Timelines for Monitoring CD4 Cell Counts and Viral Loads
The frequency of monitoring CD4 cell counts and viral loads depends on several factors, including the individual’s health status, treatment response, and the presence of other health conditions. Generally, patients starting ART may have their CD4 cell counts and viral loads checked every 3-6 months. As the virus is suppressed, monitoring may become less frequent. However, regular check-ups remain vital for continued health management.
For example, a patient with a stable viral load and CD4 count may be monitored every 6 months, while a patient experiencing treatment complications may require more frequent check-ups.
HIV Monitoring Tests Table
| Test | Purpose | Frequency |
|---|---|---|
| CD4 Cell Count | Measures the number of CD4 T cells, a key component of the immune system | Every 3-6 months, depending on individual circumstances |
| Viral Load | Quantifies the amount of HIV in the blood | Every 3-6 months, depending on individual circumstances |
| Antibody Test | Detects the presence of HIV antibodies | Initial screening, as needed |
| Rapid HIV Test | Provides rapid results for initial testing or in resource-limited settings | As needed, or as part of initial screening |
| Complete Blood Count (CBC) | Evaluates overall blood health | As needed, based on clinical indicators |
| Other blood tests (e.g., liver function tests) | Assesses organ function | As needed, based on clinical indicators or to monitor treatment side effects |
Antiretroviral Therapy (ART) and Impact on Progression
Antiretroviral therapy (ART) has revolutionized the management of HIV. It’s no longer a death sentence, but a manageable chronic condition for many. This dramatic shift is primarily due to the profound impact ART has on the progression of HIV to AIDS. By significantly suppressing the virus, ART allows the immune system to recover and function more effectively.
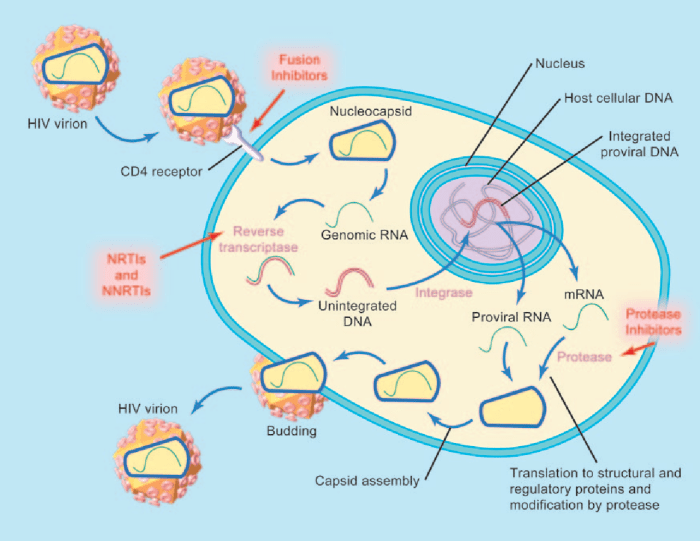
This, in turn, reduces the risk of opportunistic infections and other complications associated with AIDS.ART works by targeting different stages of the HIV life cycle, effectively hindering the virus’s ability to replicate. This interruption of the viral replication cycle leads to a reduction in the amount of HIV in the body, allowing the immune system to rebuild and fight off infections.
This is why consistent adherence to ART is so critical.
Function of ART in Slowing or Stopping HIV Progression
ART drugs work by interfering with various steps in the HIV replication process. They prevent the virus from entering cells, inhibiting the integration of viral genetic material into the host cell’s DNA, and blocking the production of new viral particles. By effectively blocking these crucial steps, ART significantly slows or even halts the progression of HIV, allowing the immune system to recover and function normally.
How ART Works to Inhibit Viral Replication
The HIV virus, in order to replicate, must first enter a human cell. ART drugs can block this entry. Once inside, the viral genetic material must be integrated into the host cell’s DNA. ART drugs also interfere with this integration process. Finally, the virus needs to produce new viral particles.
ART drugs also disrupt this process, preventing the assembly and release of new viruses. This multifaceted approach to viral suppression is a key factor in controlling HIV and preventing the progression to AIDS.
Understanding how long HIV takes to progress to AIDS is crucial, but equally important is knowing how to react to an allergic reaction, like anaphylaxis. Learning about first aid for allergies, specifically anaphylaxis, can be lifesaving. For instance, recognizing the signs and symptoms of a severe allergic reaction, and administering epinephrine (if prescribed), is a key aspect of first aid first aid allergies anaphylaxis.
Ultimately, knowing how to respond to these situations can actually make you better prepared to learn more about the progression of HIV. This knowledge is valuable, as it can help you make the best decisions about your health.
Different Types of ART Medications and Their Mechanisms of Action
Numerous ART medications exist, each targeting a specific step in the HIV life cycle. These medications are categorized into different classes, each with a unique mechanism of action.
- Nucleoside/Nucleotide Reverse Transcriptase Inhibitors (NRTIs): These drugs mimic the building blocks of DNA and RNA, which the virus needs to replicate. By incorporating these modified building blocks, they prevent the virus from creating a full copy of its genetic material. Examples include zidovudine (AZT) and lamivudine (3TC).
- Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs): These drugs bind to and directly inhibit the reverse transcriptase enzyme, the viral enzyme responsible for converting viral RNA into DNA. This prevents the conversion and thus hinders the replication process. Examples include efavirenz (Sustiva) and nevirapine (Viramune).
- Protease Inhibitors (PIs): These drugs target the protease enzyme, which is essential for the assembly of new viral particles. By inhibiting protease, the production of mature, infectious viruses is halted. Examples include ritonavir (Norvir) and lopinavir (Kaletra).
- Integrase Inhibitors (INSTIs): These drugs block the integrase enzyme, preventing the viral genetic material from integrating into the host cell’s DNA. This crucial step in the HIV replication cycle is blocked. Examples include raltegravir (Isentress) and dolutegravir (Tivicay).
- Entry Inhibitors: These drugs block the virus’s ability to enter the host cell. Examples include maraviroc (Selzentry) and enfuvirtide (Fuzeon).
Importance of Adherence to ART Regimens
Adherence to the prescribed ART regimen is absolutely critical for the success of treatment. Consistent and correct intake of medications is essential to maintain a low viral load and prevent the development of drug resistance. Missing doses or taking medications incorrectly can allow the virus to mutate and become resistant to the drugs, making it harder to control the infection in the future.
Comparison of Different ART Regimens on the Rate of HIV Progression
Different ART regimens vary in their effectiveness and potential side effects. The choice of regimen often depends on factors such as the individual’s overall health, the presence of other medical conditions, and potential drug interactions. Generally, regimens containing a combination of drugs from different classes are more effective at suppressing viral load and slowing or halting progression. Consistent use of these combined regimens significantly improves long-term health outcomes for people living with HIV.
ART Drugs, Classes, and Mechanisms of Action
| Drug | Class | Mechanism of Action |
|---|---|---|
| Zidovudine (AZT) | NRTI | Mimics DNA building blocks, preventing viral DNA synthesis |
| Efavirenz (Sustiva) | NNRTI | Inhibits reverse transcriptase enzyme |
| Ritonavir (Norvir) | PI | Inhibits protease enzyme, preventing viral particle assembly |
| Raltegravir (Isentress) | INSTI | Blocks integrase enzyme, preventing viral DNA integration |
| Maraviroc (Selzentry) | Entry Inhibitor | Blocks viral entry into the host cell |
Symptoms and Complications of AIDS

The progression of HIV to AIDS is marked by a weakening of the immune system, making individuals susceptible to a wide range of infections and complications. Understanding these symptoms and complications is crucial for early diagnosis and appropriate medical intervention. Early detection and prompt treatment significantly improve the quality of life and longevity for those affected.The later stages of HIV infection, characterized by AIDS, manifest with a variety of symptoms that can range from mild to severe.
The immune system’s compromised state allows opportunistic infections to flourish, leading to a decline in overall health and well-being. It is essential to recognize these symptoms and seek medical attention promptly.
Common Symptoms Indicating Progression to AIDS
Symptoms of AIDS progression can be varied and non-specific, sometimes mimicking other illnesses. These symptoms may include persistent fevers, unexplained weight loss, chronic fatigue, recurrent infections, and persistent skin rashes or sores. Individuals experiencing these symptoms should consult a healthcare professional for evaluation.
Opportunistic Infections in AIDS Patients, How long does it take for hiv to progress to aids
Opportunistic infections are a hallmark of AIDS. These infections take advantage of the weakened immune system, thriving where they would otherwise be controlled. Common examples include bacterial infections, fungal infections, and viral infections, which can lead to severe health consequences.
Complications Associated with Advanced HIV/AIDS
Advanced HIV/AIDS can lead to a range of complications affecting various organ systems. These complications can significantly impact an individual’s overall health, well-being, and quality of life. Examples include neurological complications, cardiovascular issues, and renal problems. Proper management of these complications through appropriate medical interventions is essential.
Impact of HIV/AIDS on Organ Systems
The progressive nature of HIV/AIDS can severely affect various organ systems. The compromised immune system allows opportunistic infections to attack different organs. The lungs, for instance, can be severely affected by pneumonia or other respiratory illnesses. The nervous system can be affected by neurological disorders. The gastrointestinal tract can be compromised by infections, and the cardiovascular system can be impacted by various conditions.
Common Opportunistic Infections in AIDS
This table lists some common opportunistic infections associated with AIDS, along with their symptoms. It is crucial to remember that this is not an exhaustive list, and symptoms can vary depending on the specific infection and individual. Early diagnosis and prompt treatment are essential for managing these infections.
| Opportunistic Infection | Common Symptoms |
|---|---|
| Pneumocystis pneumonia (PCP) | Shortness of breath, cough, fever, chest pain. |
| Tuberculosis (TB) | Cough, fever, night sweats, weight loss, fatigue. |
| Candidiasis (oral thrush) | White patches on the tongue or mouth, pain when swallowing. |
| Cytomegalovirus (CMV) retinitis | Blurred vision, floaters, eye pain. |
| Toxoplasmosis | Headache, seizures, confusion, fever, weakness. |
| Kaposi’s sarcoma | Purple or red lesions on the skin, mucous membranes, or other organs. |
Illustrative Case Studies (Hypothetical)
Understanding HIV progression is crucial for effective management. While every case is unique, examining hypothetical scenarios can illustrate typical patterns and the impact of interventions like antiretroviral therapy (ART). These examples highlight the importance of early diagnosis, consistent monitoring, and adherence to treatment.
Typical HIV Progression to AIDS (Case Study 1)
This hypothetical case study follows a 30-year-old man, identified only as “Patient A,” who contracted HIV through unprotected sexual contact. He was unaware of his infection for two years, during which the virus multiplied undetected. Early detection would have allowed for prompt initiation of ART and a more favorable outcome.Patient A’s initial CD4 cell count was 500 cells/mm³, considered within the healthy range.
Viral load was high, indicating significant viral replication. Without intervention, his CD4 count gradually declined over the next three years, as expected. Regular monitoring was crucial.
Monitoring CD4 Cell Counts and Viral Load
The following table shows the hypothetical progression of Patient A’s CD4 cell count and viral load over time.
| Time (Years) | CD4 Cell Count (cells/mm³) | Viral Load (copies/mL) |
|---|---|---|
| 0 | 500 | 100,000 |
| 1 | 450 | 80,000 |
| 2 | 400 | 60,000 |
| 3 | 350 | 40,000 |
| 4 | 300 | 20,000 |
| 5 | 250 | 10,000 |
| 6 | 200 | 5,000 |
Notice the gradual decline in CD4 count and the corresponding decrease in viral load. A significant drop below 200 cells/mm³ would indicate a progression towards AIDS.
Role of Antiretroviral Therapy (ART)
Patient A began ART at year 4 when his CD4 count reached 300 cells/mm³. This treatment aimed to suppress viral replication, allowing the immune system to recover. Adherence to ART is paramount for effectiveness. Treatment success is typically measured by the ability to maintain a suppressed viral load (below 50 copies/mL).
Impact of ART on Disease Progression
ART significantly impacted Patient A’s disease progression. Had he not started treatment, his CD4 count would have likely dropped to critically low levels much earlier. ART allowed his immune system to regain strength, improving his overall health.
Factors Influencing Progression Rate
Several factors can influence the rate of HIV progression. Patient A’s adherence to treatment, nutritional status, presence of other co-infections, and overall lifestyle choices all played a role in how quickly the virus progressed. The time between infection and the onset of symptoms is variable and can be influenced by these factors.
End of Discussion: How Long Does It Take For Hiv To Progress To Aids
In conclusion, understanding the timeline for HIV progression to AIDS is critical for individuals at risk and those already living with the virus. Early detection, consistent monitoring, and access to effective antiretroviral therapy (ART) are essential to manage the disease and prevent its progression to AIDS. The factors influencing progression, from immune response to co-infections, underscore the complexity of this disease and the need for individualized care.