Drugs that cause erectile dysfunction are a significant concern for many men. This issue is often overlooked, but understanding the various medications that can lead to erectile problems is crucial for maintaining overall health and well-being. This guide will explore the mechanisms by which certain drugs impact erectile function, examining specific drug categories, underlying mechanisms, and patient considerations.
We’ll also delve into case studies and treatment options to provide a comprehensive understanding of this often-hidden aspect of medication side effects.
Erectile dysfunction (ED) can stem from a variety of factors, including underlying health conditions and, surprisingly, certain medications. This comprehensive overview will equip readers with a clearer understanding of how various drug classes can interfere with the natural process of penile erection. By examining the mechanisms behind these effects, we can shed light on how these drugs impact blood flow, nerve signals, and hormonal balance, all of which play crucial roles in maintaining erectile function.
Introduction to Erectile Dysfunction-Causing Drugs
Erectile dysfunction (ED), the inability to achieve or maintain an erection firm enough for satisfactory sexual intercourse, is a common condition affecting men of various ages. While often associated with aging or underlying health conditions, certain medications can also contribute to ED as a side effect. Understanding the mechanisms behind this connection is crucial for both patients and healthcare professionals.
Proper diagnosis and management of ED require a comprehensive understanding of potential contributing factors, including drug-induced ED.Certain drugs interfere with the complex physiological processes involved in achieving an erection. These processes rely on a delicate balance of nerve signals, blood flow, and hormonal factors. Drugs that disrupt this balance can lead to ED. The severity and type of ED caused by a medication can vary considerably, depending on the individual and the specific drug.
It’s important to recognize that not everyone who takes a particular drug will experience ED, but the risk exists for some individuals.
Mechanisms of Drug-Induced Erectile Dysfunction
Many drugs can negatively impact erectile function through various mechanisms. These include interference with neurotransmitter signaling, hormonal imbalances, and vascular damage. For example, some medications can reduce nitric oxide levels, a crucial molecule for smooth muscle relaxation in the penis, thereby hindering blood flow. Other drugs might affect hormonal levels, which play a pivotal role in sexual function.
Comparison of Drug Classes and Potential ED
Understanding the potential links between specific drugs and ED can help individuals and healthcare providers make informed decisions. This table Artikels several drug classes known to potentially cause ED, alongside their mechanisms of action and common side effects.
| Drug Class | Mechanism of Action | Common Side Effects (Including Potential ED) | Examples of Drugs |
|---|---|---|---|
| Antihypertensives (e.g., Beta-blockers) | Reduce blood pressure by various mechanisms, including affecting heart rate and blood vessel tone. | Fatigue, dizziness, erectile dysfunction, low blood pressure, nausea. | Propranolol, Metoprolol, Atenolol |
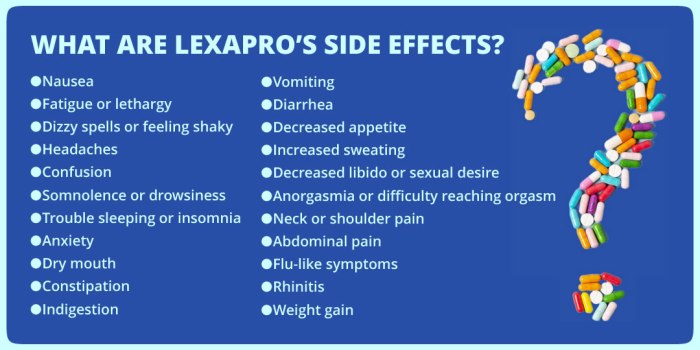
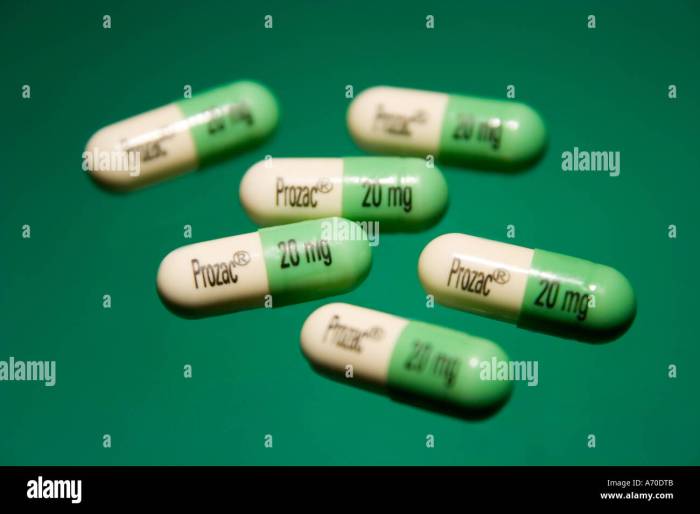
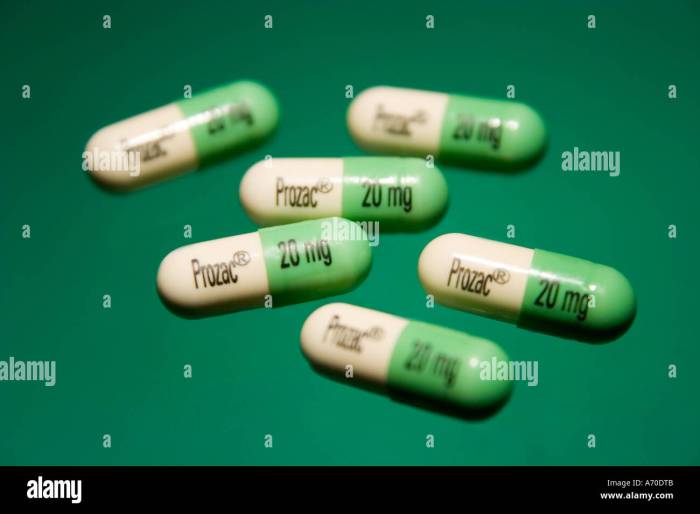
| Antidepressants (e.g., SSRIs) | Increase serotonin levels in the brain, often used to treat depression and anxiety. | Sexual dysfunction, including decreased libido and erectile dysfunction, nausea, weight changes. | Fluoxetine, Sertraline, Paroxetine |
| Antipsychotics | Affect dopamine and other neurotransmitters in the brain, commonly used to treat schizophrenia and other psychotic disorders. | Sexual dysfunction, including decreased libido, erectile dysfunction, weight gain, dry mouth. | Risperidone, Olanzapine, Haloperidol |
| Chemotherapy drugs | Interfere with cell division, often used to treat cancer. | Nausea, hair loss, fatigue, erectile dysfunction, loss of appetite. | Cisplatin, Doxorubicin, Cyclophosphamide |
| Hormonal Medications (e.g., Steroids) | Alter hormone levels, commonly used for various conditions. | Mood changes, fatigue, erectile dysfunction, increased appetite, changes in body composition. | Prednisone, Cortisone, Anabolic Steroids |
Specific Drug Categories and Their Effects
Understanding the potential side effects of medications is crucial for informed decision-making. This section delves into how various drug classes can impact erectile function, highlighting the importance of open communication with healthcare providers. Discussing these effects empowers patients to make well-informed choices about their treatment plans.
Cardiovascular Medications and Erectile Dysfunction
Cardiovascular medications, designed to manage conditions like high blood pressure and heart disease, often have side effects that can impact sexual function. These drugs can affect blood flow throughout the body, a crucial component of erectile function.
Medications used to treat cardiovascular conditions can sometimes lead to erectile dysfunction (ED). This occurs due to the impact on blood vessel relaxation and dilation, processes essential for achieving and maintaining an erection.
Antihypertensive Drugs and Erectile Dysfunction
Antihypertensive drugs, commonly prescribed to lower blood pressure, can sometimes contribute to erectile dysfunction. These medications can impact the smooth muscle relaxation required for proper blood flow to the penis.
- Certain types of beta-blockers, diuretics, and ACE inhibitors have been linked to ED in some patients.
- The mechanisms underlying this association involve the impact on the autonomic nervous system and blood vessel function.
- Individual responses to antihypertensive drugs vary, with some patients experiencing no significant side effects on their erectile function, while others may.
Antidepressants and Erectile Dysfunction
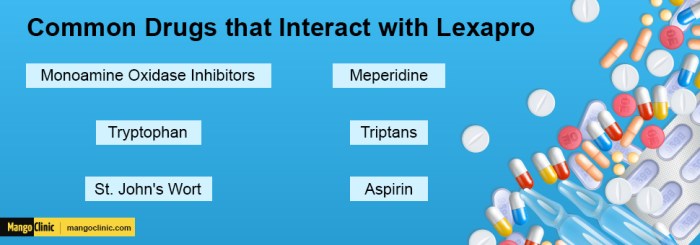
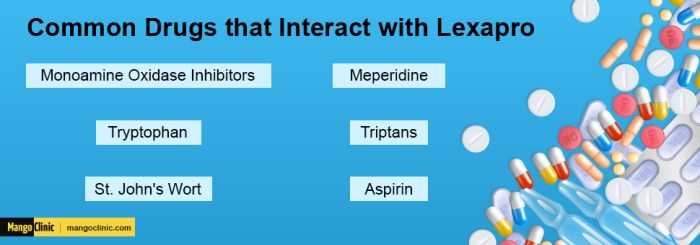
Antidepressants, crucial for managing mood disorders, can sometimes have a negative impact on sexual function, including erectile dysfunction. The exact mechanisms behind this are complex and vary based on the specific type of antidepressant.
- Selective serotonin reuptake inhibitors (SSRIs) are a common class of antidepressants that can cause sexual dysfunction, including ED, in some patients.
- Other classes of antidepressants, such as tricyclic antidepressants, may also affect erectile function, although the prevalence may vary.
- Patient reports and clinical studies have shown a correlation between antidepressant use and ED, highlighting the importance of open communication with healthcare providers regarding sexual side effects.
Antipsychotics and Erectile Dysfunction
Antipsychotic medications, used in the treatment of various mental health conditions, can sometimes affect erectile function. The impact on dopamine levels and the overall effect on the autonomic nervous system contribute to this side effect.
- Typical antipsychotics, often associated with a greater risk of sexual side effects including ED, are known to have a greater impact on dopamine levels than atypical antipsychotics.
- Atypical antipsychotics, while potentially less likely to cause ED, can still have a negative effect on sexual function in some patients.
- The degree of erectile dysfunction can vary depending on the individual and the specific antipsychotic used.
Hormonal Medications and Erectile Dysfunction, Drugs that cause erectile dysfunction
Hormonal medications, including those used to treat various conditions, can impact erectile function depending on the type and dosage. The impact on testosterone levels and other hormones is a critical factor.
- Corticosteroids, commonly used to reduce inflammation, can sometimes affect libido and erectile function.
- Androgen deprivation therapy (ADT), used in the treatment of prostate cancer, can significantly reduce testosterone levels, often leading to ED.
- The extent to which hormonal medications affect erectile function depends on the individual, the specific medication, and the dosage.
Comparison of Drug Classes and ED Risk
| Drug Class | Likelihood of ED | Underlying Mechanisms | Patient Considerations |
|---|---|---|---|
| Antihypertensives (e.g., beta-blockers, diuretics) | Moderate | Impact on blood vessel function, autonomic nervous system | Discuss potential ED with doctor; explore alternative medications if possible. |
| Antidepressants (e.g., SSRIs, SNRIs) | Moderate | Serotonin and norepinephrine imbalances | Openly discuss sexual side effects with doctor; explore alternative medications or treatment strategies. |
| Antipsychotics (e.g., typical, atypical) | High | Dopamine receptor blockade | Monitor for ED; explore alternative medications if possible. |
| Hormonal Medications (e.g., corticosteroids, ADT) | Variable | Impact on testosterone levels, hormonal balance | Discuss potential impact on sexual function with doctor; explore strategies to mitigate potential side effects. |
Mechanisms of Drug-Induced ED
Drugs can disrupt the intricate physiological processes involved in penile erection, leading to erectile dysfunction (ED). These disruptions often stem from the drug’s interference with the delicate balance of neurotransmitters, hormones, and blood flow. Understanding these mechanisms is crucial for both preventing and treating drug-induced ED.The complex interplay of neural signals, vascular responses, and hormonal influences all contribute to normal erectile function.
Disruptions to any of these areas can lead to ED, with different drugs affecting different aspects of this intricate process. For example, some drugs might impair the production of nitric oxide, a crucial molecule in the erection process, while others might interfere with the smooth muscle relaxation required for blood flow.
Nitric Oxide Production and Erection
Nitric oxide (NO) is a vital signaling molecule in the body, and it plays a pivotal role in penile erection. The production and release of NO trigger a cascade of events that lead to smooth muscle relaxation and vasodilation in the penile arteries and corpora cavernosa. This relaxation allows increased blood flow into the penis, causing an erection.
Certain drugs can directly inhibit the production of NO, or they may disrupt the signaling pathways that depend on NO. Examples of such drugs often include those used to treat high blood pressure.
Smooth Muscle Relaxation and Blood Flow
Penile erection relies on the relaxation of smooth muscle tissue within the corpora cavernosa, enabling increased blood flow. Drugs that impair this relaxation can severely impact erectile function. For instance, some medications that are used to treat hypertension may interfere with the relaxation response, resulting in reduced blood flow to the penis. This can lead to a significant decline in the ability to achieve and maintain an erection.
A direct effect on the smooth muscle is one of the ways these medications can affect the erectile response.
Neurotransmitter Pathways and Erection
The nervous system plays a crucial role in controlling the erection process. Neurotransmitters like dopamine, serotonin, and norepinephrine modulate the signals that trigger and sustain erections. Disruption of these neurotransmitter pathways can lead to ED. For instance, some antidepressants can alter serotonin levels, impacting the signals that initiate and maintain penile blood flow. Drugs affecting dopamine levels can also have similar effects.
Certain drugs are notorious for causing erectile dysfunction, impacting a man’s overall well-being. Interestingly, some health conditions can also affect this crucial function. For instance, exploring the connection between kidney stones and digestive issues is important; understanding if kidney stones can cause gastrointestinal problems is key to a holistic approach to health. can kidney stones cause gastrointestinal problems Knowing the potential ripple effects on the body is essential, and that includes potential impacts on sexual health.
Ultimately, understanding the interplay of various health factors is crucial in preventing or addressing erectile dysfunction.
Neurochemicals and Erectile Function
Neurochemicals such as dopamine and serotonin are integral components of the nervous system and play vital roles in controlling erectile function. For instance, dopamine is involved in initiating and maintaining the erection process. Conversely, serotonin can have an inhibitory effect. Certain medications that affect dopamine and serotonin levels can, therefore, disrupt the intricate balance required for normal erectile function.
Mechanisms of Drug-Induced ED: Detailed Table
| Drug | Specific Mechanism | Affected Pathways | Resulting Effect |
|---|---|---|---|
| Beta-blockers | Inhibit NO production and smooth muscle relaxation | Vascular, neural | Reduced blood flow, difficulty achieving and maintaining erection |
| Antidepressants (SSRIs) | Alter serotonin levels, impacting neurotransmission | Neural | Reduced libido, difficulty achieving and maintaining erection |
| Antihypertensives (some types) | Interfere with smooth muscle relaxation, reduce blood flow | Vascular | Reduced blood flow, impaired erection |
| Alcohol | Depresses CNS activity, impairs neurotransmission | Neural | Reduced libido, impaired erection |
Patient Considerations and Potential Solutions

Dealing with erectile dysfunction (ED) caused by medication can be frustrating and concerning. However, proactive communication and a collaborative approach with healthcare providers can significantly improve outcomes. Understanding the factors influencing ED, alongside potential solutions, empowers patients to take control of their health and well-being.Medication-induced ED is not an inevitable consequence. Often, adjustments can be made to manage the situation effectively.
This section explores patient considerations and potential solutions, emphasizing the importance of open communication, thorough evaluations, and personalized treatment plans.
Importance of Open Communication
Effective communication between patients and healthcare providers is paramount in addressing medication-induced ED. Patients should openly discuss any sexual health concerns with their doctors, including the medications they are taking. This includes both prescription and over-the-counter medications, as well as supplements and herbal remedies. Honesty and transparency facilitate a more accurate assessment of the situation and the development of appropriate solutions.
Certain medications, like some drugs used for treating chronic back pain, can unfortunately have side effects like erectile dysfunction. For example, steroid injections for steroid injections chronic back pain can sometimes impact sexual function. It’s important to discuss potential side effects with your doctor before starting any new medication, especially if you have concerns about erectile dysfunction.
Need for Thorough Medical Evaluations
A comprehensive medical evaluation is essential to identify the underlying cause of ED. This evaluation should encompass a review of the patient’s medical history, current health conditions, and the medications they are currently taking. Blood tests, physical examinations, and other diagnostic procedures may be necessary to rule out other potential contributing factors. This thorough evaluation allows for a tailored approach to treatment, maximizing the chances of success.
Certain medications can unfortunately lead to erectile dysfunction. It’s a common side effect of some drugs, and if you’re concerned, it’s crucial to talk to your doctor. For natural remedies, it’s important to research thoroughly, like learning more about goldenseal what should i know about it before trying anything new. While goldenseal might seem like a promising option, it’s essential to consult a healthcare professional before incorporating it into your routine, especially if you’re taking other medications, to avoid potential interactions and complications related to erectile dysfunction.
Potential Lifestyle Modifications
Several lifestyle modifications can mitigate the impact of medication-induced ED. These include maintaining a healthy weight, engaging in regular physical activity, and adopting a balanced diet. Stress management techniques, such as meditation or yoga, can also be beneficial. These lifestyle adjustments can improve overall health and potentially reduce the severity of ED symptoms.
Role of Alternative Treatments
Alternative treatments, such as acupuncture or herbal remedies, may offer potential benefits for some individuals. However, it is crucial to discuss these options with a healthcare provider before incorporating them into a treatment plan. Their effectiveness and safety in the context of medication-induced ED need to be carefully evaluated. Patients should not discontinue prescribed medications without consulting their doctor.
Influence of Patient History and Current Health Conditions
A patient’s medical history and current health conditions significantly influence the potential for medication-induced ED. Pre-existing conditions, such as cardiovascular disease or diabetes, can exacerbate the effects of certain medications. A thorough understanding of the patient’s complete medical profile is critical in tailoring an effective treatment plan.
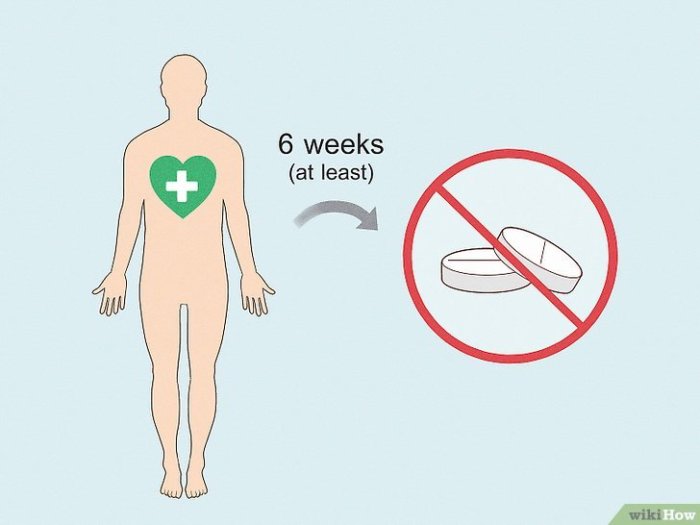
Adjusting Dosages or Switching Medications
When possible, adjusting dosages or switching medications is a viable option for mitigating medication-induced ED. A healthcare provider can evaluate the risks and benefits of different approaches, and work with the patient to find a solution that minimizes ED symptoms while maintaining the desired effects of the original medication.
Comparison of Treatment Options
| Treatment Type | Description | Potential Benefits | Potential Drawbacks |
|---|---|---|---|
| Lifestyle Modifications | Changes in diet, exercise, stress management | Improved overall health, potential reduction in ED symptoms | May not be sufficient for severe ED, requires commitment and time |
| Alternative Treatments (e.g., Acupuncture) | Non-conventional therapies | Potentially alleviate symptoms for some | Limited scientific evidence, potential interactions with medications |
| Medication Adjustments/Switching | Modifying dosage or prescribing a different medication | Target the cause of ED, potentially reduce symptoms | May not be feasible for all medications, potential side effects of new medication |
| Psychotherapy | Addressing psychological factors contributing to ED | Improve mental well-being, reduce stress related to ED | Requires patient commitment, may not be effective for all cases |
Case Studies and Illustrations: Drugs That Cause Erectile Dysfunction
Drug-induced erectile dysfunction (ED) is a significant issue, often overlooked or misdiagnosed. Understanding the specific cases where drugs contribute to ED is crucial for effective diagnosis and management. This section presents illustrative examples of how drug-induced ED manifests, highlighting the diagnostic approaches and successful treatment strategies employed.The examples presented below emphasize the importance of a thorough medical history, including medication use, when evaluating ED.
This approach allows healthcare providers to identify potential drug-related causes and implement appropriate management plans. Furthermore, the cases highlight the need for careful monitoring and follow-up care to ensure optimal patient outcomes.
Specific Case Examples of Drug-Induced ED
Several factors contribute to erectile dysfunction, and drug-induced ED is a significant concern. Medication side effects are often underestimated, but they can have substantial implications for a patient’s quality of life. This section provides examples of how drug-induced ED can affect patients and how it can be addressed.
Case Study 1: Beta-Blocker-Induced ED
A 55-year-old male patient presented with complaints of ED. His medical history revealed a diagnosis of hypertension and the use of a beta-blocker for blood pressure management. The patient reported decreased libido and difficulty achieving or maintaining erections. Diagnostic testing, including a physical examination and blood tests, ruled out other potential causes of ED. Based on the patient’s history and symptoms, the healthcare team suspected the beta-blocker as the culprit.
The patient was switched to an alternative blood pressure medication, and within a few weeks, his erectile function significantly improved.
Case Study 2: Antidepressant-Induced ED
A 32-year-old female patient reported ED symptoms after initiating a selective serotonin reuptake inhibitor (SSRI) antidepressant. She experienced decreased libido and difficulty achieving orgasm. The healthcare team carefully reviewed the patient’s medication regimen and considered the potential for drug-induced ED. The patient was advised about the possibility of sexual side effects and explored alternative antidepressant options. After switching to a different medication, the patient’s sexual function returned to normal.
Case Study 3: Chemotherapy-Induced ED
A 60-year-old male patient undergoing chemotherapy for cancer reported severe ED. The patient’s history revealed the use of certain chemotherapeutic agents known to cause ED as a side effect. The healthcare team discussed the potential impact of chemotherapy on sexual function with the patient and explored strategies to manage the side effect. Regular monitoring and support were provided, along with lifestyle recommendations to mitigate the symptoms.
Table Summarizing Key Findings from Case Studies of Drug-Induced ED
| Patient Demographics | Medication | Symptoms | Treatment Outcomes |
|---|---|---|---|
| 55-year-old male, hypertension | Beta-blocker | Decreased libido, difficulty achieving/maintaining erections | Switched to alternative blood pressure medication; erectile function improved |
| 32-year-old female, depression | SSRI antidepressant | Decreased libido, difficulty achieving orgasm | Switched to a different antidepressant; sexual function returned to normal |
| 60-year-old male, cancer | Chemotherapy agents | Severe ED | Regular monitoring, lifestyle recommendations, and support; symptoms managed |
Illustrative Images and Diagrams

Understanding the intricate mechanisms behind erectile dysfunction (ED) caused by drugs requires a visual representation of the penile anatomy and the physiological processes involved. This section provides detailed diagrams and explanations, focusing on the crucial role of blood flow and the impact various drugs have on the penile tissues.
Penile Anatomy and Blood Supply
The penis is a complex structure composed of two cylindrical bodies, called corpora cavernosa, and a spongy tissue called the corpus spongiosum. These tissues are filled with numerous small blood vessels, including arteries that carry blood in and veins that carry blood out. The intricate network of these vessels is crucial for the process of erection. A healthy flow of blood into the corpora cavernosa is essential for maintaining an erection.
The Erection Process: A Blood Flow Phenomenon
Penile erection is a highly orchestrated process involving the dilation of arteries and the constriction of veins within the penis. Stimulation triggers the release of nitric oxide (NO), a crucial chemical messenger. NO causes smooth muscle relaxation in the penile tissues, particularly within the corpora cavernosa. This relaxation allows the tissues to fill with blood, leading to an erection.
The subsequent constriction of the veins prevents blood from leaving the penis, maintaining the erection.
Impact of Drugs on Penile Tissues
Various drugs can disrupt this delicate balance of blood flow and smooth muscle relaxation. Some drugs directly interfere with the production or action of nitric oxide, hindering the relaxation process. Others may affect the smooth muscle cells themselves, altering their response to NO or other stimuli. Certain medications can also impact the overall blood vessel tone and function, which plays a vital role in maintaining an erection.
Nitric Oxide Pathway and Smooth Muscle Relaxation
Imagine a cascade of events triggered by the release of nitric oxide (NO). The diagram would show NO production, primarily in endothelial cells lining the blood vessels. NO diffuses to smooth muscle cells within the corpora cavernosa, activating a specific enzyme called guanylate cyclase. This enzyme catalyzes the conversion of GTP to cGMP. Elevated levels of cGMP lead to smooth muscle relaxation, allowing blood to flow into the corpora cavernosa.
This relaxation and subsequent blood flow are crucial for penile erection. A drug interfering with this pathway would disrupt the entire process.
Corpora Cavernosa: Structure and Response to Drugs
The corpora cavernosa are the two erectile tissues within the penis. Their structure consists of a network of trabeculae, which are connective tissue partitions. These trabeculae contain smooth muscle cells, which, when relaxed, allow the corpora cavernosa to expand and fill with blood, creating an erection. Drugs that affect smooth muscle function, such as those used to treat hypertension or heart conditions, can potentially disrupt the delicate balance required for a healthy erection by affecting the smooth muscle’s response to nitric oxide.
Drugs like alpha-blockers, for instance, can directly impact the smooth muscle cells, contributing to ED.
Closing Notes
In conclusion, a variety of medications can unfortunately lead to erectile dysfunction. This comprehensive guide has highlighted the intricate relationship between drug use and erectile function, emphasizing the importance of open communication between patients and healthcare providers. By understanding the potential risks and taking proactive steps to address potential issues, individuals can work with their doctors to find effective solutions and maintain overall well-being.
We’ve explored the physiological pathways affected, examined specific drug categories, and emphasized the need for patient-centered care in managing drug-induced ED. Ultimately, this knowledge empowers informed decisions about medication choices and promotes a healthier approach to sexual health.