Antibiotics before dental work are a common practice, but understanding the reasons behind it and the potential alternatives is crucial. This guide delves into the rationale for using antibiotics before dental procedures, considering various factors and risks involved. We’ll examine the different types of dental work, the impact of patient history, and alternatives to routine antibiotic use, ultimately aiming for a comprehensive understanding.
From the potential benefits of pre-emptive antibiotics to the potential downsides, this overview examines the considerations surrounding antibiotic use before dental work. We will discuss the factors that influence the decision, including patient risk factors and the specific types of dental procedures.
Antibiotics Before Dental Procedures: A Closer Look
Pre-dental antibiotic prophylaxis, a common practice, involves administering antibiotics before certain dental procedures to prevent potential infections. This is often done for individuals at higher risk of developing infections following procedures. Understanding the rationale, types of procedures, and concerns surrounding this practice is crucial for informed decision-making.
Rationale for Pre-Dental Antibiotic Use
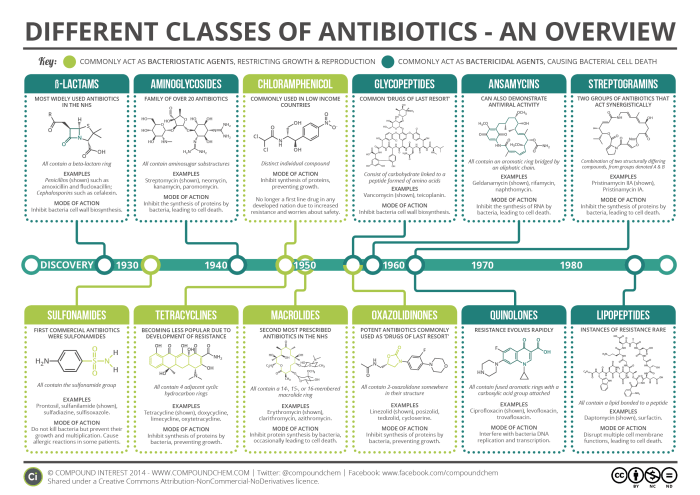
The rationale behind pre-dental antibiotic use stems from the potential for oral bacteria to enter the bloodstream during procedures. This can lead to infective endocarditis, a serious infection of the heart valves, especially in individuals with pre-existing heart conditions. The antibiotics act as a preventative measure, reducing the risk of bacterial invasion and subsequent infection.
Types of Dental Procedures Requiring Antibiotics
Certain dental procedures are more likely to introduce bacteria into the bloodstream, necessitating antibiotic prophylaxis. These procedures often involve invasive techniques or the manipulation of gum tissue.
Taking antibiotics before dental work can be a tricky decision, especially if you’re concerned about your overall health. Factors like your sleep quality can influence your body’s ability to heal. For example, if you’re struggling with poor sleep, checking out the Pittsburgh Sleep Quality Index (PSQI) might help you understand the potential impact on your immune system.
Ultimately, discussing your individual needs with a dentist is crucial to making the best choice regarding antibiotics before any dental procedure.
- Surgical extractions: Extractions of teeth requiring extensive tissue manipulation or bone removal.
- Periodontal procedures: Procedures involving deep scaling, root planing, or flap surgery, where bacteria are more likely to enter the bloodstream.
- Dental implant surgeries: These procedures can disrupt tissues and increase the risk of bacterial introduction.
- Tooth extractions: While not all extractions require antibiotics, those involving significant trauma or extensive manipulation of surrounding tissue often warrant pre-medication.
Concerns and Controversies Surrounding the Practice
While pre-dental antibiotic prophylaxis is often beneficial, there are concerns regarding its widespread use and potential drawbacks. These concerns include unnecessary antibiotic use, antibiotic resistance, and the potential for allergic reactions.
- Unnecessary antibiotic use: Some studies suggest that the benefits of pre-emptive antibiotics might be overstated for certain procedures or patient populations, leading to unnecessary antibiotic use and potential adverse effects.
- Antibiotic resistance: The overuse of antibiotics for routine procedures can contribute to the development of antibiotic resistance, making infections more difficult to treat in the future.
- Allergic reactions: Patients can experience allergic reactions to antibiotics, highlighting the importance of careful consideration and allergy testing before administering them.
- Potential for harm: While rare, antibiotics themselves can cause side effects such as gastrointestinal upset, skin rashes, and in extreme cases, more severe reactions.
Patient Selection and Risk Assessment
The decision to prescribe pre-dental antibiotics should be made on a case-by-case basis, considering the patient’s individual risk factors and the nature of the procedure. A thorough evaluation of the patient’s medical history, including pre-existing heart conditions and any known allergies, is crucial.
Factors influencing antibiotic use
Pre-dental antibiotic prophylaxis, while often necessary, isn’t a one-size-fits-all approach. Understanding the factors that influence the decision to prescribe antibiotics is crucial for both patients and dentists. This involves recognizing the risk factors that might necessitate their use, the selection process for the appropriate antibiotic, and the role of patient history in the decision-making process.The decision to prescribe pre-dental antibiotics hinges on a complex interplay of factors, including the patient’s individual risk profile and the specifics of the dental procedure.
This careful evaluation ensures that antibiotics are used judiciously, minimizing the risk of infection while also avoiding unnecessary exposure to these powerful medications.
Risk Factors Increasing the Need for Pre-dental Antibiotics
Certain factors increase a patient’s susceptibility to infection, potentially necessitating pre-dental antibiotics. These factors include a compromised immune system, previous history of endocarditis, and certain congenital heart conditions. A weakened immune system, such as that seen in patients with HIV or undergoing chemotherapy, makes them more vulnerable to infections.
- Compromised Immune System: Conditions like HIV, cancer treatment, and organ transplantations often lead to a weakened immune response, making patients more susceptible to infections following dental procedures. In such cases, the risk of bacterial endocarditis (infection of the heart valves) is elevated.
- History of Endocarditis: Patients with a prior history of bacterial endocarditis, an infection of the heart lining or valves, require careful consideration when undergoing dental procedures. Pre-dental antibiotics can significantly reduce the risk of recurrent endocarditis.
- Certain Congenital Heart Conditions: Some congenital heart conditions, especially those involving abnormal heart valves or repaired defects, place patients at higher risk for endocarditis during dental procedures. The specific condition and its severity influence the need for pre-dental antibiotics.
- Presence of Prosthetic Heart Valves: Patients with prosthetic heart valves are at substantial risk of endocarditis following dental procedures. Pre-dental antibiotics are typically recommended for these individuals.
Factors Determining the Choice of Antibiotic
Several factors influence the selection of the appropriate antibiotic. The type of dental procedure, the patient’s specific medical history, and potential allergies are critical considerations. The choice should be carefully weighed against the potential benefits and risks of each antibiotic.
- Type of Dental Procedure: The invasiveness of the dental procedure plays a role in the antibiotic selection. More invasive procedures, like those involving significant tissue manipulation, carry a higher risk of infection and may warrant a different antibiotic than less invasive ones.
- Patient Allergies: A thorough patient history regarding allergies to antibiotics is essential. Using an antibiotic to which the patient is allergic can lead to serious adverse reactions.
- Patient’s Medical History: The patient’s complete medical history, including any other current medications, is a critical factor. Drug interactions and other potential complications must be considered when selecting an antibiotic.
Role of Patient History in Decision-Making
A detailed patient history is paramount in determining the need for pre-dental antibiotics. This history includes not only current medical conditions but also past illnesses, surgeries, and allergies.
- Current Medical Conditions: Active infections, such as respiratory or urinary tract infections, might influence the need for pre-dental antibiotics. The severity and type of infection need careful consideration.
- Past Illnesses and Surgeries: Previous surgeries, particularly those involving the heart or vascular system, and any associated complications, play a role in the risk assessment.
- Allergies: Allergies to specific antibiotics are crucial information, as alternative medications must be considered.
Impact of Specific Medical Conditions on Antibiotic Use
Certain medical conditions significantly impact the decision regarding pre-dental antibiotics. The specifics of each condition and its severity must be considered.
- Rheumatic Heart Disease: Patients with rheumatic heart disease, particularly those with valve damage, require careful consideration when undergoing dental procedures.
- Cardiovascular Conditions: Various cardiovascular conditions, including previous heart attacks, heart failure, and coronary artery disease, influence the risk assessment for endocarditis and guide antibiotic decisions.
Different Age Groups and Their Effect on the Decision
Age-related factors influence the need for pre-dental antibiotics. Infants, children, and the elderly require specific considerations.
- Infants and Children: Infants and children may have underdeveloped immune systems, increasing the risk of infection following dental procedures. Appropriate antibiotics and dosages need careful evaluation.
- Elderly: The elderly may have co-morbidities that increase the risk of infection and adverse drug reactions. Pre-dental antibiotics are carefully considered, and the choice of antibiotic should be tailored to individual needs.
Types of Dental Procedures and Associated Risks: Antibiotics Before Dental Work
Understanding the specific risks of infection associated with different dental procedures is crucial for determining the appropriate antibiotic prophylaxis. Various dental treatments carry varying degrees of potential for introducing bacteria into the bloodstream, which can lead to serious systemic infections. This section delves into the types of dental procedures, their associated risks, and the rationale for antibiotic use in each case.
Dental Procedures and Infection Risk
Different dental procedures carry different levels of risk for introducing bacteria into the bloodstream. Procedures involving manipulation of the gums, bone, or teeth are more likely to cause bacterial spread than routine cleanings.
Taking antibiotics before dental work is a common practice, and for good reason. Just like prepping for a surgery, it’s about preventing infections. Similar to the meticulous care needed after something like fracture hardware removal, where physical therapy after fracture hardware removal plays a crucial role in recovery, antibiotics help reduce the risk of post-procedure complications.
So, next time you need dental work, remember to discuss the need for antibiotics with your dentist.
| Procedure Type | Risk of Infection | Rationale for antibiotic use |
|---|---|---|
| Dental extractions (removal of teeth) | High | Often warranted due to the disruption of tissues and potential for bone exposure. |
| Dental implants | Moderate | May require antibiotics depending on the complexity and surgical nature of the procedure. |
| Root canal therapy | Low to Moderate | Antibiotic use is often considered if there is extensive infection or risk factors are present. |
| Gum disease treatment (e.g., scaling and root planing) | Low | Usually not routinely required unless significant inflammation is present. |
| Routine dental cleanings (prophylaxis) | Very Low | Antibiotics are not typically needed. |
Potential for Bacterial Spread During Procedures
The potential for bacterial spread during dental procedures depends on factors such as the complexity of the procedure, the patient’s oral health, and the specific instruments used. For instance, procedures that involve extensive tissue manipulation, such as extractions or gum surgeries, are more likely to disrupt the oral flora and introduce bacteria into the bloodstream. In contrast, routine cleanings typically do not cause the same level of disturbance.
Proper sterilization techniques and meticulous surgical practices help mitigate this risk.
Post-Dental Work Infections
Certain infections can develop following dental procedures. These infections can range from mild to severe and require appropriate medical intervention.
| Infection Type | Symptoms | Treatment |
|---|---|---|
| Bacterial Endocarditis | Fever, chills, fatigue, heart murmur, shortness of breath | Hospitalization, intravenous antibiotics, possibly surgery. |
| Cellulitis | Redness, swelling, warmth, pain, tenderness in the affected area | Oral antibiotics, potentially hospitalization. |
| Abscesses | Pain, swelling, tenderness, pus formation | Drainage of the abscess, antibiotics, potentially hospitalization. |
| Sepsis | Severe inflammation throughout the body; fever, chills, rapid pulse, low blood pressure, altered mental status | Intensive care, intravenous antibiotics, supportive care. |
Bacterial endocarditis, a serious infection of the heart valves, is a potential complication that can arise from dental procedures. It is a concern primarily for individuals with pre-existing heart conditions.
Alternatives to Routine Antibiotic Use
Taking antibiotics before dental procedures is a common practice, but it’s not always necessary. Recent research and a growing understanding of oral health have highlighted alternative approaches to preventing infections, focusing on strategies that reduce risk without the potential downsides of antibiotics. This shift emphasizes proactive oral hygiene and preventative measures alongside traditional methods.Alternative strategies offer a balanced approach to dental care, minimizing the use of antibiotics while maintaining a high standard of infection control.
This proactive approach empowers individuals to take an active role in their oral health, leading to healthier outcomes and fewer instances of antibiotic-related side effects.
Oral Hygiene Practices and Infection Prevention
Maintaining excellent oral hygiene plays a crucial role in reducing the risk of infection before and after dental procedures. Regular brushing, flossing, and using mouthwash help remove plaque and bacteria, significantly reducing the number of pathogens that could lead to complications.
- Brushing Technique: Proper brushing technique, twice daily for two minutes, is essential for effectively removing food particles and plaque. A soft-bristled brush and gentle, circular motions are key to avoiding gum irritation and enamel damage.
- Flossing: Daily flossing removes plaque from between teeth where brushing alone cannot reach. This helps prevent the buildup of bacteria and tartar, which are major contributors to gum disease.
- Mouthwash: Antiseptic mouthwashes can help reduce bacteria in the mouth. These can complement brushing and flossing, enhancing oral hygiene and decreasing the likelihood of infection.
Preventive Measures Before and After Dental Procedures
Several preventive measures can be taken before and after dental procedures to further reduce the risk of infection. These strategies complement robust oral hygiene routines.
- Pre-procedure Rinse: Using a prescribed antiseptic mouth rinse before a procedure can help temporarily reduce bacterial load in the mouth. This is particularly useful for procedures that involve minor incisions or trauma.
- Post-procedure Care: Following the dentist’s instructions for aftercare is critical. This may include using prescribed mouth rinses, avoiding specific foods or activities, and maintaining meticulous oral hygiene to prevent infection.
- Lifestyle Factors: Maintaining a healthy lifestyle with a balanced diet, sufficient sleep, and stress management can boost the body’s natural defenses, potentially reducing susceptibility to infections.
Comparison of Risks and Benefits
The decision to use antibiotics or alternative strategies depends on a careful consideration of the risks and benefits. Antibiotics, while effective in many cases, can have side effects, including allergic reactions, antibiotic resistance, and disruptions to the gut microbiome. Alternative strategies, on the other hand, reduce these potential risks while promoting overall oral health.
| Factor | Antibiotics | Alternative Strategies |
|---|---|---|
| Effectiveness | Generally effective against bacterial infections | Effective in preventing infections by reducing bacterial load and promoting oral hygiene |
| Side Effects | Potential for allergic reactions, antibiotic resistance, and disruption of gut microbiome | Minimal side effects, primarily focusing on oral hygiene |
| Long-term Impact | Potential for long-term health consequences | Promotes long-term oral health and overall well-being |
| Cost | May involve costs associated with medication | Lower cost associated with lifestyle changes and oral hygiene |
“Proactive oral hygiene, including consistent brushing, flossing, and the use of mouthwash, is a powerful tool for infection prevention, significantly reducing the need for routine antibiotic use.”
Specific Considerations for Different Patient Groups
Antibiotic prophylaxis before dental procedures is a crucial aspect of patient care, but its application varies significantly based on individual factors. Understanding these nuances is essential for tailoring recommendations to specific patient groups, optimizing safety, and minimizing unnecessary antibiotic use. This section delves into the considerations for various patient populations, including those with underlying medical conditions, children, and individuals with antibiotic allergies.
Ever wondered about antibiotics before dental work? It’s a common practice, often recommended to prevent infection, especially if you have a history of certain conditions. Similar to how careful preparation is key for a smooth recovery after nasal polyps surgery, nasal polyps surgery recovery involves careful post-operative care. Ultimately, the right antibiotic strategy, like the right aftercare for any procedure, is crucial for preventing complications and getting back to your best self quickly.
This is why understanding the reasoning behind antibiotics before dental work is essential.
Patients with Underlying Medical Conditions
Patients with certain medical conditions may have an increased risk of complications from infections, thus requiring careful consideration of antibiotic use. For example, individuals with compromised immune systems, such as those undergoing chemotherapy or with conditions like HIV, are more susceptible to infections. Similarly, patients with heart conditions, particularly those with prosthetic heart valves or a history of infective endocarditis, are at a higher risk of developing bacterial endocarditis following dental procedures.
In such cases, the decision to prescribe antibiotics should be made in consultation with the patient’s cardiologist or other relevant specialists. A comprehensive assessment of the patient’s medical history and current condition is critical.
Children
The need for antibiotics before dental procedures in children differs from that in adults. Pediatric patients may exhibit varying degrees of risk tolerance and response to infections, and the potential for adverse effects from antibiotics needs careful consideration. Additionally, children’s developing immune systems might require a different approach to prophylaxis. The risk-benefit ratio of antibiotic use must be carefully evaluated based on the specific child’s medical history and the nature of the dental procedure.
Consideration should be given to potential side effects of antibiotics, such as allergic reactions or gastrointestinal distress, which can be more pronounced in children.
Antibiotic Allergies or Sensitivities
Patients with documented allergies or sensitivities to antibiotics require specific attention. A thorough allergy history is paramount. If an allergy is confirmed, alternative approaches to preventing infection must be explored. These might include meticulous oral hygiene instructions, careful post-operative care, or the use of alternative antimicrobial agents. The presence of a documented allergy necessitates a detailed discussion with the patient’s physician to determine the safest and most effective course of action.
Impact of Dental Procedure Type
The specific type of dental procedure also plays a role in the decision to use antibiotics. Procedures involving manipulation of tissues, especially those that involve the gums and other soft tissues, may carry a higher risk of infection than procedures that do not involve significant tissue manipulation.
Table of Patient Group Considerations
| Patient Group | Conditions | Antibiotic Recommendations |
|---|---|---|
| Patients with compromised immune systems (e.g., HIV, cancer treatment) | Weakened immune response, increased susceptibility to infection | Antibiotic prophylaxis is often recommended, with careful consideration of the specific condition and procedure. Consultation with the patient’s physician is crucial. |
| Patients with prosthetic heart valves or history of infective endocarditis | Increased risk of bacterial endocarditis | Antibiotic prophylaxis is typically recommended, following guidelines established by the American Heart Association (AHA). |
| Children | Developing immune systems, potential for adverse effects from antibiotics | Antibiotic prophylaxis should be considered carefully, based on the specific child’s medical history, the nature of the procedure, and the risk-benefit assessment. |
| Patients with antibiotic allergies or sensitivities | Allergic reactions to antibiotics | Alternative strategies, such as meticulous oral hygiene or alternative antimicrobial agents, should be explored. Consultation with the patient’s physician is essential. |
Patient Education and Informed Consent
Open communication and patient understanding are crucial when discussing pre-dental antibiotics. Educating patients about the rationale behind these medications empowers them to make informed decisions about their dental care. This process builds trust and ensures that the chosen course of action aligns with the patient’s values and well-being.
Patient Education Guide
Effective patient education requires a clear explanation of the benefits and potential risks of pre-dental antibiotics. This approach aims to avoid unnecessary anxiety while ensuring patients comprehend the decision-making process. A straightforward, empathetic approach is essential to promote active participation and shared decision-making.
Sample Dentist Script
This script provides a framework for dentists to explain pre-dental antibiotics to their patients. The key is to present information clearly and concisely, allowing patients to ask questions and express concerns.
“Good morning, [Patient Name]. Today, we’re discussing the use of antibiotics before your dental procedure. These medications are sometimes recommended to help prevent potential infections. The risk of infection is very low in most cases, but in certain individuals, such as those with weakened immune systems, pre-operative antibiotics may be beneficial. We will assess your specific situation to determine the best course of action.”
“We will discuss your medical history and any underlying conditions that might increase your risk of infection. This helps us make an informed decision together about whether antibiotics are necessary for your procedure.”
“If antibiotics are recommended, we will carefully explain the benefits and potential side effects. You have the right to ask questions and discuss your options.”
Informed Consent Flowchart, Antibiotics before dental work
The flowchart Artikels the process for obtaining informed consent. It emphasizes the importance of patient comprehension and active participation in the decision-making process.
(Note: A visual flowchart would illustrate this process more effectively. A flowchart could include steps like: Patient History Review, Risk Assessment, Discussion of Options, Questioning and Clarification, Consent Form Signing, and Documentation.)
Patient Education Pamphlet Elements
This pamphlet serves as a valuable resource for patients, providing clear and concise information about pre-dental antibiotics.
- Introduction: Briefly introduce the concept of pre-dental antibiotics and their role in preventing infection. Mention that the decision is individualized and based on the patient’s specific needs.
- Rationale for Use: Clearly explain the rationale behind pre-dental antibiotic use, focusing on the prevention of post-operative infections. Include examples of high-risk individuals.
- Potential Benefits: Explain the potential benefits of using pre-dental antibiotics, highlighting the prevention of infections and reducing the risk of complications. Explain the limited benefits in some cases.
- Potential Risks: Discuss the potential risks and side effects of antibiotics, including allergic reactions, antibiotic resistance, and other adverse effects. Emphasize that these risks are usually minimal.
- Patient’s Role: Clearly state the patient’s role in the decision-making process, highlighting their right to ask questions and seek clarification. Highlight the importance of honesty regarding medical history.
- Patient Questions: Include a section where patients can list their questions or concerns regarding the use of pre-dental antibiotics.
- Contact Information: Provide contact information for the dental office, including the dentist and staff, allowing patients to follow up with any questions or concerns.
Emerging Research and Trends

Reducing the routine use of antibiotics before dental procedures is a growing area of research. Early studies have shown promising results, leading to a shift in clinical guidelines and a renewed focus on minimizing unnecessary antibiotic exposure. This shift reflects a broader global effort to combat antibiotic resistance, a significant threat to public health.Current research is actively investigating alternative strategies to minimize the need for prophylactic antibiotics in dental settings.
These approaches range from better risk assessment tools to novel preventive measures, aiming to personalize treatment plans and reduce the overuse of antibiotics.
Investigating Alternatives to Routine Antibiotic Use
Research into alternative strategies for preventing infection after dental procedures is increasingly focusing on individual patient factors. This includes exploring pre-emptive measures, such as improved oral hygiene protocols and tailored risk stratification models. The aim is to identify patients who truly benefit from antibiotics, reducing unnecessary exposure for those who don’t.
Examples of New Studies
Numerous studies are exploring alternative approaches to routine antibiotic use. One notable area of research involves evaluating the effectiveness of pre-emptive oral hygiene regimens in high-risk patients. Studies are also looking at the use of local anesthetics and antimicrobial mouthwashes to reduce the risk of post-operative infections. Furthermore, research is underway to refine risk assessment models, using factors like age, medical history, and specific dental procedures to determine antibiotic necessity.
Impact on Clinical Practice
The findings from these studies are impacting clinical practice in several ways. Dental professionals are increasingly using risk assessment tools to tailor antibiotic prescriptions. For example, a patient with a history of recurrent infections might require antibiotics, while a healthy individual undergoing a routine cleaning might not. This personalized approach to antibiotic use is becoming more commonplace, reducing unnecessary antibiotic exposure and potentially contributing to a decline in antibiotic-resistant bacteria.
Long-Term Implications of Reducing Antibiotic Use
The long-term implications of reducing routine antibiotic use are substantial. A key benefit is the potential to slow the development and spread of antibiotic-resistant bacteria. This is crucial for maintaining the effectiveness of antibiotics for treating serious infections in the future. Furthermore, reducing unnecessary antibiotic use can potentially decrease the risk of adverse reactions to antibiotics in patients.
While the exact long-term impact remains an area of ongoing research, early indicators suggest a positive correlation between reduced antibiotic use and a healthier microbial ecosystem.
Outcome Summary
In conclusion, the decision to use antibiotics before dental work is complex, demanding careful consideration of individual patient needs and risk factors. While antibiotics can offer protection against infection, the potential for harm, especially with overuse, underscores the importance of exploring alternative preventative strategies. Understanding the risks and benefits of both approaches is vital for informed decision-making, leading to better patient outcomes.