The benefits of carnosine, a naturally occurring compound, are increasingly recognized for its potential impact on muscle function, cellular health, and even neurological well-being. This exploration delves into the science behind carnosine, examining its various roles and potential applications. We’ll uncover how carnosine impacts everything from athletic performance to the aging process.
Carnosine, a dipeptide found naturally in the body, is a crucial component in numerous physiological processes. It’s found in high concentrations in muscle tissue, where it plays a role in protecting against damage and fatigue. This article explores how carnosine may contribute to muscle strength, reduce fatigue, and potentially even influence the aging process. We’ll also discuss various sources of carnosine, from dietary intake to supplements, and delve into the safety considerations surrounding its use.
Introduction to Carnosine
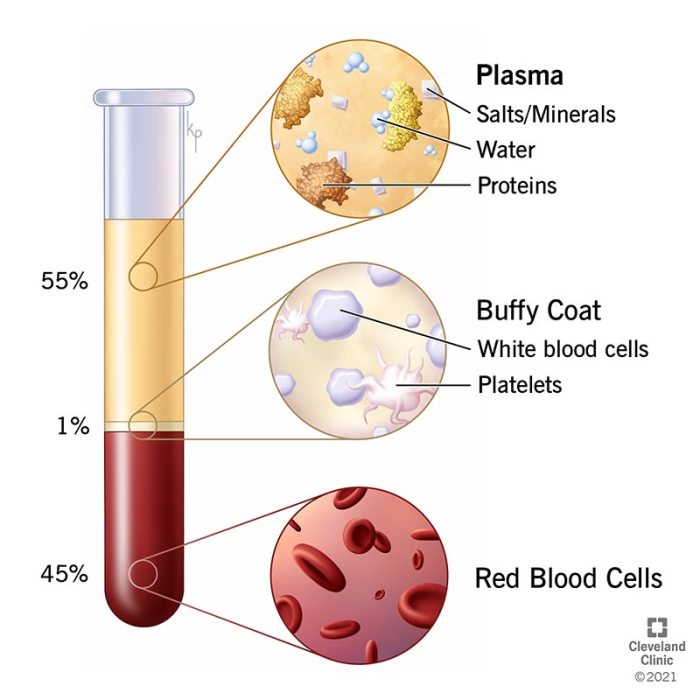
Carnosine, a naturally occurring dipeptide, plays a crucial role in various physiological processes within the human body. It’s a combination of two amino acids, beta-alanine and histidine, linked together. Its chemical structure, β-alanyl-L-histidine, contributes to its unique properties and biological activities.This compound is found in high concentrations in skeletal muscle and the brain, indicating its importance for these organs.
Understanding its natural sources, physiological roles, and available forms can help us appreciate its potential benefits and appropriate usage.
Natural Sources of Carnosine
Carnosine is primarily synthesized within the body, but it’s also found in certain foods. The highest concentrations are found in skeletal muscle tissue. Brain tissue also contains significant amounts. The diet, though, plays a minor role in carnosine intake compared to endogenous production. Certain animal products, such as beef and pork, contain noticeable amounts of carnosine.
The presence of carnosine in foods varies significantly depending on factors like animal breed, diet, and preparation methods.
Role of Carnosine in Physiological Processes
Carnosine’s primary function is to act as a buffer, neutralizing harmful compounds and protecting against oxidative stress. It also plays a crucial role in maintaining cellular homeostasis, reducing inflammation, and supporting various metabolic processes. This dipeptide acts as a powerful antioxidant, combating free radicals and mitigating the damaging effects of oxidative stress. It contributes to maintaining the optimal pH balance in cells and tissues, crucial for healthy function.
Forms and Types of Carnosine
Understanding the various forms of carnosine is important for choosing the appropriate supplementation strategy. Different forms may have varying bioavailability and absorption rates, impacting their effectiveness.
| Form | Source | Benefits (Potential) | Dosage |
|---|---|---|---|
| Powder | Dietary Supplements | Muscle support, potential antioxidant benefits | Typically 1-3 grams per day, depending on individual needs and product recommendation. |
| Capsules | Dietary Supplements | Convenient delivery, potentially higher bioavailability compared to powders | Dosage varies with the supplement; consult the product label for specific recommendations. |
| Food Sources | Beef, Pork, Poultry | Natural source of carnosine, potentially beneficial in conjunction with a balanced diet. | Intake varies depending on the amount of food consumed. |
Potential Benefits of Carnosine
Carnosine, a naturally occurring dipeptide found in high concentrations in muscle tissue, has garnered significant interest for its potential health benefits, particularly in the realm of athletic performance and muscle function. This exploration delves into the potential benefits of carnosine, examining its impact on muscle function, fatigue, recovery, and oxidative stress.Understanding the intricacies of carnosine’s action is crucial to appreciating its potential.
Carnosine’s ability to buffer reactive compounds, like hydrogen peroxide, and its role in maintaining cellular homeostasis are pivotal to its purported benefits.
Muscle Function and Protein Synthesis
Carnosine’s presence in muscle tissue is strongly correlated with muscle function. Research suggests carnosine might positively influence muscle protein synthesis, a key process in building and repairing muscle tissue. This enhancement could lead to improved muscle strength and endurance. Increased muscle protein synthesis is vital for muscle growth and repair, contributing to a stronger and more resilient muscular system.
Effects on Muscle Fatigue and Recovery
Muscle fatigue is a significant concern for athletes and individuals engaging in strenuous physical activity. Carnosine is hypothesized to play a crucial role in mitigating this fatigue by neutralizing the accumulation of lactic acid and other metabolites that contribute to muscle fatigue. This neutralization can facilitate faster recovery and reduced post-exercise soreness.
Protection Against Oxidative Stress
Oxidative stress, caused by the accumulation of harmful reactive oxygen species (ROS), can damage muscle tissue and impair performance. Carnosine acts as a potent antioxidant, protecting against oxidative stress and cellular damage. Its ability to quench ROS is a key factor in preserving muscle health and function, particularly during intense exercise.
Carnosine, a naturally occurring compound, boasts impressive antioxidant properties, potentially offering protection against cellular damage. Understanding how it impacts the body’s response to infections like gonorrhea is fascinating, especially after treatment. For example, knowing the potential symptoms that can arise post-treatment, like those detailed in this article on gonorrhea symptoms after treatment , is crucial for holistic health.
Ultimately, carnosine’s benefits extend to supporting overall cellular health and resilience, making it a potentially valuable supplement in a comprehensive health strategy.
Comparative Analysis of Carnosine’s Effects on Different Muscle Types
| Muscle Type | Effect on Function | Effect on Fatigue | Effect on Oxidative Stress |
|---|---|---|---|
| Skeletal Muscle | Potentially enhanced strength and endurance due to improved protein synthesis and reduced damage. | Reduced fatigue by buffering metabolites like lactic acid. | Reduced oxidative stress and cellular damage, maintaining muscle integrity. |
| Cardiac Muscle | Potentially improved contractility and reduced risk of damage from oxidative stress, particularly in conditions like heart failure. | Possible reduction in fatigue, potentially improving cardiac function. | Protection against oxidative stress, mitigating damage associated with reactive oxygen species. |
Potential for Enhancing Athletic Performance
The potential benefits of carnosine for athletic performance are promising. By improving muscle function, reducing fatigue, and protecting against oxidative stress, carnosine could contribute to enhanced endurance, strength, and recovery. This translates to improved athletic output, faster recovery times, and a potentially greater capacity for sustained physical exertion. For example, increased carnosine levels in athletes might translate to more repetitions in a weightlifting routine or a longer run without fatigue.
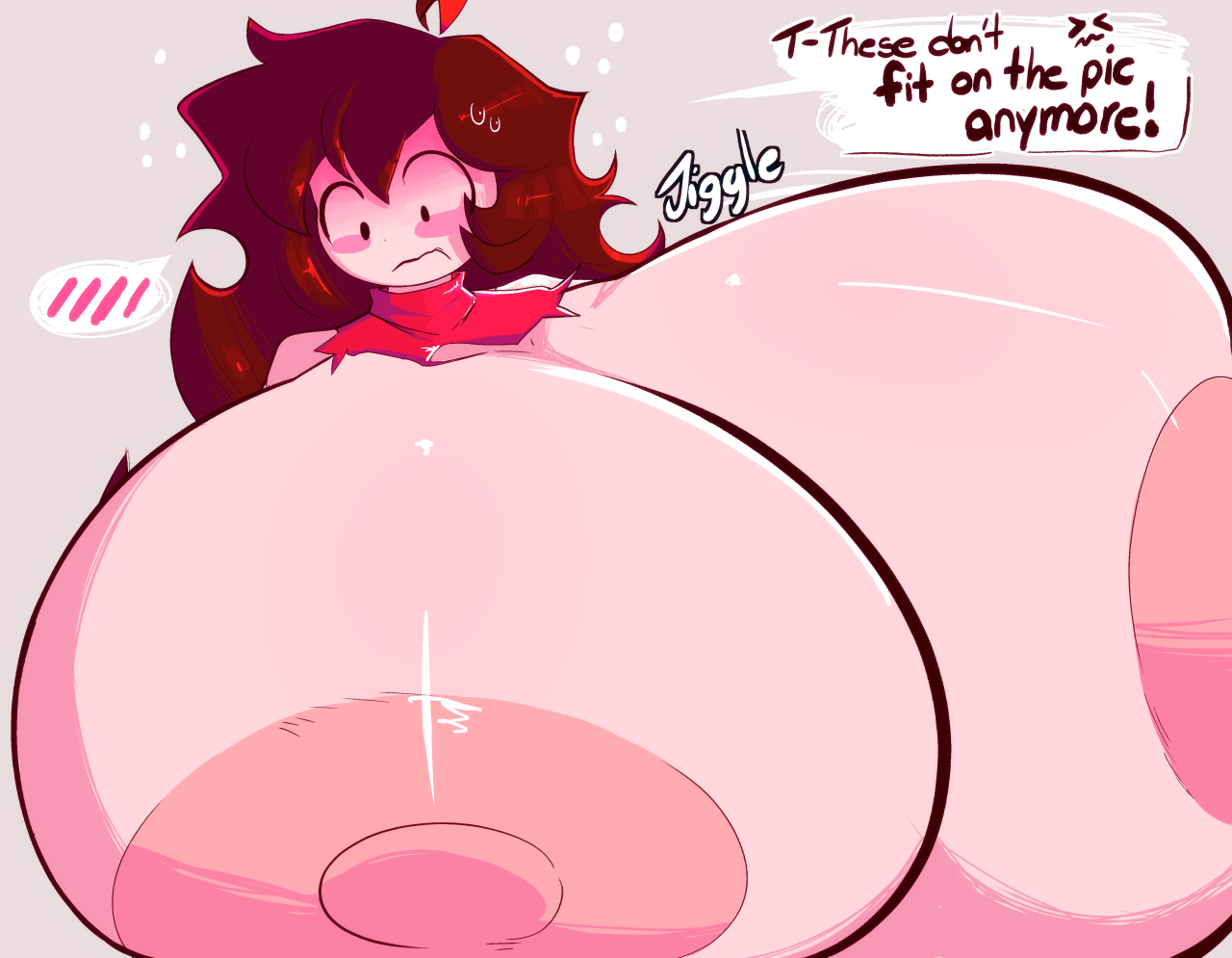
Carnosine and Cellular Health

Carnosine, a naturally occurring dipeptide, plays a crucial role in cellular protection. Its ability to interact with various cellular components and neutralize damaging agents makes it a potential therapeutic candidate for a range of conditions. This section delves into carnosine’s protective mechanisms against cellular damage and its potential impact on inflammation.Carnosine’s remarkable ability to shield cells from harm stems from its unique chemical structure and its capacity to interact with reactive species and damaging agents.
It acts as a potent antioxidant, reducing oxidative stress, a major contributor to cellular aging and disease. This protective effect is particularly important in maintaining healthy tissues and organs.
Cellular Protection against Oxidative Stress, The benefits of carnosine
Carnosine’s antioxidant properties are well-documented. It effectively scavenges reactive oxygen species (ROS), such as free radicals, which can damage cellular components, including proteins, lipids, and DNA. This protection is crucial in preventing cellular dysfunction and promoting longevity. For example, prolonged exposure to UV radiation can generate high levels of ROS, leading to cellular damage and potentially skin aging.
Carnosine’s antioxidant activity could potentially mitigate these effects.
Carnosine and Inflammation Reduction
Inflammation is a complex biological response to harmful stimuli. While necessary for healing, chronic inflammation can contribute to various diseases. Carnosine’s role in reducing inflammation is a promising area of research.
Carnosine is a powerful antioxidant, known for its potential benefits in reducing muscle fatigue and inflammation. Learning more about the amazing properties of sea moss can offer a fascinating perspective on how these natural compounds work together. Check out sea moss everything you need to know for a deep dive into its potential health benefits. Ultimately, understanding the various ways natural compounds like carnosine can support overall health and wellness is crucial for a balanced lifestyle.
- Neutralization of inflammatory mediators: Carnosine can interact with inflammatory molecules, such as cytokines and prostaglandins, potentially reducing their activity and the inflammatory response. This action could have implications for conditions characterized by chronic inflammation.
- Modulation of immune cell activity: Carnosine may influence the activity of immune cells involved in the inflammatory process. This regulation could contribute to a more balanced and controlled immune response.
- Reduction of oxidative stress: As mentioned earlier, carnosine’s antioxidant properties directly contribute to reducing the production of ROS, a key driver of inflammation. Lowering oxidative stress can help calm the inflammatory cascade.
- Inhibition of inflammatory enzymes: Certain enzymes, like cyclooxygenase (COX), play a crucial role in the production of inflammatory mediators. Carnosine may inhibit the activity of these enzymes, thereby decreasing the generation of inflammatory compounds.
- Promoting anti-inflammatory pathways: Carnosine could potentially stimulate cellular pathways that counter inflammation, creating a protective environment against harmful cellular processes.
Protein and Peptide Interactions
Carnosine’s ability to interact with proteins and peptides is critical to its cellular effects. It can bind to various proteins, altering their structure and function. These interactions can have a profound impact on cellular processes.
Carnosine’s interaction with proteins can affect their stability, activity, and susceptibility to damage.
This interaction is particularly relevant in maintaining the integrity of proteins crucial for cellular functions. Furthermore, carnosine may influence protein folding and assembly, ensuring proper cellular structure and function.
Mechanism of Action in Protein and Peptide Interactions
- Hydrogen bonding: Carnosine’s amino acid side chains can form hydrogen bonds with specific amino acid residues in proteins, altering their conformation.
- Electrostatic interactions: Carnosine’s charged groups can participate in electrostatic interactions with proteins, influencing their activity.
- Formation of complexes: Carnosine can form complexes with proteins, potentially modulating their function and stability.
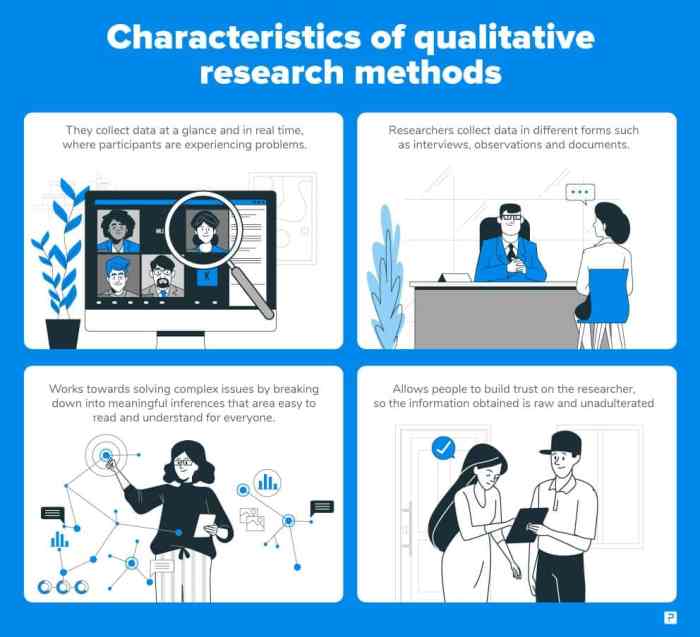
Carnosine and Neurological Health
Carnosine, a naturally occurring dipeptide, has garnered attention for its potential benefits beyond its role in muscle function. Recent research suggests a promising link between carnosine and neurological health, particularly in protecting neurons from damage and potentially mitigating the progression of neurological disorders. This exploration delves into the potential mechanisms and evidence supporting carnosine’s neuroprotective effects.Carnosine’s ability to neutralize harmful reactive oxygen species (ROS) and metal ions is a key aspect of its neuroprotective properties.
These molecules are implicated in neuronal damage, playing a significant role in the pathogenesis of various neurological conditions. By reducing oxidative stress, carnosine may help maintain neuronal integrity and function.
Potential Role in Neuronal Protection
Carnosine acts as a potent antioxidant, scavenging harmful free radicals that can damage cell structures, including neurons. This antioxidant capacity is crucial in preserving the integrity of neuronal membranes and preventing the accumulation of oxidative damage, a hallmark of neurodegenerative diseases. Furthermore, carnosine can chelate metal ions, preventing their harmful interactions with cellular components. This dual action of scavenging free radicals and chelating metals contributes to its overall neuroprotective effect.
Potential Benefits in Managing Neurological Disorders
The potential benefits of carnosine extend to managing neurological disorders like Alzheimer’s disease. Evidence suggests that oxidative stress and metal ion accumulation significantly contribute to the development and progression of Alzheimer’s. By mitigating these damaging factors, carnosine may slow or even halt disease progression. While more research is needed to fully understand the extent of carnosine’s impact on specific neurological disorders, its protective effects on neuronal structures and function provide a basis for further investigation.
For example, studies in animal models have shown promising results regarding memory enhancement and reduced neuronal damage in the presence of carnosine.
Evidence Supporting Neuroprotective Effects
A growing body of research supports carnosine’s neuroprotective properties. In vitro studies have demonstrated carnosine’s ability to protect neurons from various stressors, including oxidative stress and metal ion toxicity. Animal studies have also shown promising results, exhibiting reduced neuronal damage and improved cognitive function in various models of neurological disorders. While human trials are limited, the existing evidence suggests a potential role for carnosine in promoting neuronal health.
For instance, one study showed improvements in cognitive function in patients with mild cognitive impairment after supplementation with carnosine.
Summary Table of Potential Benefits
| Neurological Function | Potential Benefit | Mechanism | Evidence Level |
|---|---|---|---|
| Memory | Improvement | Reduced oxidative stress, improved neuronal function | Moderate |
| Neuroinflammation | Reduction | Antioxidant and anti-inflammatory properties | Emerging |
| Neuron Protection | Increased | Neutralization of harmful free radicals and metal ions | Strong |
| Cognitive Decline | Possible Slowing | Protection of neurons from damage, reduced oxidative stress | Moderate |
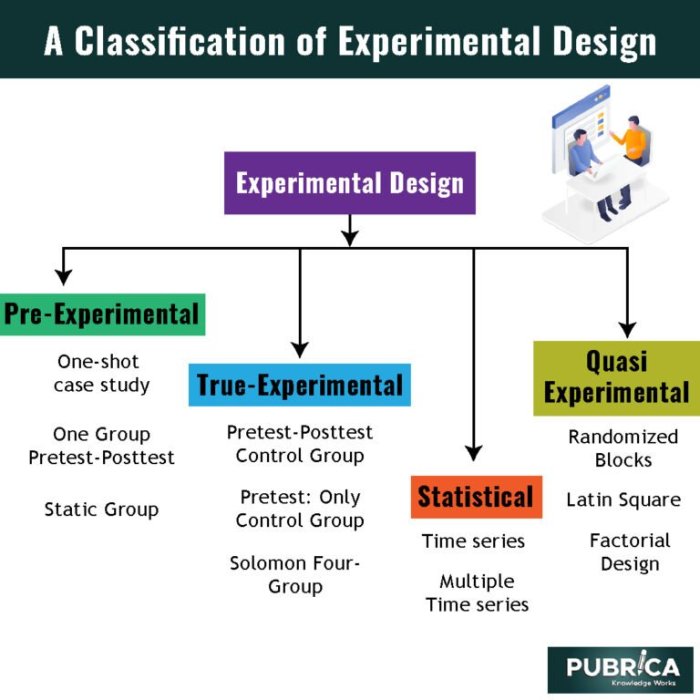
Carnosine and Aging

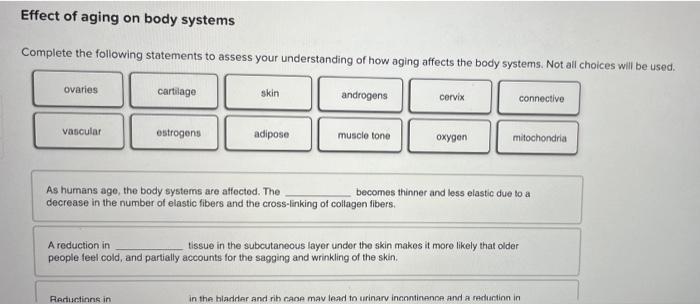
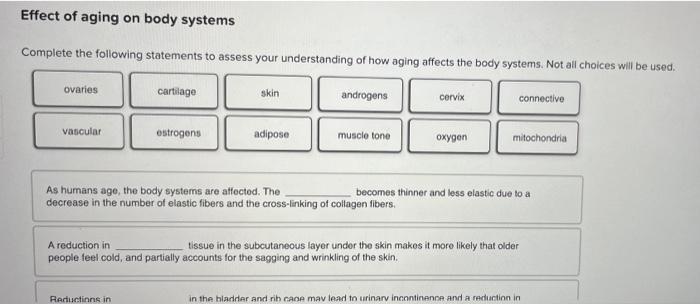
Carnosine, a naturally occurring dipeptide, has garnered attention for its potential role in slowing the aging process. Its antioxidant and anti-inflammatory properties, along with its ability to protect cells from damage, suggest a possible connection between carnosine supplementation and improved healthspan. This exploration dives into the potential mechanisms through which carnosine might combat age-related decline.The aging process is complex, involving various cellular and molecular changes.
Carnosine’s multifaceted action, targeting multiple pathways associated with aging, makes it an intriguing candidate for interventions aimed at extending healthy lifespan. Research continues to investigate the precise ways carnosine influences these pathways, and further studies are needed to fully elucidate its potential in this area.
Potential Mechanisms of Carnosine in Aging
Carnosine’s antioxidant capacity plays a crucial role in mitigating oxidative stress, a significant contributor to cellular damage and aging. It scavenges reactive oxygen species (ROS), thereby protecting cellular components from damage. Further, carnosine’s ability to chelate metal ions can prevent the formation of harmful free radicals. This dual action helps maintain cellular integrity and function as we age.
Carnosine and Cellular Senescence
Cellular senescence, a state of cellular aging and dysfunction, is implicated in age-related diseases. Studies have shown that carnosine can potentially reduce the accumulation of senescent cells. By modulating cellular pathways related to senescence, carnosine may contribute to a healthier aging process. This includes supporting cellular repair mechanisms and preventing the release of damaging factors by senescent cells.
The precise mechanisms through which carnosine influences cellular senescence remain a subject of ongoing research.
Age-Related Processes Affected by Carnosine
Carnosine’s potential impact on aging encompasses various processes. These processes can be broadly categorized into:
- Oxidative Stress Mitigation: Carnosine’s antioxidant properties directly combat oxidative stress, a major driver of cellular damage and aging. By neutralizing free radicals, carnosine protects cellular structures and functions, thus potentially delaying age-related decline.
- Inflammation Regulation: Chronic inflammation is linked to aging and various age-related diseases. Carnosine’s anti-inflammatory effects may help reduce the inflammatory burden, leading to a healthier aging process.
- Protein Damage Repair: Proteins are crucial for cellular function, and their degradation contributes to aging. Carnosine may support protein repair mechanisms, thus potentially mitigating the impact of protein damage associated with aging.
- Cellular Senescence Modulation: The accumulation of senescent cells is associated with age-related diseases. Carnosine may reduce the accumulation of senescent cells, potentially slowing the aging process.
- Neuroprotective Effects: Age-related neurodegenerative diseases are often associated with oxidative stress and inflammation. Carnosine’s neuroprotective effects may contribute to preserving cognitive function and overall neurological health as we age.
- Mitochondrial Function: Mitochondria, the powerhouses of cells, play a vital role in cellular function. Carnosine may support mitochondrial function, which is crucial for maintaining cellular energy production and overall health as we age.
Carnosine and Food Sources
Carnosine, a naturally occurring dipeptide, is found in various foods. While not a primary dietary focus, incorporating foods rich in carnosine into your diet could contribute to overall health, particularly if you’re interested in its potential benefits. Understanding the food sources of carnosine, along with their carnosine content and potential bioavailability, is essential for anyone looking to potentially leverage its properties.A significant portion of carnosine in the human body is derived from dietary intake.
However, the exact amount of carnosine present in different foods and the degree to which it’s absorbed by the body can vary. This is influenced by several factors, including food preparation methods.
Carnosine, a naturally occurring compound, offers a range of potential health benefits. Knowing your family’s medical history is crucial when considering the benefits of carnosine, as certain conditions might be linked to its effectiveness. For instance, understanding your family’s predisposition to specific diseases, like heart conditions or muscle disorders, can help you tailor a strategy that aligns with your unique genetic background.
Recording family medical history can help you uncover these patterns and make informed decisions about your health, leading to a more effective strategy for harnessing the benefits of carnosine for your specific needs. This proactive approach allows you to gain a deeper understanding of how your body might react to carnosine.
Food Sources Rich in Carnosine
A variety of foods contain carnosine, although the concentration can differ significantly. Meat products, particularly red meat, are known to be relatively high in carnosine. However, other sources, like some seafood and certain plant-based foods, may also contribute to carnosine intake.
| Food | Carnosine Content (mg/100g) | Other Nutrients | Preparation Methods |
|---|---|---|---|
| Beef | High | Protein, Iron, Zinc | Cooked |
| Pork | Moderate | Protein, Vitamin B | Cooked, cured |
| Salmon | Low | Omega-3 fatty acids, Vitamin D | Baked, grilled, or pan-fried |
| Chicken | Moderate | Protein, Vitamin B | Roasted, grilled, or fried |
| Certain Mushrooms | Trace Amounts | Fiber, Vitamins | Sautéed, roasted, or added to soups |
Bioavailability of Carnosine from Different Food Sources
The bioavailability of carnosine, meaning how much of the carnosine in food is actually absorbed and used by the body, varies depending on the food source. Factors like the presence of other nutrients, the form of carnosine in the food, and the individual’s digestive health can influence how well the body absorbs carnosine. While meat products often have higher carnosine content, the bioavailability might not always be as high as other potential sources.
Effect of Cooking Methods on Carnosine Content
Cooking methods can impact the carnosine content in food. Heat, particularly high heat, can potentially degrade carnosine, resulting in a lower concentration in the cooked food compared to the raw material. Methods that involve prolonged cooking or high temperatures may have a more significant effect on the carnosine levels. For example, roasting meat at high temperatures for extended periods might result in a noticeable decrease in carnosine compared to shorter cooking times.
Steaming or lightly grilling might preserve more carnosine than deep frying.
Carnosine and Safety
Carnosine, a naturally occurring dipeptide, has garnered attention for its potential health benefits. However, like any supplement, it’s crucial to understand the potential risks and responsible usage. This section delves into the safety considerations surrounding carnosine supplementation, covering potential side effects, toxicity concerns, recommended dosages, and the importance of professional guidance.Understanding the potential side effects and safety profile of carnosine is vital for anyone considering supplementation.
While generally considered safe, individual responses can vary, and careful monitoring is essential.
Potential Side Effects
The majority of studies on carnosine supplementation report a good safety profile. However, some potential side effects have been noted in certain individuals. These side effects are typically mild and transient, resolving upon discontinuation of the supplement.
- Gastrointestinal issues, such as nausea, vomiting, and diarrhea, have been reported in some cases.
- Headaches and dizziness have also been reported in a small number of individuals.
- Allergic reactions, though rare, are possible.
Current Understanding of Carnosine Toxicity
While carnosine is generally considered safe, there’s a limited understanding of potential long-term toxicity. Current research suggests that carnosine is unlikely to cause severe or permanent adverse effects at recommended dosages. However, further research is warranted to fully elucidate the long-term effects of carnosine supplementation. There are no reported cases of severe carnosine toxicity in the scientific literature.
Recommended Dosage
The recommended dosage of carnosine varies depending on the specific product and the intended use. Currently, there isn’t a standardized, universally accepted dosage for all individuals. The optimal dosage is best determined through consultation with a healthcare professional. The most commonly studied doses range from 2 grams to 6 grams per day, but individual needs may vary.
Importance of Consulting a Healthcare Professional
Given the varying individual responses and the limited research on long-term effects, consulting a healthcare professional before taking carnosine supplements is highly recommended. This consultation is especially crucial for individuals with pre-existing health conditions, such as kidney problems or liver disease, as carnosine can potentially interact with certain medications or conditions. A healthcare professional can assess individual needs, potential interactions, and tailor a safe and effective supplementation strategy, if any.
Final Conclusion: The Benefits Of Carnosine
In conclusion, carnosine presents a fascinating array of potential benefits, impacting various aspects of health and well-being. From supporting muscle function and protecting against oxidative stress to potentially influencing neurological health and delaying the aging process, the evidence surrounding carnosine’s capabilities is promising. However, more research is crucial to fully understand its mechanisms and optimal use. This article highlights the current knowledge and potential applications, but individual responses to carnosine may vary.