How ACL surgery is performed is a complex procedure, but understanding the process can ease anxieties. This in-depth look explores the various stages, from initial diagnosis to post-operative rehabilitation, offering a clear and concise overview of the entire journey. We’ll delve into pre-operative assessments, surgical techniques, and the critical role of post-operative care in achieving optimal recovery. Get ready to gain valuable insights into this essential medical procedure.
The anterior cruciate ligament (ACL) plays a crucial role in knee stability. Tears to this vital ligament often require surgical intervention. This guide details the steps involved in ACL reconstruction, from diagnosing the injury to the long-term rehabilitation process. Different surgical approaches, graft options, and post-operative care protocols are also discussed, providing a holistic understanding of the procedure.
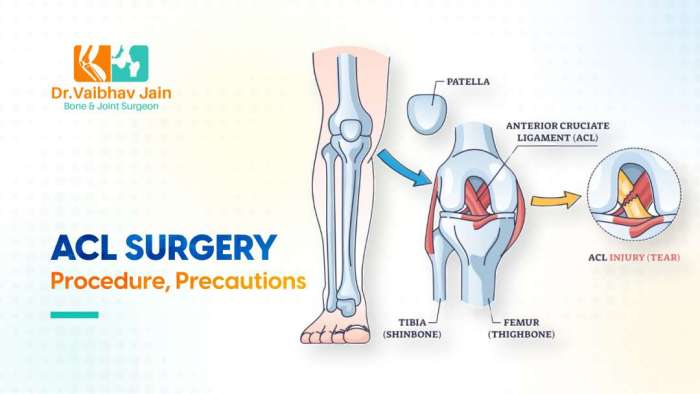
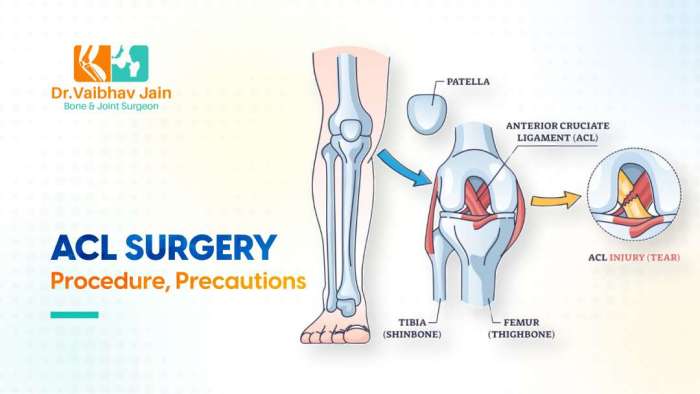
Introduction to ACL Surgery
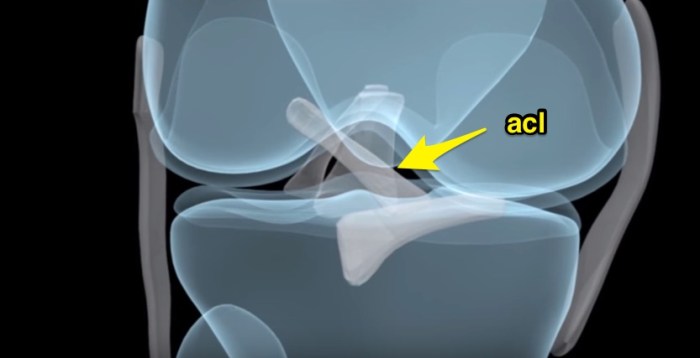
The anterior cruciate ligament (ACL) is a crucial part of the knee joint, acting as a stabilizer, preventing excessive forward movement of the tibia (shinbone) relative to the femur (thighbone). It’s a key component in maintaining knee joint stability during various activities, especially those involving twisting, pivoting, and cutting. Understanding its function is essential to grasping the impact of an injury.Common causes of ACL tears include sudden stops and changes in direction, direct blows to the knee, and landing awkwardly from a jump.
These forceful movements can overstretch or tear the ACL, often resulting in significant pain and instability. The severity of the injury can vary greatly, from a minor sprain to a complete tear. Knowing the potential causes helps in prevention strategies and early intervention.Prompt diagnosis and treatment are vital for optimal recovery and minimizing long-term complications. Delayed intervention can lead to chronic knee instability, osteoarthritis, and a diminished quality of life.
Early diagnosis allows for timely intervention, potentially avoiding the need for surgical repair in less severe cases. This underscores the importance of seeking medical attention promptly when experiencing knee pain or instability.The overarching goals of ACL surgery are to restore knee stability, alleviate pain, and allow patients to return to their pre-injury activity levels. This often involves a surgical procedure to reconstruct the ACL using grafts from other parts of the body or from donor tissue.
The recovery process typically includes physical therapy to regain strength and range of motion.
History of ACL Surgical Techniques
Early attempts at ACL repair involved simple suturing techniques. These methods, however, often proved insufficient to restore proper knee function. Over time, advancements in surgical techniques and materials led to the development of more robust and effective repair methods. Early 20th-century approaches focused on securing the ligament ends with sutures, but these often failed to provide adequate stability.
As our understanding of the ligament and the knee joint improved, the use of autografts (grafts from the patient’s own body) gained traction. These methods, while still requiring significant rehabilitation, provided more predictable results. More recent techniques have incorporated advancements in graft harvesting and fixation methods, further refining the surgical process and improving long-term outcomes. One significant advancement involved the use of allograft tissue, which provides an alternative source of graft material.
These techniques are now considered standard practice, demonstrating the continuous evolution of ACL surgical procedures.
Common Causes of ACL Tears
Sudden stops and changes in direction are frequent causes of ACL tears. For example, a basketball player abruptly stopping to avoid a collision often puts immense stress on the knee, potentially leading to a tear. Direct blows to the knee can also cause damage. In a football game, a forceful impact to the side of the knee can directly injure the ACL.
Landing awkwardly from a jump is another common cause, such as in volleyball or basketball. The forces generated during landing, especially when the foot is not properly positioned, can result in a tear.
Importance of Timely Diagnosis and Treatment
Early diagnosis and prompt treatment are critical in minimizing long-term problems. For instance, a patient who delays seeking medical attention might develop chronic knee instability, leading to a higher risk of subsequent injuries. Delayed treatment can also increase the likelihood of developing osteoarthritis in the affected knee. This underscores the significance of early intervention and appropriate medical care.
Overall Goals of ACL Surgery
Restoring knee stability is a primary goal. This is achieved through surgical reconstruction of the ACL, using a variety of grafts and techniques. Pain relief is another important objective. The surgical procedure aims to reduce pain and discomfort associated with the injury. Ultimately, enabling patients to resume their pre-injury activity levels is the desired outcome.
This involves a rigorous rehabilitation program, aimed at strengthening the knee muscles and improving range of motion.
Pre-operative Assessment and Planning
Before embarking on ACL reconstruction surgery, a thorough pre-operative assessment is crucial. This meticulous process ensures the patient’s well-being, the surgeon’s understanding of the injury, and the optimal selection of the surgical technique. This phase goes beyond simply confirming the tear; it involves a comprehensive evaluation to personalize the surgical approach for the best possible outcome.Accurate diagnosis and meticulous planning are fundamental to successful ACL surgery.
This phase focuses on identifying the precise nature of the injury, evaluating the patient’s overall health, and tailoring the surgical approach to individual needs. The pre-operative process aims to minimize risks and maximize the chance of a positive recovery.
ACL surgery involves meticulously repairing or replacing the anterior cruciate ligament, often using grafts from the patient’s own body or synthetic materials. Understanding the nuances of pain, like differentiating kidney pain from back pain, can be crucial in diagnosing and treating sports injuries. For example, if you’re experiencing pain in your lower back or side, knowing the distinction between kidney pain vs back pain could significantly impact the path to recovery.
The surgical procedure itself requires careful attention to detail and precise placement of the new ligament to ensure long-term stability and function.
Diagnostic Procedures for ACL Tears
Various diagnostic procedures are employed to confirm an ACL tear. These procedures include physical examinations, imaging studies, and potentially arthroscopy. Physical examinations involve evaluating joint stability, range of motion, and palpating for tenderness or swelling.Imaging studies, such as MRI (Magnetic Resonance Imaging), are crucial for visualizing the ligaments and surrounding tissues. MRI scans provide detailed images of the knee joint, allowing for the precise identification of the ACL tear, its extent, and associated injuries.
X-rays may also be taken to rule out any fractures or other bony abnormalities. Arthroscopy, a minimally invasive procedure, involves inserting a small camera into the knee joint to directly visualize the ACL and other structures. This direct visualization can confirm the diagnosis and potentially identify associated damage. Combining these techniques ensures a definitive diagnosis and informs the surgical plan.
Patient Evaluation Steps
Comprehensive patient evaluation involves a series of steps to assess their suitability for surgery. A detailed medical history, including previous injuries and medical conditions, is essential. This information helps identify potential risks and complications. Physical examinations assess the knee’s range of motion, strength, and stability. Neurological assessments are performed to ensure proper nerve function and sensation in the affected limb.This process also involves a detailed discussion of the patient’s expectations and any concerns.
Open communication with the patient is crucial for building trust and addressing their questions. This includes explaining the surgical procedure, potential risks, and the recovery process. This holistic approach ensures informed consent and shared decision-making.
Surgical Technique Selection Factors
Several factors influence the choice of surgical technique. These include the severity of the tear, the patient’s age, activity level, and any pre-existing conditions. The surgeon also considers the desired outcome, aiming for optimal knee stability and function. Graded severity of ACL tears and associated damage are assessed.Different surgical approaches cater to various patient profiles. The choice between a traditional graft or a newer, less invasive approach, considers factors like the patient’s activity level and desired recovery time.
Each technique has advantages and disadvantages, and the optimal approach is tailored to the individual.
Importance of Patient Preparation and Counseling
Thorough patient preparation and counseling are vital for a successful surgical outcome. This involves educating the patient about the surgical procedure, potential risks and complications, and the post-operative recovery process. This preparation also includes discussing realistic expectations for recovery and rehabilitation.Counseling helps manage anxiety and concerns, fostering a positive attitude toward the recovery journey. This proactive approach empowers the patient and contributes to better adherence to post-operative instructions.
Essential Pre-operative Information
| Category | Information |
|---|---|
| Medical History | Previous injuries, allergies, medications, medical conditions, and current health status. |
| Imaging Results | MRI, X-ray findings, and any other relevant imaging studies. |
| Physical Assessments | Range of motion, strength, stability, and neurological function of the affected knee. |
| Activity Level | Patient’s sport or activity level, desired return to activity timeline, and lifestyle. |
| Patient Expectations | Understanding the patient’s expectations, concerns, and goals for surgery. |
Surgical Techniques
ACL reconstruction surgery involves carefully restoring the torn anterior cruciate ligament (ACL) using various techniques and materials. The choice of approach and graft type depends on several factors, including the patient’s age, activity level, and the extent of the injury. Surgical precision and meticulous attention to detail are crucial for optimal outcomes and minimizing the risk of complications.
Surgical Approaches
Different surgical approaches are used for ACL reconstruction, each with its own advantages and disadvantages. Minimally invasive techniques are increasingly popular, offering smaller incisions and potentially faster recovery times. These approaches often use specialized instruments and techniques to access the knee joint. Traditional open approaches, while providing greater visualization, may result in larger scars and a slightly longer recovery period.
Graft Options
Choosing the right graft is essential for ACL reconstruction. Autografts, derived from the patient’s own tissue, and allografts, sourced from a donor, are the two main types. The selection of a graft type often depends on factors like the patient’s overall health, the specific characteristics of the injury, and the surgeon’s preference.
Autograft Harvesting
Autografts are frequently harvested from the patient’s own body. Common sources include the hamstring tendons and the patellar tendon. Hamstring tendon harvesting involves taking a portion of the semitendinosus and gracilis tendons. Patellar tendon autografts are derived from the central portion of the patellar tendon, along with a segment of the bone from the tibia and patella.
Proper surgical technique during harvesting is critical to minimize potential complications like nerve damage, muscle weakness, and stiffness.
- Hamstring Tendon Autograft: This technique involves carefully isolating and preparing the semitendinosus and gracilis tendons, preserving their blood supply to promote healing. The tendons are then prepared for implantation, often by carefully shaping and sizing them.
- Patellar Tendon Autograft: In this approach, a section of the patellar tendon, along with a portion of the bone from the patella and tibia, is carefully harvested. This technique necessitates precise surgical incisions to minimize potential complications and ensure a strong graft. Post-operative care and rehabilitation are crucial to minimize potential complications.
Allograft Preparation and Implantation
Allografts, derived from cadaveric tissue, provide a readily available alternative to autografts. They undergo rigorous testing and processing to ensure safety and compatibility. Allograft preparation involves sterilization and processing to remove any potential contaminants or disease agents. Implants are meticulously sized and prepared to fit the patient’s anatomy, ensuring a secure and stable reconstruction.
Graft Fixation Techniques
Various techniques are employed to secure the graft within the knee joint. These methods include using screws, interference devices, or a combination of both. The choice of fixation technique depends on several factors, including the graft type and the surgeon’s preference. Careful placement and tensioning of the graft are essential for optimal function and stability.
Comparison of Graft Types
| Graft Type | Advantages | Disadvantages |
|---|---|---|
| Hamstring Autograft | Generally considered to have a low risk of complications, potential for a faster recovery, lower risk of anterior knee pain. | May lead to hamstring weakness or discomfort. |
| Patellar Tendon Autograft | Strong graft, often a reliable option for patients requiring high-demand activities. | Higher risk of anterior knee pain, potential for patellar tracking issues. |
| Allograft | Readily available, minimizes the risk of complications. | Potential for rejection, possibility of disease transmission (extremely rare with modern sterilization methods). |
Minimally Invasive Techniques, How acl surgery is performed
Minimally invasive ACL reconstruction techniques involve smaller incisions and specialized instruments. These methods often utilize arthroscopic procedures, allowing for precise visualization and manipulation of the knee joint. The benefits include less postoperative pain, faster recovery, and smaller scars. However, these techniques demand highly skilled surgeons with expertise in arthroscopic surgery.
Post-operative Care and Rehabilitation
The journey to recovery after ACL surgery is a marathon, not a sprint. Post-operative care and rehabilitation are crucial for a successful return to activity. This phase focuses on restoring strength, range of motion, and function while minimizing the risk of complications. Patience and adherence to the prescribed plan are paramount.Immediate post-operative care lays the foundation for a smooth recovery.
Close monitoring and adherence to the prescribed protocol are essential for optimal healing and minimizing potential complications. This crucial period sets the stage for the long-term rehabilitation process.
Immediate Post-Operative Care
The first few days following ACL surgery are critical. Pain management, swelling control, and meticulous wound care are paramount. Ice packs, compression bandages, and elevation are vital to minimize swelling and promote healing. Medications prescribed by the surgeon are critical for managing pain and inflammation. Early mobilization, with guidance from physical therapists, is essential to prevent stiffness and promote circulation.
A dedicated support system is invaluable, helping with daily tasks and providing emotional support.
Importance of Physical Therapy
Physical therapy is an integral part of the ACL rehabilitation process. It provides tailored exercises and guidance to restore strength, mobility, and function. A qualified physical therapist designs a personalized plan that addresses individual needs and goals. This plan helps to regain full range of motion, restore muscle strength, and improve proprioception (the body’s awareness of its position in space).
Physical therapy is essential for preventing long-term complications and ensuring a safe and effective recovery.
Phases of Rehabilitation
Rehabilitation typically involves distinct phases, each with specific goals. These phases are designed to progressively challenge the healing tissues and restore function. Understanding each phase and its objectives is essential for patient compliance and success.
Phase 1: Early Recovery (0-4 weeks)
This phase prioritizes pain management, swelling reduction, and regaining a full range of motion. Exercises focus on gentle range-of-motion exercises, isometric contractions (muscle contractions without movement), and light cardiovascular activities. Examples include gentle knee flexion and extension exercises, ankle pumps, and stationary bike riding. A gradual increase in activity is crucial, avoiding overexertion.
Phase 2: Strengthening and Proprioception (4-8 weeks)
This phase emphasizes the strengthening of the muscles surrounding the knee joint and improving proprioception. Exercises progress to include light resistance training, balance exercises, and functional activities. Examples include hamstring curls, quadriceps sets, and exercises that challenge balance on unstable surfaces. Progression should be gradual and pain-free.
Phase 3: Functional Training (8-12 weeks)
This phase focuses on preparing the patient for return to sport-specific activities. Exercises incorporate agility drills, plyometrics (jumping and hopping exercises), and sport-specific movements. Examples include lateral shuffles, single-leg hops, and drills mimicking the movements of the patient’s sport. This phase ensures the patient is prepared to safely return to their chosen activities.
ACL surgery involves carefully repairing or replacing the torn ligament. It’s a complex procedure, but thankfully, advancements in techniques have made it less invasive. While I’m no doctor, I’m fascinated by the different approaches to reconstructing this crucial knee ligament. Learning about the various types of toenail fungus types of toenail fungus is fascinating too, but getting back to the surgery, it’s all about precise placement and the use of grafts or other materials to restore full function.
Ultimately, the goal is always to get patients back on their feet, so to speak.
Phase 4: Return to Sport (12+ weeks)
The final phase focuses on returning to the patient’s pre-injury level of activity. This includes advanced agility training, plyometrics, and sport-specific drills. Exercises are tailored to the specific demands of the patient’s sport. It is crucial to monitor for any signs of pain or instability.
Potential Complications and Management
Potential complications include persistent pain, swelling, stiffness, and instability. These issues are addressed through a combination of medication, physical therapy, and in some cases, further surgical intervention. Early detection and appropriate management are critical in minimizing the impact of these complications. A dedicated team of healthcare professionals ensures the patient receives comprehensive care.
Key Milestones in ACL Rehabilitation
| Phase | Timeline (Weeks) | Key Exercises |
|---|---|---|
| Early Recovery | 0-4 | Gentle range-of-motion exercises, isometric contractions, light cardio |
| Strengthening & Proprioception | 4-8 | Resistance training, balance exercises, functional activities |
| Functional Training | 8-12 | Agility drills, plyometrics, sport-specific movements |
| Return to Sport | 12+ | Advanced agility, plyometrics, sport-specific drills |
Creating a Structured Exercise Plan
A structured exercise plan for ACL rehabilitation is crucial. This plan should be personalized, taking into account the patient’s specific needs and goals. It should include a progressive increase in intensity and difficulty, ensuring that exercises are performed correctly and pain-free. Regular progress assessments are vital to ensure that the plan remains effective and safe.
Considerations for Different Patient Profiles: How Acl Surgery Is Performed
ACL reconstruction surgery is a complex procedure, and its success hinges on carefully considering individual patient needs. Factors like age, activity level, and pre-existing conditions significantly influence surgical technique, rehabilitation protocols, and long-term outcomes. Tailoring the approach to each patient profile ensures optimal results and minimizes potential complications.
ACL Reconstruction in Children
Children’s growing skeletons present unique challenges in ACL reconstruction. The goal is to rebuild the ligament while preserving the growth plates, which are crucial for proper bone development. Techniques often involve smaller incisions and less invasive approaches to minimize the risk of impacting the growth plates. The use of autografts (tissue from the patient) may be preferred over allografts (tissue from a donor) in some cases due to the potential for graft rejection with allografts.
The long-term success of reconstruction in children is also influenced by their growth and activity levels, demanding meticulous monitoring and rehabilitation plans tailored to their age.
Surgical Considerations for Athletes
Athletes, particularly those in high-impact sports, require specific surgical and rehabilitation strategies to ensure they can return to their pre-injury performance levels. Surgical techniques must consider the demanding nature of their sport and the need for rapid healing and strengthening. This often involves meticulous graft placement, precise fixation techniques, and rigorous post-operative rehabilitation programs that are tailored to the specific demands of the sport.
Examples include customized strength training programs, agility drills, and sport-specific exercises.
Special Needs of Patients with Pre-existing Conditions
Patients with pre-existing conditions, such as diabetes, obesity, or cardiovascular issues, require careful assessment and modification of the surgical plan. These conditions can impact the healing process and increase the risk of complications. The surgical team must consider these factors when determining the optimal approach, anesthesia protocols, and post-operative care. For example, patients with diabetes may need closer monitoring of blood sugar levels during and after surgery.
Importance of Patient Education and Compliance
Patient education and compliance are critical to the success of ACL reconstruction. Understanding the procedure, rehabilitation protocols, and potential risks empowers patients to actively participate in their recovery. Clear communication about the expected recovery timeline, home exercises, and potential setbacks is crucial. Compliance with post-operative instructions, including medication adherence and adherence to rehabilitation schedules, directly affects the likelihood of a successful outcome.
Furthermore, understanding the potential need for long-term follow-up is essential for patients to proactively manage their recovery.
Importance of Long-Term Follow-Up and Monitoring
Long-term follow-up is essential to assess the long-term success of ACL reconstruction. Regular check-ups allow the monitoring of the graft’s integration, stability, and the patient’s overall joint health. These checkups also allow for the early detection of any complications, such as osteoarthritis or recurrent instability, enabling timely intervention and management.
Key Differences in ACL Surgery for Different Age Groups
| Age Group | Surgical Technique Considerations | Rehabilitation Protocol Considerations | Long-Term Follow-up Needs |
|---|---|---|---|
| Children (pre-puberty) | Minimally invasive techniques, growth plate preservation, smaller incisions | Gradual progression, focus on functional recovery, close monitoring of growth plates | Long-term monitoring for growth and potential instability |
| Adolescents (puberty) | Balancing growth plate preservation with ligament reconstruction, potential for growth spurts | Gradual progression with focus on strength and flexibility, consideration of future sport participation | Monitoring for long-term stability, potential for osteoarthritis |
| Adults | Various graft options, precise surgical technique, focus on stability and function | Gradual progression, focus on functional recovery, sport-specific training if applicable | Monitoring for long-term stability, potential for osteoarthritis |
Surgical Tools and Instruments
The meticulous selection and precise use of surgical tools are critical to the success of ACL reconstruction. Careful consideration of each instrument’s functionality, combined with the surgeon’s experience and the patient’s specific needs, minimizes complications and maximizes positive outcomes. This section delves into the essential tools and instruments used in ACL reconstruction, focusing on their roles in graft preparation, fixation, and arthroscopic visualization.Surgical instruments, ranging from specialized arthroscopic shavers to precise bone-drilling devices, are carefully chosen to match the surgeon’s technique and the patient’s unique anatomy.
Factors such as the type of graft used, the patient’s bone structure, and the surgeon’s preference all contribute to the selection process. Proper instrumentation minimizes tissue trauma, promotes optimal healing, and contributes to a faster recovery for the patient.
ACL surgery involves meticulously repairing or reconstructing the anterior cruciate ligament. Doctors use tiny instruments and precise techniques to reattach the torn ligament, often using grafts from the patient’s own body or donor tissue. While recovering from this procedure, it’s important to focus on a healthy diet, and understanding the different treatments for iron deficiency anemia options can also be beneficial for overall healing.
This is because proper nutrition is crucial for tissue repair and a strong immune response, making it essential for a speedy recovery from ACL surgery.
Graft Preparation Instruments
A critical step in ACL reconstruction involves preparing the graft tissue for implantation. The precise handling of the graft is essential to ensure its optimal strength and biocompatibility. This involves specialized instruments designed to maintain the integrity of the graft while shaping it to fit the recipient site.
- Arthroscopic Graft Shavers: These tools are used to carefully trim and shape the graft, ensuring a precise fit within the bone tunnels. Their sharp edges and controlled cutting action help to maintain the integrity of the graft and prevent damage to surrounding tissues. They come in various sizes and shapes, allowing for tailored adjustments based on the graft type and the patient’s anatomy.
For example, a hamstring graft might require a different shaver profile than a patellar tendon graft.
- Bone-Drilling Instruments: Used to create the tunnels in the femur and tibia, these tools are crucial for securing the graft. High-speed drills with precise control are essential to avoid damaging the surrounding structures and ensuring the tunnels are of the correct diameter and depth. Variations in drill bits accommodate different graft types and bone densities.
- Osteotomes and Elevators: These instruments are used to carefully elevate and prepare the bone for tunnel creation, ensuring a smooth and precise surgical approach. They are crucial for shaping and preparing the bone surface to receive the graft. Careful use of these instruments minimizes the risk of damage to the surrounding tissues and promotes a stable healing environment.
Fixation Instruments
The fixation of the graft is equally important to ensure long-term stability and functionality. Specialized instruments are used to secure the graft within the bone tunnels, providing the necessary tensile strength for the knee joint.
- Arthroscopic Anchors and Screws: These instruments are used to secure the graft to the bone tunnels. Different types of anchors and screws are available to match various graft types and bone conditions. They provide a strong and stable fixation point, preventing the graft from loosening over time. For instance, bioabsorbable screws might be suitable for certain patients, offering an alternative to metal screws.
- Bioabsorbable Fixation Devices: These devices offer a temporary fixation point during the initial healing phase, with the advantage of gradually dissolving over time. This minimizes the risk of metal allergies or infections, potentially improving long-term outcomes.
Arthroscopic Cameras and Accessories
The arthroscopic camera plays a vital role in providing real-time visualization during the surgical procedure. High-quality cameras with advanced features are essential to ensure optimal visualization and precision.
- Arthroscopic Cameras: Different cameras offer various features, including different magnification levels, image clarity, and the ability to capture high-resolution images and videos. These cameras aid in the visualization of the surgical site and allow the surgeon to accurately assess the condition of the ACL and surrounding tissues. The choice between different cameras often depends on the surgeon’s preference and the complexity of the procedure.
- Arthroscopic Light Sources: The quality of the light source significantly affects the visibility of the surgical site. Strong, focused light helps the surgeon see the critical structures and perform the procedure with greater precision.
Factors Influencing Tool Selection
The selection of surgical tools is influenced by various factors, including the type of graft, the patient’s specific anatomy, the surgeon’s technique, and the level of experience.
- Graft Type: The type of graft (hamstring, patellar tendon, or allograft) directly influences the choice of instruments for preparation and fixation. Different grafts require different techniques and tools for optimal results.
- Patient Anatomy: Variations in bone structure, joint alignment, and soft tissue conditions influence the selection of specific instruments for accurate and efficient tunnel creation and graft fixation.
- Surgeon’s Experience and Preference: The surgeon’s level of expertise and personal preference play a role in selecting the specific instruments and techniques used during the procedure.
Surgical Tool Illustrations
Unfortunately, I cannot create images or illustrations. However, reliable online resources and medical textbooks often contain visual representations of the instruments described above. Searching for “ACL reconstruction instruments” on reputable medical websites can provide detailed images.
Potential Complications and Prevention
ACL surgery, while a crucial procedure for restoring knee function, carries potential risks. Understanding these complications and the strategies to prevent them is essential for both patients and surgeons. Proper pre-operative assessment, meticulous surgical technique, and a comprehensive post-operative rehabilitation program all contribute to minimizing these risks. This section will delve into potential complications, their causes, and effective prevention and management strategies.
Potential Complications
ACL reconstruction, like any surgical procedure, carries the risk of complications. These can range from minor issues like infection to more significant problems like graft failure or persistent pain. Recognizing these potential problems is crucial for developing proactive strategies to mitigate them. Thorough post-operative monitoring and a patient-centered approach are paramount in addressing these complications effectively.
Infection
Infections, although less frequent, are a potential concern after any surgical procedure. The risk of infection is directly correlated with the extent of the surgical procedure and the patient’s overall health. Maintaining a sterile surgical field, administering prophylactic antibiotics, and monitoring the patient closely for signs of infection are critical in minimizing this risk. Strict adherence to post-operative wound care instructions plays a significant role in preventing infection.
Graft Failure
Graft failure is a significant concern that can impact the long-term success of ACL reconstruction. The graft, a tendon or ligament substitute, can weaken or tear over time. Factors contributing to graft failure include inadequate graft healing, improper surgical technique, and patient-specific factors, such as poor compliance with rehabilitation protocols. The choice of graft type, surgical technique, and patient adherence to post-operative instructions influence the risk of graft failure.
Persistent Pain
Persistent pain after ACL surgery is a common complaint, often stemming from factors such as inadequate pain management, improper healing, or complications related to the surgical procedure. Careful pain management strategies, including medication and physical therapy, are crucial in managing pain post-operatively. Prompt and accurate diagnosis of the source of persistent pain is essential for effective management.
Nerve Damage
Nerve damage is a rare but possible complication of ACL surgery. It can result from surgical instruments or techniques, potentially affecting sensation and function in the affected area. Minimizing the risk involves careful surgical technique, precise instrument placement, and ongoing assessment of nerve function. Proper patient positioning and the use of advanced surgical instruments can help mitigate nerve damage.
Arthrofibrosis
Arthrofibrosis, the formation of scar tissue within the joint, can restrict knee motion and function. It can result from various factors, including inflammation, inadequate mobilization, and certain surgical techniques. Early and aggressive physiotherapy, focusing on range of motion exercises, can help prevent arthrofibrosis. This meticulous attention to rehabilitation protocols is crucial in preventing this complication.
Table of Potential Complications
| Potential Complications | Causes | Prevention Strategies |
|---|---|---|
| Infection | Compromised surgical technique, poor wound care, weakened immune system | Strict surgical asepsis, prophylactic antibiotics, meticulous wound care, vigilant monitoring |
| Graft Failure | Inadequate graft healing, improper surgical technique, patient non-compliance with rehabilitation | Appropriate graft selection, meticulous surgical technique, thorough post-operative rehabilitation |
| Persistent Pain | Inadequate pain management, improper healing, surgical complications | Effective pain management protocols, diligent monitoring for complications, appropriate rehabilitation |
| Nerve Damage | Surgical instruments or techniques, improper patient positioning | Careful surgical technique, precise instrument placement, patient positioning, nerve monitoring |
| Arthrofibrosis | Inflammation, inadequate mobilization, certain surgical techniques | Early and aggressive physiotherapy, range of motion exercises, close monitoring |
Ongoing Patient Monitoring
Ongoing patient monitoring is critical for identifying and addressing complications promptly. Regular follow-up appointments, physical examinations, and functional assessments help detect any signs of complications early. This proactive approach ensures that any problems are addressed before they escalate. Patient education about recognizing potential problems and promptly reporting symptoms is crucial for effective management.
Conclusive Thoughts
In conclusion, ACL surgery is a significant undertaking, demanding meticulous planning and execution. From the initial assessment and surgical techniques to the crucial post-operative rehabilitation, every step is critical in ensuring a successful outcome. This guide highlights the multifaceted nature of ACL reconstruction, emphasizing the importance of individual patient needs and the tailored approach necessary for optimal recovery.
Understanding the procedure from start to finish can empower patients and their families to make informed decisions about their healthcare.