ACL tears after surgery present a unique challenge, requiring careful consideration of the recovery process. This guide delves into the complexities of ACL reconstruction, from surgical techniques to potential complications and the crucial role of post-surgical rehabilitation. Understanding the nuances of this journey is key to successful outcomes.
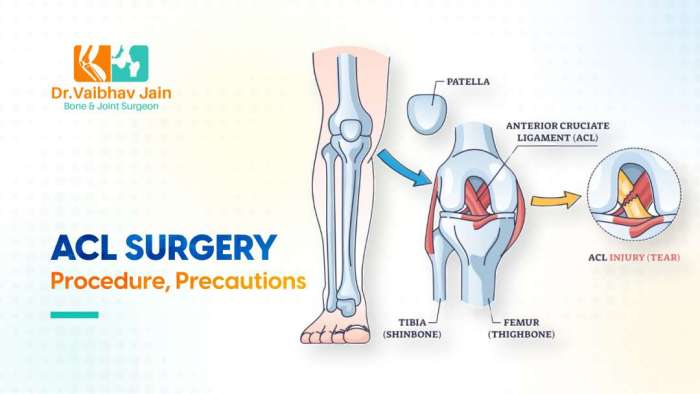
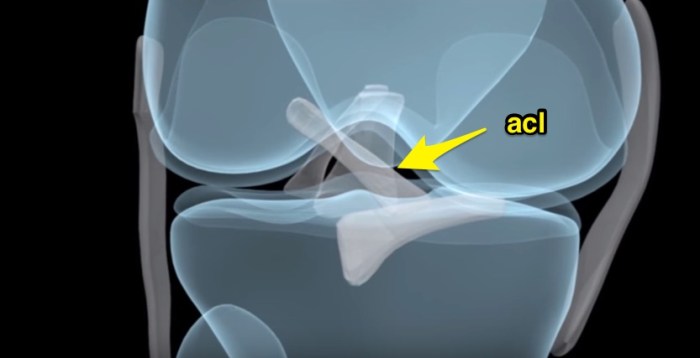
Anterior cruciate ligament (ACL) tears are a common injury, particularly in athletes. Surgical repair, often involving ACL reconstruction, aims to restore stability and function. Common procedures include using hamstring or patellar tendon grafts. This detailed look at ACL tears after surgery provides a clear picture of the entire process, from initial surgery to long-term outcomes.
Introduction to ACL Tears After Surgery

An anterior cruciate ligament (ACL) tear is a common injury, particularly among athletes. ACL tears often require surgical repair, usually involving reconstruction. This surgical process aims to restore stability to the knee joint, allowing for a return to normal activities. The recovery process after surgery is crucial for successful rehabilitation and long-term joint health.Surgical reconstruction aims to replace the torn ligament with a graft, typically taken from another part of the body, like the hamstring or patellar tendon.
The choice of graft depends on individual factors and the surgeon’s preference. Post-operative rehabilitation plays a significant role in regaining strength, flexibility, and range of motion.
Surgical Procedures for ACL Reconstruction
Various surgical techniques are employed in ACL reconstruction. These procedures involve replacing the torn ACL with a substitute ligament, often from a patient’s own body tissue. The primary goal is to restore the knee’s stability and functionality.
Common Graft Types
The choice of graft material significantly impacts the recovery process. Understanding the different graft types is crucial for patients to make informed decisions about their treatment.
| Graft Type | Source | Advantages | Disadvantages |
|---|---|---|---|
| Hamstring Grafts | Hamstring tendons | Generally easier to harvest, less invasive | Potential for hamstring weakness if not carefully handled |
| Patellar Tendon Grafts | Patellar tendon | Strong graft, often associated with faster recovery | Potential for patellar tendonitis or pain in the patella region |
| Quadriceps Tendon Grafts | Quadriceps tendon | Excellent strength, potentially faster recovery | More invasive harvesting, potential for quadriceps weakness |
Typical Recovery Timeline
The recovery timeline following ACL reconstruction surgery is variable, depending on several factors. These include the patient’s age, activity level, and adherence to the rehabilitation protocol. A realistic understanding of the recovery process is essential for patient management.A typical recovery timeline might involve several phases:
- Initial Phase (Weeks 1-4): Focus on pain management, controlled range of motion exercises, and early mobilization. Patients will likely use crutches or other assistive devices during this phase. Examples include controlled knee flexion and extension exercises, as well as light range of motion exercises. This phase prioritizes minimizing swelling and protecting the healing graft.
- Intermediate Phase (Weeks 4-12): Gradually increase the intensity and range of motion exercises. Begin strengthening exercises for the surrounding muscles. The goal is to restore the knee’s stability and functionality. Examples include progressively increasing resistance during strengthening exercises and the introduction of sport-specific exercises.
- Advanced Phase (Weeks 12-24+): Return to normal activities, including sports, is a gradual process. Continued strengthening and proprioception exercises are vital for preventing re-injury. This phase may include more complex agility and balance training. Examples include progressing from simple to more complex movements, such as running, jumping, and agility drills, while gradually increasing intensity and duration.
Potential Complications: Acl Tears After Surgery
While ACL reconstruction surgery is a highly effective procedure, potential complications can arise. These complications range from relatively minor issues to more serious problems that may impact long-term recovery and function. Understanding the potential complications and their likelihood is crucial for both patients and surgeons to make informed decisions. Careful planning and meticulous surgical technique can minimize the risk of these complications.Post-operative complications are a multifaceted concern, influenced by individual patient factors, surgical technique, and post-operative care.
The likelihood of specific complications varies, and factors like age, overall health, and adherence to post-operative instructions can significantly impact the outcome.
Recovering from an ACL tear after surgery is tough, but fueling your body with the right foods is key to healing. Focus on nutrient-rich options like lean protein and complex carbohydrates to support your body’s repair process. Eating a balanced diet, like those found in foods that give you energy , will give you the energy you need for physical therapy and daily activities.
This will ultimately help you regain strength and get back to your active lifestyle faster. A good diet is essential for successful ACL recovery.
Infection
Infection is a serious complication following any surgical procedure, and ACL reconstruction is no exception. Bacterial infections can lead to significant tissue damage, potentially requiring additional surgeries and prolonged recovery periods.
- Causes of infection often stem from contamination during surgery, poor wound care, or underlying health conditions that compromise the immune system. Surgical site infections (SSIs) can result from inadequate sterilization procedures or the introduction of bacteria during the procedure.
- The likelihood of infection is generally low, but factors like the presence of pre-existing infections, or a compromised immune system increase the risk. This is why thorough pre-operative assessments and meticulous surgical technique are essential.
Stiffness
Post-operative stiffness is a common concern, potentially limiting the range of motion in the knee joint. This can result from various factors, including scar tissue formation, inflammation, or inadequate rehabilitation.
- Early and aggressive physiotherapy plays a vital role in minimizing stiffness. Consistent exercises and gentle stretching routines, guided by a physical therapist, help maintain joint flexibility and prevent the development of adhesions and contractures.
- In some cases, stiffness can persist despite diligent rehabilitation. In such situations, specific treatment modalities like joint injections or manipulation might be considered to improve mobility.
Delayed Healing
Delayed healing encompasses a spectrum of issues, from slow wound closure to persistent pain and delayed return to activity. Several factors can contribute to delayed healing.
- Factors such as poor blood supply to the surgical area, inadequate nutrition, or pre-existing medical conditions can hinder the body’s natural healing processes.
- The healing process varies significantly from person to person. Some individuals heal faster than others, while others may experience prolonged recovery times.
Failure of Graft
Failure of the graft refers to the ACL graft not properly integrating with the surrounding tissues or not functioning as intended, which can lead to knee instability. This is a more serious complication.
- Factors such as improper graft selection, poor surgical technique, or patient factors (e.g., high activity levels) can potentially contribute to graft failure. Understanding patient activity level and expectations is crucial in determining the right surgical approach.
- The likelihood of graft failure is lower when the surgical procedure is performed correctly, and the patient actively participates in the rehabilitation process.
Other Complications, Acl tears after surgery
Other potential complications include: nerve damage, blood clots, and loosening of the hardware used in the procedure.
| Complication | Signs and Symptoms |
|---|---|
| Nerve Damage | Numbness, tingling, or pain along the nerve pathway. |
| Blood Clots | Swelling, pain, warmth, or redness in the affected limb. |
| Hardware Loosening | Pain, clicking, or catching sensations in the knee. |
Post-Surgical Rehabilitation
Recovering from ACL reconstruction surgery requires a structured and diligent approach to rehabilitation. This phase isn’t just about regaining range of motion; it’s about building strength, restoring stability, and ultimately, returning to your pre-injury activity level. The process is progressive, requiring careful monitoring and adherence to a personalized plan. Success depends heavily on patient commitment and the guidance of a qualified physical therapist.The post-surgical rehabilitation program is designed to address the specific needs of each patient.
It carefully progresses through distinct phases, gradually increasing the intensity and complexity of exercises. Understanding the different phases and their associated exercises is crucial for successful recovery. This knowledge empowers patients to actively participate in their rehabilitation journey and accelerate their return to normal activities.
Phases of Post-Surgical Rehabilitation
The rehabilitation process following ACL reconstruction is typically divided into several distinct phases. Each phase builds upon the previous one, gradually increasing the demands placed on the knee and surrounding tissues. A crucial aspect of these phases is the gradual introduction of controlled stress to facilitate healing and prevent re-injury.
Phase 1: Early Recovery (First 4-6 Weeks)
This initial phase focuses on protecting the healing graft and minimizing swelling. The primary goals are pain management, regaining a full range of motion, and beginning the process of regaining strength and stability. Activities are carefully monitored to ensure the healing tissues are not stressed beyond their capacity.
- Protecting the healing graft: Activities are designed to prevent excessive stress on the repaired ligament. This often involves using crutches, knee braces, and limited weight-bearing. Emphasis is placed on avoiding activities that could jeopardize the healing process.
- Range of motion exercises: Gentle exercises are performed to maintain the range of motion of the knee joint. These exercises include passive range of motion (assisted by a therapist or another person) and active assisted range of motion (with some assistance from the patient). Simple exercises like knee flexion and extension are typically performed.
- Gentle strengthening exercises: Initial strengthening exercises are focused on the quadriceps muscle, targeting the front of the thigh. These exercises may include isometric quad sets (squeezing the quadriceps muscle without moving the knee) and gentle hamstring exercises.
Phase 2: Strengthening and Proprioception (6-12 Weeks)
This phase gradually increases the intensity of exercises, focusing on improving muscle strength, balance, and proprioception (the body’s awareness of its position in space). The focus shifts towards controlled movements that gradually challenge the healing tissue while also promoting stability and coordination.
- Progressive strengthening exercises: Exercises are progressively loaded to enhance quadriceps and hamstring strength. These include exercises like straight leg raises, and more advanced hamstring exercises, ensuring the exercises don’t compromise the healing process.
- Proprioceptive exercises: These exercises help improve the knee’s ability to sense its position and movement. Examples include balance exercises on unstable surfaces, such as wobble boards or foam pads, and exercises that challenge the knee’s coordination.
- Cardiovascular exercises: Low-impact cardio, such as stationary cycling and swimming, are introduced to gradually improve cardiovascular fitness.
Phase 3: Functional Training (12-24 Weeks)
This phase prepares the patient for a return to sport or other activities. The focus is on functional movements that mimic activities of daily living and sports-specific movements. The aim is to fully integrate the knee into normal movement patterns.
- Functional exercises: Exercises are designed to mimic activities like stair climbing, squatting, and running. These exercises are progressively introduced to ensure the knee can handle the stresses associated with these movements.
- Sport-specific training: If applicable, specific exercises for the patient’s sport are introduced. This may involve agility drills, plyometrics (exercises that involve jumping and explosive movements), and other sport-specific activities, all under careful supervision.
- Return to sport progression: A gradual return to sports activities is carefully monitored. This often involves a progression of drills and activities that gradually increase the demands on the knee joint.
Progression of Exercises Across Rehabilitation Phases
| Phase | Exercises |
|---|---|
| Phase 1 | Isometric quad sets, passive range of motion, gentle hamstring exercises |
| Phase 2 | Straight leg raises, hamstring curls, balance exercises, low-impact cardio |
| Phase 3 | Functional exercises, sport-specific training, plyometrics, return to sport progression |
Importance of Adherence to the Rehabilitation Program
Adherence to the rehabilitation program is paramount for successful recovery and a full return to activity. A commitment to the prescribed exercises and activities is crucial for ensuring the healing process progresses as expected. A dedicated effort is necessary to maximize the benefits of the rehabilitation plan.
Factors Affecting Recovery
The road to recovery after ACL surgery is a journey unique to each individual. While the surgical procedure itself is a significant step, the factors influencing the healing process are just as crucial. Understanding these variables allows for a more personalized approach to rehabilitation, maximizing the chances of a successful outcome.Factors like age, activity level, and pre-existing conditions play pivotal roles in determining the length and nature of the recovery period.
Recovering from an ACL tear surgery can be a long haul, and while physical therapy is key, some unexpected symptoms can pop up. One common complaint is tinnitus, or ringing in the ears. Understanding the potential causes and treatments for this symptom is crucial for a smooth recovery. For a deeper dive into the causes, symptoms, and available treatments for tinnitus, check out this helpful resource on ringing in ears symptoms causes and treatment.
Ultimately, addressing these unexpected symptoms alongside the standard physical therapy will help you get back on your feet faster after your ACL surgery.
Furthermore, adherence to the rehabilitation plan and overall lifestyle choices greatly impact the final results.
Age and Recovery
Age significantly influences the body’s natural healing capacity. Younger individuals often experience faster tissue regeneration and quicker recovery times compared to older adults. This is due to the inherent differences in cellular turnover and tissue repair mechanisms. While age isn’t a barrier to successful recovery, it often necessitates a more cautious and potentially longer rehabilitation protocol. For instance, an older athlete might require a more gradual progression of exercises to avoid undue stress on the healing tissues.
The emphasis shifts towards maintaining joint function and mobility while minimizing the risk of complications.
Activity Level and Recovery
An individual’s pre-injury activity level plays a critical role in the recovery process. Professional athletes, for example, will need a more intensive rehabilitation program to regain the high level of strength and endurance required for their sport. Their rehabilitation will likely involve more specialized exercises and a more rigorous schedule compared to someone with a less demanding lifestyle.
The focus will be on not only regaining the lost function but also surpassing it to reach their previous performance level. Conversely, individuals with lower pre-injury activity levels will have a more manageable recovery trajectory, with a focus on building a solid foundation of strength and mobility before progressing to more complex movements.
Pre-Existing Conditions and Recovery
Pre-existing conditions can also influence the recovery process. Conditions like diabetes, obesity, or cardiovascular issues can affect the body’s overall healing response. These conditions may necessitate modifications to the rehabilitation program to address any potential complications or limitations. For instance, someone with diabetes might require more careful monitoring of blood sugar levels during the rehabilitation phase to prevent complications.
The rehabilitation plan will be customized to accommodate the individual’s specific health needs and limitations.
Optimizing Recovery for Specific Characteristics
Individuals with specific characteristics can benefit from tailored rehabilitation strategies. For instance, athletes can incorporate sport-specific exercises into their rehabilitation plan to ensure they can return to their pre-injury performance levels. This personalized approach allows for a more efficient recovery and a quicker return to the activity they love. Similarly, individuals with pre-existing conditions can work with their physical therapists to adjust the program based on their individual needs and limitations.
Different Rehabilitation Approaches
Various rehabilitation approaches can be employed to address individual needs. A structured program combining physical therapy, strength training, and potentially bracing or supportive devices, might be beneficial. The rehabilitation plan should consider factors like the individual’s pain tolerance, activity level, and overall health status. For example, a progressive resistance program designed by a physical therapist can help build strength and improve joint stability, gradually increasing the intensity and complexity of exercises as the individual progresses.
Furthermore, incorporating lifestyle modifications, such as nutrition and sleep, can further support the healing process and optimize the recovery journey.
Long-Term Outcomes
ACL reconstruction surgery aims to restore knee stability and function. However, the journey to long-term success isn’t always straightforward. Understanding the potential outcomes, both positive and challenging, is crucial for patients and their healthcare providers. Factors influencing the long-term results range from the surgical technique itself to the patient’s adherence to rehabilitation protocols.Successful ACL reconstruction, while common, isn’t a guaranteed outcome.
Recovering from an ACL tear after surgery can be a long journey, and sometimes you might notice a lump under the skin. This is a common concern, and understanding the potential causes and when to seek medical attention is crucial. Knowing that a lump could be a normal part of the healing process or a sign of a complication is important.
Checking out resources like lump under skin causes and when to worry can help you differentiate between the two. Ultimately, consistent communication with your doctor about any changes is key to a successful ACL recovery.
Post-operative complications and individual factors can influence the long-term functionality of the reconstructed ligament. This section explores the key elements that contribute to successful long-term results and addresses potential challenges.
Success Rates of ACL Reconstruction
Success rates for ACL reconstruction vary depending on several factors, including the surgeon’s experience, the patient’s age, activity level, and adherence to rehabilitation. Studies have shown that the procedure can achieve high success rates, typically exceeding 80% in many cases. However, factors such as graft choice, surgical technique, and patient compliance play a significant role. These results are often measured by return to pre-injury activity levels and the absence of significant pain or instability.
Factors Contributing to Successful Long-Term Outcomes
Numerous factors influence the long-term success of ACL reconstruction. Patient compliance with rehabilitation protocols is paramount. A comprehensive rehabilitation program, including exercises to strengthen supporting muscles, improve range of motion, and regain balance, is crucial. Furthermore, a patient’s overall health, age, and activity level significantly impact recovery. Younger patients generally have better long-term outcomes compared to older patients.
The choice of graft type also plays a role; different grafts (autografts, allografts) might exhibit varying degrees of integration and durability.
Potential for Re-injury
Re-injury after ACL reconstruction is a possibility, although not a certainty. Factors that increase the risk of re-injury include inadequate rehabilitation, a return to high-impact activities too soon, and a lack of proper conditioning. The severity and type of pre-injury activity and the individual’s inherent predisposition to injury also influence the likelihood of re-injury. For instance, athletes participating in contact sports often face a higher risk of re-injury than those involved in non-contact activities.
Comparison of Surgical Techniques
Different surgical techniques for ACL reconstruction exist, each with its own advantages and disadvantages. Arthroscopic techniques are commonly used and involve minimally invasive procedures. These procedures often lead to quicker recovery times and less scarring compared to open procedures. However, the long-term outcomes of various techniques can differ based on the specific details of the surgery and the patient’s individual response.
Studies examining long-term outcomes of different techniques often consider factors such as graft survival, stability, and the ability to return to previous activity levels.
Long-Term Functional Outcomes
Long-term functional outcomes following ACL reconstruction vary. Some patients experience a complete return to pre-injury activity levels, while others may experience limitations in specific activities. The success of the surgery depends on several factors, including the severity of the initial injury, the patient’s compliance with rehabilitation, and the surgical technique employed. A patient’s age, activity level, and overall health are also critical factors influencing long-term functional outcomes.
Patient Experiences and Perspectives
The journey of recovering from an ACL tear and reconstruction is profoundly personal. Beyond the physical rehabilitation, patients face a complex emotional and psychological landscape. Understanding these experiences is crucial for providing comprehensive care and support. This section delves into the diverse perspectives and challenges encountered by individuals navigating this process.
Patient Experiences: A Summary
Patient experiences following ACL reconstruction are varied, influenced by factors such as pre-injury activity levels, personality, support systems, and the surgical technique. There are common threads, however, of both triumph and struggle. The following table summarizes some key experiences.
| Aspect | Common Experience |
|---|---|
| Physical Pain and Discomfort | Patients commonly report varying degrees of pain and discomfort during the rehabilitation process, especially during the initial stages. The intensity and duration of this pain can differ significantly based on individual factors. |
| Psychological Impact | Anxiety, frustration, and depression are not uncommon, especially during periods of plateau in progress. Fear of re-injury or concerns about long-term functionality can contribute to emotional distress. |
| Social Adjustment | Changes in daily routines and social activities can lead to feelings of isolation or frustration. Adjustments to limitations and the recovery process can impact relationships with friends and family. |
| Emotional Well-being | Maintaining a positive attitude and managing emotional challenges are crucial aspects of the recovery process. Patients may experience emotional ups and downs, but support systems can significantly influence their journey. |
| Motivation and Perseverance | Maintaining motivation throughout the recovery period is a significant challenge. Progress can be slow, and setbacks are common. Patients need to understand the importance of consistent effort and perseverance. |
Successful Recovery Stories
Numerous patients have achieved successful recoveries following ACL reconstruction. These stories often highlight the importance of a dedicated rehabilitation program, strong support networks, and a positive attitude. One example is a high school athlete who, through diligent physical therapy and a supportive family, regained full range of motion and athletic abilities. They were able to return to their sport at a high level and continue playing for many years.
Less Successful Recovery Stories
Unfortunately, some patients experience less successful recoveries. Factors like inadequate adherence to rehabilitation protocols, pre-existing conditions, or psychological challenges can hinder progress. One example involves a patient who struggled with motivation and adherence to the prescribed rehabilitation exercises. This led to delayed recovery, potential complications, and a prolonged recovery time. This emphasizes the importance of patient engagement and consistent follow-up.
Psychological Impact of Injury and Surgery
ACL injuries and subsequent surgeries can significantly impact a patient’s psychological well-being. The fear of re-injury, concerns about future athletic participation, and the physical and emotional demands of rehabilitation can lead to anxiety, depression, and feelings of isolation. Addressing these psychological aspects is crucial for optimal recovery. For example, cognitive behavioral therapy (CBT) can help patients manage their thoughts and feelings related to the injury.
Emotional Journey During Recovery
The emotional journey of a patient recovering from an ACL injury and surgery is multifaceted and often unpredictable. Patients may experience a range of emotions, from initial shock and disappointment to frustration and anger during setbacks, and finally, joy and satisfaction as they progress toward recovery. Acknowledging and addressing these emotions is essential for a smoother recovery process.
It’s important for patients to allow themselves to feel the full spectrum of emotions and seek support when needed.
Surgical Techniques & Procedures
Choosing the right surgical technique for ACL reconstruction is crucial for a successful recovery. Different methods cater to individual patient needs and preferences, while also considering the surgeon’s expertise and the specific characteristics of the injury. Understanding these options empowers patients to make informed decisions with their healthcare providers.
Different Surgical Techniques
Various surgical techniques exist for ACL reconstruction, each with its own set of advantages and disadvantages. These techniques primarily differ in the approach to graft harvesting and placement. Open procedures, while once common, are now less frequently used due to the greater precision and reduced invasiveness offered by arthroscopic techniques. Arthroscopic surgery uses small incisions and specialized instruments, allowing for a less disruptive procedure.
Arthroscopic ACL Reconstruction
Arthroscopic ACL reconstruction is the most common surgical technique. It involves minimally invasive incisions, typically 2-3 small portals. Surgeons use specialized instruments to visualize and repair the damaged ligament. This approach generally results in less pain, quicker recovery, and smaller scars. It is also less disruptive to surrounding tissues.
Graft Types and Their Advantages/Disadvantages
The choice of graft material significantly influences the recovery process and long-term outcomes. The most common grafts are derived from the patient’s own body tissues, including hamstring tendons and patellar tendons. Other options include allograft tissues (from a donor).
Comparison of Graft Types
| Graft Type | Source | Advantages | Disadvantages |
|---|---|---|---|
| Hamstring Tendon | Patient’s hamstring muscle | Generally quicker recovery, less risk of patellar tendonitis, lower risk of anterior knee pain. | Potential for hamstring weakness, slightly higher risk of graft rupture in the first year. |
| Patellar Tendon | Patient’s patellar tendon | Stronger graft, potentially better long-term stability, less risk of hamstring weakness. | Potential for anterior knee pain, potential for patellar tendonitis, slightly longer recovery time. |
| Allograft | Donor tissue | May be useful in cases where autograft is not ideal. | Risk of rejection, potential for disease transmission if not properly screened and treated, more expensive. |
Impact on Recovery
The specific surgical technique and the chosen graft type directly impact the recovery period. For example, arthroscopic surgery with a hamstring tendon graft might lead to a faster return to activities compared to an open procedure with a patellar tendon graft. Individual patient factors like age, activity level, and overall health play a crucial role in determining the best approach.
This individualized approach ensures the optimal balance between speed of recovery and long-term stability.
Factors Influencing Surgical Technique Selection
Several factors influence the surgeon’s decision regarding the surgical technique and graft choice. These factors include the severity of the tear, the patient’s age, activity level, and overall health. The surgeon’s experience and preferences also play a significant role. Open procedures are less common, but still an option for complex injuries. The primary goal is to select the procedure that provides the best chance for a successful and complete recovery.
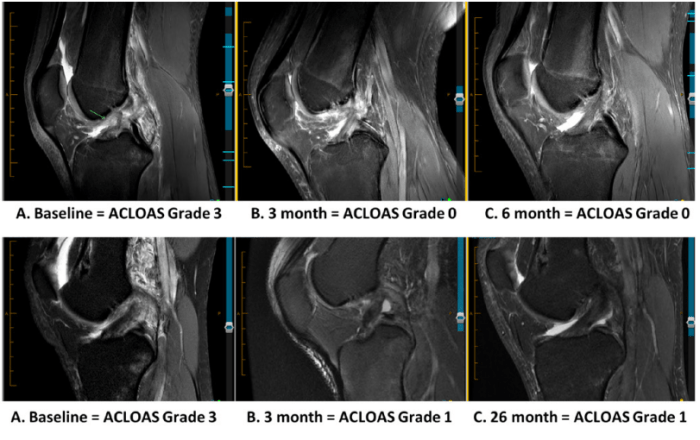
Monitoring and Evaluation
Post-operative monitoring and evaluation are crucial for ensuring successful ACL reconstruction and minimizing complications. These procedures help track the healing process, identify potential issues early, and adjust the rehabilitation plan as needed. Regular assessments allow healthcare providers to gauge the patient’s progress, ensuring they’re on track to achieve optimal outcomes.
Methods for Monitoring Healing
Regular check-ups and physical assessments are fundamental in monitoring the healing process after ACL reconstruction. These assessments help evaluate the extent of tissue integration, joint stability, and overall function. A combination of clinical examinations, imaging studies, and functional tests provide a comprehensive picture of the patient’s progress. These methods enable healthcare professionals to adapt the rehabilitation program based on the patient’s individual needs and response to treatment.
Importance of Regular Check-ups
Regular check-ups are essential to assess the healing process and identify potential problems early. They provide a platform to evaluate the patient’s progress and ensure adherence to the prescribed rehabilitation plan. Prompt detection of complications, such as infection or persistent swelling, can lead to timely interventions, minimizing the risk of long-term complications. Early intervention is critical to maximizing the chances of a successful recovery.
Diagnostic Tools for Monitoring Progress
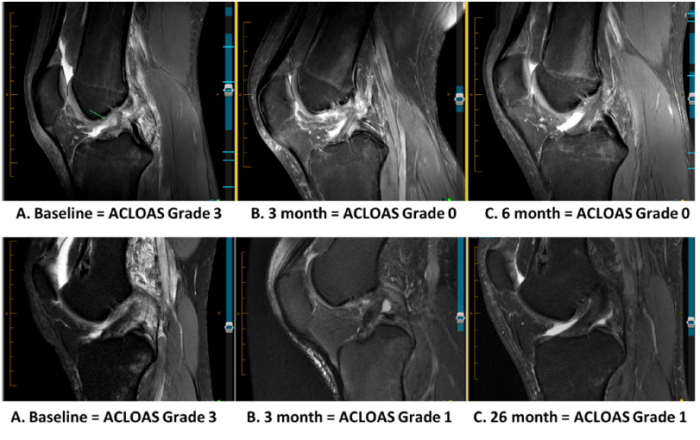
Various diagnostic tools are employed to monitor the healing process. These tools include physical examinations, which assess range of motion, strength, and stability of the knee joint. Radiographic imaging, such as X-rays and MRI scans, provides detailed images of the bone and soft tissues, allowing visualization of the graft integration and potential complications. Functional tests, like the Lachman test and anterior drawer test, are used to evaluate the stability of the ACL reconstruction.
These tests are vital in assessing the effectiveness of the surgery and the patient’s ability to perform daily activities.
Post-Operative Imaging Techniques
A crucial aspect of monitoring the healing process is employing appropriate imaging techniques. These techniques provide valuable insights into the status of the reconstructed ACL, the surrounding tissues, and the overall healing process. Early detection of complications or delayed healing is possible through these methods. Accurate imaging guides decisions about rehabilitation progression and surgical interventions if needed.
| Imaging Technique | Description | Use in ACL Monitoring |
|---|---|---|
| X-ray | Two-dimensional radiographic image of bones. | Evaluates bone alignment, assesses for fracture, or signs of loosening. |
| MRI (Magnetic Resonance Imaging) | Three-dimensional detailed image of soft tissues. | Visualizes the ACL graft, surrounding ligaments, cartilage, and tendons. Identifies any signs of inflammation, swelling, or graft tears. |
| CT (Computed Tomography) | Three-dimensional image of the bones and soft tissues. | Provides detailed anatomical information about bone structures and can evaluate the graft integration with the bone. |
| US (Ultrasound) | Real-time image of soft tissues using sound waves. | Assess for soft tissue swelling, inflammation, and evaluate the healing process in the early stages post-surgery. |
Addressing Specific Concerns
Navigating the journey after ACL reconstruction surgery can be filled with anxieties and uncertainties. This section focuses on common concerns and provides practical strategies to address them, helping you feel more empowered and prepared for the road ahead. From pain management to returning to your favorite activities, we’ll explore actionable solutions.
Pain Management Strategies
Managing post-operative pain is crucial for a smooth recovery. A multi-faceted approach, incorporating medication, physical therapy techniques, and lifestyle adjustments, is essential.
- Medication adherence is vital. Follow your physician’s instructions precisely regarding dosage and timing of pain relievers. Over-the-counter options like ibuprofen can help manage mild to moderate discomfort. Prescription medication, such as opioids, may be necessary for more severe pain, but use these medications only as directed by your physician and be aware of potential side effects.
Discuss alternative pain management options with your healthcare team if needed.
- Ice packs and compression are beneficial for reducing swelling and pain. Applying ice for 15-20 minutes at a time, several times a day, can help minimize discomfort. Proper compression helps to control swelling and support the healing tissues.
- Physical therapy techniques like gentle range-of-motion exercises and manual therapy can aid in pain management. These methods, guided by a qualified physical therapist, promote healing and reduce stiffness.
Return to Sports
Returning to sports after ACL reconstruction is a significant goal for many patients. A gradual and well-structured approach, emphasizing functional strength and stability, is key to successful return.
- A phased return-to-sport protocol, designed by your physical therapist, is critical. This program gradually increases the intensity and complexity of activities, ensuring that the knee is adequately prepared for the demands of the sport. Each phase should be completed before progressing to the next, to avoid potential setbacks or reinjury.
- Strength training is essential to improve knee stability and muscle strength around the joint. Exercises should be tailored to your specific needs and progress gradually. Focus on building strength in the quadriceps, hamstrings, and surrounding muscles to support the knee joint. Progressive resistance exercises are essential to ensure that you do not overload the tissues.
- Proper warm-up and cool-down routines are essential before and after physical activity. These routines prepare the muscles and tissues for activity and help prevent injury.
Potential Limitations
ACL reconstruction surgery does not guarantee a complete return to your pre-injury activity level. Patients need to acknowledge potential limitations and adjust their expectations accordingly.
- Some activities might require modifications or adjustments. For instance, high-impact activities might need to be avoided or modified to reduce stress on the reconstructed ligament.
- Gradual return to activities is essential. Jumping, pivoting, and other demanding movements should be reintroduced gradually to minimize the risk of re-injury. Listen to your body, and adjust your activities accordingly.
- Long-term monitoring and follow-up care are crucial. Regular check-ups with your orthopedic surgeon are essential to ensure that the healing process is progressing as expected and to address any potential complications.
Common Patient Concerns & Responses
| Common Question | Appropriate Response |
|---|---|
| How long will it take to fully recover? | Recovery time varies depending on the individual, but a typical timeline is several months. Factors like age, activity level, and adherence to the rehabilitation program influence recovery. |
| Will I be able to return to my previous activity level? | While a full return is often possible, it’s essential to understand that there might be limitations. A phased return-to-sport program, designed in consultation with your healthcare team, is crucial. |
| How can I manage the pain effectively? | Pain management strategies often involve a combination of medication, ice packs, compression, physical therapy, and lifestyle adjustments. Always follow your physician’s instructions. |
Addressing Rehabilitation Challenges
Specific challenges in rehabilitation can be addressed through individualized strategies.
- Motivation and adherence to the rehabilitation program are crucial. Setting realistic goals, celebrating milestones, and maintaining a positive attitude can enhance motivation. Consider seeking support from family and friends or support groups.
- Managing pain and swelling is critical during rehabilitation. Proper techniques, like icing, compression, and elevation, can help manage discomfort and facilitate the healing process. Discuss pain management options with your healthcare team.
- Overcoming psychological barriers like fear of re-injury or anxiety about returning to sports can be addressed with a supportive environment and open communication with your healthcare team.
End of Discussion
In conclusion, navigating the path of ACL tears after surgery demands a comprehensive approach, encompassing surgical techniques, potential complications, and personalized rehabilitation plans. Factors like age, activity level, and pre-existing conditions significantly impact recovery. A strong support system, adherence to the rehabilitation program, and open communication with healthcare professionals are vital for achieving optimal long-term outcomes. This guide aims to equip you with the knowledge and insights necessary for a successful recovery.