Fibromyalgia primary or secondary is a complex condition that often stumps doctors and patients alike. Understanding the distinctions between primary and secondary forms is crucial for proper diagnosis and effective management. This exploration delves into the characteristics, causes, and treatment approaches for both, offering a comprehensive guide for anyone affected by or seeking to understand this pervasive illness.
This article will cover the definition of fibromyalgia, including its diagnostic criteria and comparison to other conditions. We will delve into the origins and contributing factors of primary fibromyalgia, contrasting them with the secondary form, which often arises from other underlying health issues. We will explore the diagnostic process, differentiating the symptoms and approaches for each type. Further, we will Artikel management strategies tailored to both primary and secondary forms, emphasizing the crucial role of interdisciplinary care.
Illustrative case studies will solidify the discussion and highlight the complexity of diagnosis.
Defining Fibromyalgia
Fibromyalgia is a chronic condition characterized by widespread musculoskeletal pain, fatigue, and a range of other symptoms. Understanding its intricacies is crucial for effective diagnosis and management. This chronic pain syndrome impacts daily life significantly, demanding a comprehensive approach to care.Fibromyalgia is a complex disorder that involves widespread pain, accompanied by various symptoms impacting a person’s overall well-being.
Figuring out if your fibromyalgia is primary or secondary can be tricky. It’s a bit like choosing the right doctor for your asthma – you need someone who understands the nuances and complexities of your specific condition. Finding the right specialist, like a pulmonologist for types of asthma doctors and choosing the best one , is key to getting the right diagnosis and treatment plan.
Ultimately, pinpointing whether your fibromyalgia is primary or secondary is crucial for developing an effective treatment strategy. It’s a personal journey, so don’t hesitate to seek out expert opinions.
It’s not just about the pain; it encompasses a constellation of issues affecting sleep, mood, and cognitive function. The exact cause of fibromyalgia remains elusive, but research suggests a combination of genetic predisposition, environmental factors, and psychological elements play a role.
Characteristics of Fibromyalgia
Fibromyalgia is defined by its pervasive pain and accompanying symptoms. The pain is often described as a deep, aching sensation, affecting multiple areas of the body simultaneously. Fatigue is a common and significant symptom, often impacting energy levels and daily activities. Sleep disturbances are frequently reported, with difficulty falling asleep, staying asleep, or experiencing restorative sleep.
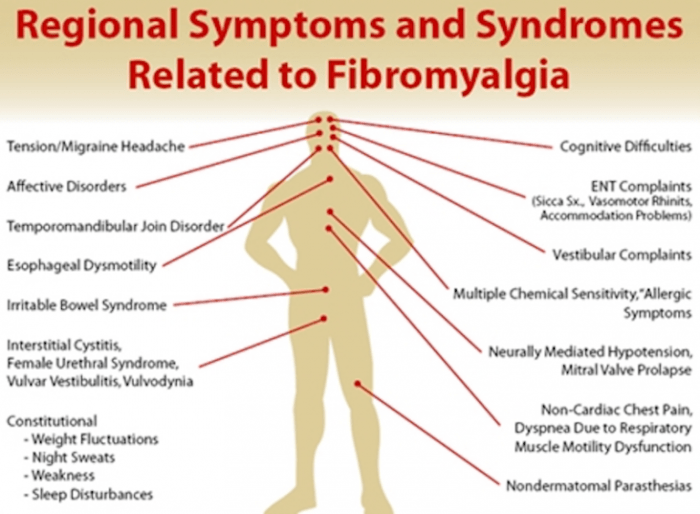
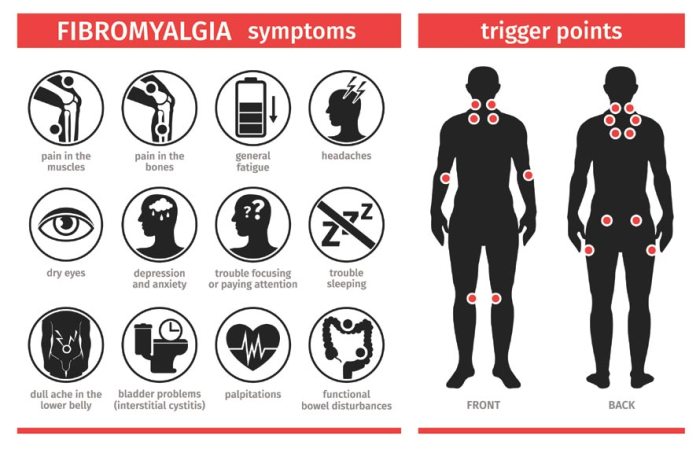
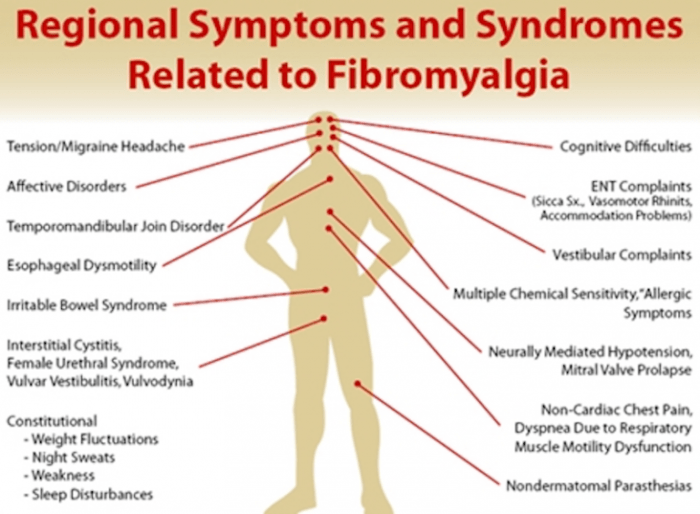
Symptoms of Fibromyalgia
The symptoms of fibromyalgia extend beyond pain and fatigue. Cognitive difficulties, such as trouble concentrating or memory problems, are common complaints. Emotional distress, including anxiety and depression, frequently accompanies the condition. Other symptoms include headaches, irritable bowel syndrome, and sleep disturbances.
Diagnostic Criteria for Fibromyalgia
The diagnosis of fibromyalgia relies on a combination of clinical evaluation and symptom assessment. The American College of Rheumatology (ACR) criteria are commonly used. These criteria include widespread pain, pain lasting for at least three months, and the presence of tender points. These tender points are specific areas on the body where pressure elicits pain.
Comparison with Other Conditions
| Feature | Fibromyalgia | Rheumatoid Arthritis | Osteoarthritis ||—|—|—|—|| Pain | Widespread, deep aching | Joint pain, symmetrical | Joint pain, localized, progressive || Inflammation | Low to absent | High | Low to moderate || Tender Points | Present | Absent | Absent || Fatigue | Often severe | Variable | Variable || Sleep | Disrupted | Variable | Variable || Cognitive Issues | Common | Variable | Variable |
This table highlights key distinctions between fibromyalgia and other conditions.
The presence or absence of inflammation, tender points, and specific pain patterns can aid in differentiation. Consulting with a healthcare professional is essential for accurate diagnosis and tailored treatment plans.
Diagnostic Process Flowchart
(A visual flowchart would be best presented graphically. Here is a textual representation instead.) Patient presents with symptoms (e.g., widespread pain, fatigue, sleep disturbances).→ Healthcare professional assesses patient history and performs a physical examination.→ Questions about the duration, intensity, and location of pain are asked.→ Examination for tender points according to the ACR criteria.→ Evaluation of other symptoms (fatigue, sleep, cognitive issues).→ Rule out other potential conditions (e.g., rheumatoid arthritis, lupus).→ If criteria for fibromyalgia are met, a diagnosis of fibromyalgia is made.→ Patient is provided with appropriate management strategies and referrals (e.g., physical therapy, counseling).
This flowchart illustrates a general diagnostic process. The exact steps and evaluations may vary depending on the individual case and healthcare provider’s approach.
Primary Fibromyalgia
Primary fibromyalgia, a perplexing condition, remains a mystery in many ways. While the exact causes are still being investigated, researchers are uncovering potential factors that may play a role in its development. This form of fibromyalgia is not triggered by another underlying medical condition, as is the case with secondary fibromyalgia. Instead, it is believed to originate from intrinsic factors within the individual.Primary fibromyalgia is characterized by widespread pain, fatigue, and a constellation of other symptoms.
The origins of this condition are often attributed to a complex interplay of genetic predispositions and environmental influences. Understanding these contributing factors can pave the way for improved diagnostic and therapeutic approaches.
Potential Origins of Primary Fibromyalgia
The exact origins of primary fibromyalgia remain elusive. Several hypotheses propose potential pathways for its development, highlighting the complexity of the condition. These hypotheses suggest that primary fibromyalgia isn’t simply a single cause but rather an amalgamation of factors interacting in intricate ways.
Figuring out if your fibromyalgia is primary or secondary can be tricky, right? While exploring natural remedies for pain management, I’ve been researching different approaches, and stumbled upon some interesting natural treatments for endometriosis. Natural treatments for endometriosis are definitely worth looking into for anyone experiencing chronic pain, and it’s a good starting point to help identify possible underlying factors, which could help to understand the roots of fibromyalgia.
Ultimately, determining whether fibromyalgia is primary or secondary requires a thorough assessment with your doctor, so don’t self-diagnose!
Contributing Factors to Primary Fibromyalgia
Several factors are believed to contribute to the development of primary fibromyalgia. These factors may act individually or in combination to increase susceptibility to the condition.
- Genetic Predisposition: A family history of fibromyalgia or other chronic pain conditions can increase the risk of developing primary fibromyalgia. This suggests a potential genetic component, though the specific genes involved remain to be fully elucidated. Individuals with a family history of mood disorders, anxiety, or other chronic conditions might be at a higher risk as well.
This correlation needs further investigation.
- Environmental Factors: Exposure to certain environmental stressors, such as infections, trauma, or significant life events, may play a role in triggering or exacerbating primary fibromyalgia. Stressful events, such as the death of a loved one or a major accident, might trigger or worsen existing pain and symptoms. The precise nature of this relationship remains unclear.
- Neurobiological Factors: Impairments in the central nervous system’s processing of pain signals might be a key element in primary fibromyalgia. This includes abnormal functioning of neurotransmitters and altered brain activity patterns. These dysfunctions can lead to a heightened sensitivity to pain and a more pronounced response to otherwise benign stimuli.
Prevalence of Primary vs. Secondary Fibromyalgia
The prevalence of primary fibromyalgia compared to secondary fibromyalgia is a topic of ongoing research. Estimates vary, and more studies are needed to clarify the exact prevalence of each form. However, primary fibromyalgia is believed to be more prevalent than secondary fibromyalgia in certain patient populations, particularly in those without any other identifiable underlying conditions. This difference in prevalence needs further study to understand its true extent.
Genetic and Environmental Factors
Genetic and environmental factors are suspected to play a crucial role in primary fibromyalgia. The interplay of these factors is believed to influence an individual’s susceptibility to the condition. However, the precise mechanisms through which these factors interact remain to be fully understood. Further research is needed to uncover the specific genes and environmental triggers that contribute to the development of primary fibromyalgia.
Theories Regarding the Cause of Primary Fibromyalgia
| Theory | Description |
|---|---|
| Neurobiological Dysfunction | Suggests abnormal processing of pain signals in the central nervous system, potentially involving altered neurotransmitter function. |
| Genetic Predisposition | Implies a hereditary component, where individuals with certain genetic markers might be more susceptible to developing the condition. |
| Environmental Factors | Posits that environmental stressors, such as infections, trauma, or significant life events, can trigger or exacerbate primary fibromyalgia. |
| Interaction of Multiple Factors | Recognizes that the development of primary fibromyalgia likely involves a complex interplay of genetic, neurobiological, and environmental factors. |
Secondary Fibromyalgia
Secondary fibromyalgia isn’t a distinct condition in itself, but rather a manifestation of fibromyalgia symptoms arising from another underlying medical issue. It’s crucial to understand that the symptoms are not caused by the underlying condition directly but are often a complex consequence of the body’s response to it. This response can involve various physiological and psychological mechanisms. Identifying and addressing the root cause is vital for effective management.Secondary fibromyalgia often shares overlapping symptoms with primary fibromyalgia, making diagnosis challenging.
However, the presence of a clear link to another medical condition is the key differentiator. Differentiating between primary and secondary fibromyalgia necessitates a thorough medical evaluation, including a complete medical history, physical examination, and potentially diagnostic tests to identify the contributing factors.
Conditions Associated with Secondary Fibromyalgia
A variety of medical conditions can trigger or exacerbate the development of secondary fibromyalgia. These conditions can impact various systems within the body, from the musculoskeletal to the neurological and immune systems. Understanding these connections is essential for comprehensive care.
- Chronic Fatigue Syndrome (CFS): CFS often coexists with fibromyalgia, characterized by persistent fatigue, sleep disturbances, and cognitive difficulties. The overlap suggests shared pathophysiological mechanisms potentially involving immune system dysfunction or neurotransmitter imbalances.
- Rheumatoid Arthritis (RA): Chronic inflammation associated with RA can lead to widespread pain and stiffness, mimicking fibromyalgia symptoms. The shared inflammatory response may contribute to the development of secondary fibromyalgia in some individuals.
- Lupus: Systemic lupus erythematosus (SLE) is an autoimmune disorder that can cause a range of symptoms, including widespread pain, fatigue, and cognitive dysfunction. The chronic inflammatory nature of lupus may be a factor in the development of secondary fibromyalgia.
- Multiple Sclerosis (MS): The neurological damage caused by MS can result in pain, fatigue, and sensory disturbances that overlap with fibromyalgia symptoms. The neurological involvement may be a crucial factor in the development of secondary fibromyalgia in some cases.
- Post-Traumatic Stress Disorder (PTSD): Experiencing a traumatic event can significantly impact the body’s physiological and psychological well-being. The resulting stress response may contribute to the development of secondary fibromyalgia, especially when coupled with other physical or psychological conditions.
Pathophysiological Mechanisms
The precise pathophysiological mechanisms linking various conditions to secondary fibromyalgia are not fully understood. However, several potential factors are implicated.
- Chronic Inflammation: Many conditions associated with secondary fibromyalgia involve chronic inflammation. This inflammation can trigger a cascade of events leading to widespread pain, fatigue, and other symptoms associated with fibromyalgia.
- Neurotransmitter Imbalances: Some research suggests that neurotransmitter dysregulation, such as serotonin and norepinephrine imbalances, may play a role in both primary and secondary fibromyalgia. The presence of underlying conditions may exacerbate these imbalances, contributing to the development of symptoms.
- Immune System Dysfunction: Dysfunction in the immune system has been linked to various conditions associated with secondary fibromyalgia. This dysfunction may lead to a heightened inflammatory response, impacting various tissues and organs, potentially contributing to widespread pain and fatigue.
- Central Sensitization: Conditions that involve chronic pain or nerve damage can lead to central sensitization. This altered processing of pain signals in the central nervous system can result in widespread pain and other symptoms, potentially leading to secondary fibromyalgia.
Potential Triggers
Various factors can potentially trigger or exacerbate secondary fibromyalgia in individuals with underlying conditions.
- Stress: Stressful life events, including physical or emotional trauma, can significantly impact the body’s physiological and psychological responses, possibly contributing to or worsening secondary fibromyalgia symptoms.
- Medications: Certain medications can have side effects that mimic or worsen fibromyalgia symptoms, particularly those targeting chronic pain or inflammation. Proper medication management is essential.
- Infection: Infections, especially chronic infections, can trigger or exacerbate underlying conditions and contribute to secondary fibromyalgia.
- Lifestyle Factors: Unhealthy lifestyle choices, such as poor diet, lack of exercise, and inadequate sleep, can worsen existing conditions and potentially contribute to the development of secondary fibromyalgia.
Conditions Potentially Causing Secondary Fibromyalgia
| Condition | Associated Symptoms |
|---|---|
| Chronic Fatigue Syndrome | Persistent fatigue, sleep disturbances, cognitive difficulties |
| Rheumatoid Arthritis | Widespread pain, stiffness, inflammation |
| Lupus | Widespread pain, fatigue, cognitive dysfunction, skin rashes |
| Multiple Sclerosis | Neurological symptoms, pain, fatigue, sensory disturbances |
| Post-Traumatic Stress Disorder | Anxiety, depression, flashbacks, nightmares, sleep disturbances |
Differentiating Primary and Secondary Fibromyalgia
Understanding the distinctions between primary and secondary fibromyalgia is crucial for accurate diagnosis and tailored treatment. While both conditions share overlapping symptoms, their underlying causes and diagnostic pathways differ significantly. This difference in origins influences the course and prognosis of the illness.Primary fibromyalgia, often seen as an idiopathic condition, is characterized by a complex interplay of genetic and environmental factors that contribute to its development.
Secondary fibromyalgia, conversely, is frequently linked to another identifiable medical condition or event. Distinguishing these two types is essential for guiding appropriate medical interventions and management strategies.
Symptom Comparison
The symptoms of primary and secondary fibromyalgia can overlap, but subtle differences exist. Primary fibromyalgia often presents with widespread pain, fatigue, and sleep disturbances as the initial and dominant symptoms. Secondary fibromyalgia, in contrast, may present with pain and fatigue alongside symptoms specific to the underlying condition. For instance, if the secondary cause is lupus, the patient may exhibit joint inflammation and skin rashes alongside the fibromyalgia symptoms.
Diagnostic Approaches
Diagnostic approaches for primary and secondary fibromyalgia differ based on the suspected cause. Primary fibromyalgia relies heavily on a comprehensive medical history, physical examination, and symptom assessment. Clinicians use standardized pain scales and questionnaires to gauge the severity and distribution of pain. In secondary fibromyalgia, the diagnostic process involves identifying the underlying condition first. The assessment then focuses on evaluating the symptoms of fibromyalgia within the context of the primary condition.
For example, if the patient has rheumatoid arthritis, the rheumatologist would consider both the arthritis-related symptoms and the potential fibromyalgia symptoms to formulate a complete diagnosis.
Risk Factors
Identifying potential risk factors is important for both primary and secondary fibromyalgia. For primary fibromyalgia, genetic predisposition, stress, and trauma are frequently implicated. For secondary fibromyalgia, the risk factors are intricately linked to the underlying cause. For instance, individuals with a history of trauma or chronic infections are at higher risk of developing secondary fibromyalgia. It’s important to remember that these are risk factors, not definitive causes.
Course and Prognosis
| Characteristic | Primary Fibromyalgia | Secondary Fibromyalgia |
|---|---|---|
| Symptom Onset | Often insidious, developing gradually over time. | May occur abruptly or gradually, often triggered by a specific event. |
| Symptom Progression | Generally chronic, with periods of fluctuating severity. | May fluctuate alongside the progression of the underlying condition; if the underlying condition is resolved, symptoms may improve. |
| Treatment Response | Varied; some individuals respond well to medication and lifestyle interventions, while others experience limited relief. | Treatment response often depends on the efficacy of treatment for the underlying condition; improvement in the underlying condition often leads to improvement in fibromyalgia symptoms. |
| Prognosis | Chronic condition requiring ongoing management. | Dependent on the prognosis of the underlying condition; if the underlying condition is managed, the secondary fibromyalgia may also improve. |
Typical Presentation
The typical presentation of primary fibromyalgia often involves a gradual onset of widespread pain, fatigue, and sleep disturbances. The pain may be described as aching, burning, or stabbing, and is typically present for at least three months. In secondary fibromyalgia, the symptom presentation is often influenced by the underlying condition. For instance, a patient with lupus might initially present with joint pain, fatigue, and sleep disturbances characteristic of lupus, with the fibromyalgia symptoms developing over time.
Management Strategies
Managing fibromyalgia, whether primary or secondary, requires a multifaceted approach focusing on pain relief, symptom management, and overall well-being. Effective strategies often involve a combination of therapies and lifestyle adjustments tailored to the individual’s specific needs and the underlying cause, if applicable. This personalized approach is crucial for achieving optimal outcomes.Effective management strategies for fibromyalgia address not only the physical symptoms but also the significant impact on mental health and daily functioning.
Understanding the specific needs of each individual is paramount, as different treatments and combinations of therapies may be more or less effective depending on the person.
Figuring out if your fibromyalgia is primary or secondary can be tricky, right? While there’s no magic bullet, some folks explore natural remedies like apple cider vinegar shots apple cider vinegar shots for potential symptom relief. Ultimately, accurate diagnosis and treatment plans are crucial for managing fibromyalgia, no matter the type.
Common Management Strategies for Primary Fibromyalgia
A variety of strategies are employed to manage primary fibromyalgia, aiming to reduce pain, improve sleep, and enhance overall function. These approaches are typically holistic, recognizing the interconnectedness of physical, emotional, and mental well-being.
- Pharmacological Interventions: Medications such as antidepressants (e.g., duloxetine, milnacipran) and anticonvulsants (e.g., pregabalin, gabapentin) are often prescribed to help manage pain and other symptoms. These medications can be used individually or in combination, and their effectiveness varies from person to person.
- Physical Therapy: Physical therapy plays a crucial role in managing pain and improving mobility. Exercises tailored to the individual’s capabilities, such as range-of-motion exercises, stretching, and strengthening exercises, can help alleviate pain and stiffness. Physical therapists can also teach patients proper posture and body mechanics to reduce strain on the body.
- Occupational Therapy: Occupational therapy focuses on adapting daily activities and environments to accommodate the limitations imposed by fibromyalgia. This may involve modifying work tasks, home routines, and using assistive devices to minimize physical strain and improve overall function. This includes evaluating and modifying activities, adapting workspaces, and selecting assistive devices for easier and less painful task completion.
- Lifestyle Modifications: Regular exercise, a balanced diet, and stress management techniques are essential components of fibromyalgia management. Consistent exercise, even in short bursts, can improve mood, reduce pain, and increase energy levels. Maintaining a healthy diet rich in nutrients supports overall well-being and can indirectly influence symptom management. Stress reduction techniques, such as yoga, meditation, or deep breathing exercises, can help manage emotional distress and its impact on pain perception.
Management Strategies for Secondary Fibromyalgia, Fibromyalgia primary or secondary
When fibromyalgia is secondary to another medical condition, the management strategy must address both the underlying condition and the symptoms of fibromyalgia. This necessitates a comprehensive approach that considers the interplay between the two.
- Treating the Underlying Condition: Prioritizing the treatment of the underlying cause is crucial. For example, if the secondary fibromyalgia is related to rheumatoid arthritis, the treatment plan would include managing the arthritis alongside the fibromyalgia symptoms. Effective management of the primary condition often leads to improved fibromyalgia symptoms.
- Symptom-Specific Interventions: Managing the pain and other symptoms associated with both conditions is critical. Treatments may include the same approaches used for primary fibromyalgia, such as medications, physical therapy, and lifestyle modifications, adapted as needed to address the specific needs of the underlying condition.
- Multidisciplinary Collaboration: Collaboration between specialists treating the underlying condition and fibromyalgia specialists is essential to ensure a holistic and coordinated approach. This ensures that the treatments for both conditions are complementary and avoid any negative interactions.
Comparison of Treatment Approaches
While both primary and secondary fibromyalgia management strategies often overlap, key differences arise from the presence or absence of an underlying condition.
- Primary Fibromyalgia: Treatment focuses on managing the symptoms directly, employing various therapies and lifestyle modifications without the need to address an underlying cause.
- Secondary Fibromyalgia: Treatment requires a dual approach, focusing on both the underlying condition and the fibromyalgia symptoms. Addressing the underlying cause often significantly impacts fibromyalgia symptom management.
Interdisciplinary Care
Interdisciplinary care plays a critical role in managing both primary and secondary fibromyalgia. This collaborative approach brings together specialists from various fields, including physicians, physical therapists, occupational therapists, psychologists, and social workers.
- Holistic Approach: Interdisciplinary care fosters a holistic approach to patient care, addressing the diverse aspects of fibromyalgia, including physical, emotional, and social needs.
- Personalized Treatment Plans: Collaborative efforts lead to the development of personalized treatment plans that consider the unique needs and circumstances of each individual.
- Improved Outcomes: A coordinated approach improves treatment outcomes by ensuring that all relevant factors are considered and addressed.
Treatment Modalities Table
| Treatment Modality | Primary Fibromyalgia | Secondary Fibromyalgia |
|---|---|---|
| Pharmacological Interventions | Antidepressants, anticonvulsants | Antidepressants, anticonvulsants, medications for underlying condition |
| Physical Therapy | Exercise, stretching, mobility improvement | Exercise, stretching, mobility improvement, tailored to underlying condition |
| Occupational Therapy | Adaptive strategies, assistive devices | Adaptive strategies, assistive devices, tailored to underlying condition |
| Lifestyle Modifications | Regular exercise, balanced diet, stress management | Regular exercise, balanced diet, stress management, lifestyle changes related to underlying condition |
| Interdisciplinary Care | Essential for holistic approach | Crucial for coordinated care and addressing both conditions |
Illustrative Case Studies
Understanding the complexities of fibromyalgia often requires delving into real-world scenarios. These case studies, while hypothetical, aim to highlight the diverse presentations and management approaches for primary and secondary fibromyalgia, emphasizing the nuances in diagnosis and treatment. The distinctions between these two forms are crucial for developing effective and personalized care plans.
Case Study 1: Primary Fibromyalgia
This case study focuses on a 35-year-old woman, Sarah, presenting with a gradual onset of widespread pain over the past five years. Her pain is described as a deep, aching sensation, affecting her entire body. Accompanying symptoms include fatigue, sleep disturbances, and cognitive difficulties, which significantly impact her daily life. She reports frequent headaches and irritable bowel syndrome.
- Medical History: Sarah has a family history of anxiety and depression, but no known autoimmune conditions. She reports no significant past traumas or infections. Her physical examinations are unremarkable, revealing no specific physical abnormalities.
- Diagnostic Process: A comprehensive evaluation, including a thorough medical history, physical examination, and symptom assessment, is crucial. The diagnostic criteria for fibromyalgia, focusing on widespread pain and accompanying symptoms, are considered. Blood tests and imaging studies are often conducted to rule out other conditions, such as rheumatoid arthritis or lupus. Sarah’s responses to standardized questionnaires for fibromyalgia symptom assessment were suggestive of the condition.
- Treatment Plan: The treatment plan for Sarah emphasizes a multidisciplinary approach. This includes medication for pain management, such as non-steroidal anti-inflammatory drugs (NSAIDs), antidepressants, or other medications as prescribed by her physician. Alongside medication, stress management techniques, such as yoga, meditation, or counseling, are encouraged to address anxiety and mood issues. Physical therapy and exercise, tailored to her abilities and pain levels, can also improve mobility and function.
Case Study 2: Secondary Fibromyalgia
This case study involves a 48-year-old man, David, who developed widespread pain symptoms after experiencing a significant injury, including a whiplash-associated disorder, three years prior. He initially experienced pain in the neck and shoulders but now describes widespread pain, accompanied by muscle spasms, and pronounced fatigue.
- Medical History: David’s medical history reveals a recent severe motor vehicle accident that led to a whiplash injury. He also reports having a history of chronic back pain due to a previous injury, although the severity has increased significantly after the accident. He has also reported intermittent gastrointestinal issues.
- Diagnostic Process: The diagnostic process for David involves a thorough evaluation of his symptoms, including a careful examination of his accident history. A neurological evaluation to assess nerve function and spinal integrity is essential, alongside diagnostic imaging (X-rays, MRIs) to identify any physical abnormalities resulting from the accident. Laboratory tests may be performed to rule out other conditions.
In this case, careful correlation of symptoms with the accident history and subsequent physical evaluations will be critical for diagnosis.
- Treatment Plan: The treatment plan for David requires a more comprehensive approach, recognizing the underlying cause of his fibromyalgia. Addressing the whiplash-associated disorder is crucial. This may involve physical therapy, pain management techniques, and potentially medication for pain relief. The treatment also focuses on addressing his general health and well-being, including stress management and improving sleep quality. Crucially, the treatment plan must incorporate rehabilitation exercises for his neck and back to restore function and reduce chronic pain.
Closing Summary: Fibromyalgia Primary Or Secondary
In conclusion, differentiating between primary and secondary fibromyalgia is essential for personalized treatment plans. While both types share similar symptoms, their underlying causes and management approaches differ significantly. Understanding these distinctions is vital for patients and healthcare professionals to navigate the diagnostic and therapeutic journey effectively. By examining the causes, symptoms, and management strategies for each type, we can better equip ourselves to provide optimal care and support for those living with fibromyalgia.