Epiretinal membrane retinal scar tissue forms a delicate yet significant threat to vision. This intricate web of scar tissue, often developing on the retina, can lead to a range of visual disturbances. Understanding its formation, diagnosis, and treatment options is crucial for effective management and preserving sight. This post will explore the specifics of this condition, from its definition and symptoms to treatment options and prognosis.
The formation of epiretinal membrane (ERM) is often linked to the underlying cause of the retinal scar tissue, which could stem from injury, inflammation, or age-related factors. This scar tissue, when located on the retina, can distort vision, leading to significant impairment if not addressed. We’ll explore the different ways this condition is diagnosed and the various treatment approaches available, ranging from medications to surgical procedures.
This comprehensive look at ERM and retinal scar tissue will be invaluable for patients, families, and healthcare professionals alike.
Defining Epiretinal Membrane and Retinal Scar Tissue
Epiretinal membranes (ERMs) and retinal scar tissue are common concerns in eye care, often arising from various eye conditions. Understanding their formation, characteristics, and relationship to the retina is crucial for diagnosis and treatment. This discussion delves into the specifics of ERMs, their connection to scar tissue development, and how they differ from other retinal pathologies.Epiretinal membranes are abnormal layers of tissue that grow over the surface of the retina.
These membranes, composed of cells and extracellular matrix, can lead to the development of scar tissue. The precise mechanisms driving the formation of this scar tissue are complex, involving inflammatory responses and abnormal cell proliferation.
Definition of Epiretinal Membrane (ERM)
An epiretinal membrane (ERM) is a thin, translucent layer of scar tissue that grows over the surface of the retina, typically in the macula, which is the central part of the retina responsible for sharp central vision. This membrane can cause distortion and blurring of central vision.
Dealing with epiretinal membrane retinal scar tissue can be tough, but focusing on overall health can help. While I’m no doctor, I’ve heard that certain herbal remedies can help with general cold symptoms, and best teas for a cold might offer some soothing relief. Of course, this is no substitute for professional medical advice, but a healthy lifestyle, including good hydration and rest, could potentially aid in the healing process for epiretinal membrane retinal scar tissue.
Formation of Retinal Scar Tissue in ERM
The development of scar tissue in ERM is a consequence of the inflammatory response and abnormal cell proliferation associated with the membrane’s formation. Inflammation triggers the release of growth factors that promote the growth and accumulation of extracellular matrix proteins, which contribute to the formation of the scar tissue. This process can lead to significant visual impairment if not addressed.
Anatomical Location and Relationship to the Retina, Epiretinal membrane retinal scar tissue
ERMs typically originate from the retinal pigment epithelium (RPE) and other adjacent tissues. They grow over the neurosensory retina, often in the macula. This location, directly over the light-sensitive photoreceptor cells, creates the potential for significant visual impairment as the membrane distorts the normal retinal structure.
Comparison with Other Retinal Pathologies
While ERMs and other retinal pathologies can lead to visual impairment, they have distinct characteristics. Macular holes, for example, are focal defects in the macula, resulting in a small, dark area in the central vision, while ERMs are more widespread, growing over the surface of the retina. Age-related macular degeneration (AMD) presents with different visual symptoms and underlying mechanisms compared to ERMs.
Furthermore, diabetic retinopathy often involves blood vessel abnormalities rather than the membrane growth that defines ERMs.
Key Differences Between ERM and Macular Hole
| Feature | Epiretinal Membrane (ERM) | Macular Hole |
|---|---|---|
| Location | Over the surface of the retina, often in the macula. | A focal defect in the macula. |
| Appearance | Thin, translucent layer. | A small, dark area in the central vision. |
| Cause | Inflammation, abnormal cell proliferation. | Unknown, but likely related to structural weakness in the macula. |
| Visual Impact | Distortion and blurring of central vision. | Loss of central vision. |
Symptoms and Diagnosis
Epiretinal membrane (ERM) and retinal scar tissue, though often subtle in their early stages, can lead to significant vision impairment if left untreated. Understanding the symptoms and diagnostic procedures is crucial for timely intervention and effective management. This section delves into the common visual complaints associated with ERM and retinal scar tissue, and Artikels the various diagnostic methods used to identify and characterize these conditions.Identifying the specific symptoms and accurately diagnosing epiretinal membranes and retinal scar tissue is crucial for timely intervention and effective treatment.
Early detection allows for appropriate management and potentially better outcomes. The visual symptoms, often subtle initially, can progressively worsen over time. Diagnostic procedures are designed to not only confirm the presence of ERM or retinal scar tissue but also to evaluate its extent and impact on vision.
Visual Symptoms
Patients with ERM and retinal scar tissue often experience a range of visual symptoms. These symptoms can include blurred vision, distortion of straight lines (metamorphopsia), difficulty with night vision, and reduced visual acuity. The presence of floaters, or small specks or shadows that drift in the field of vision, is also sometimes reported. The severity of these symptoms can vary significantly depending on the size, location, and density of the membrane or scar tissue.
Diagnostic Procedures
Several diagnostic procedures are employed to identify and characterize epiretinal membranes and retinal scar tissue. These methods help ophthalmologists assess the extent of the condition and its impact on the patient’s vision. A comprehensive eye examination is crucial, incorporating a thorough evaluation of the patient’s medical history and visual symptoms.
Ophthalmoscopy
Ophthalmoscopy, a fundamental diagnostic tool, allows visualization of the interior structures of the eye, including the retina. During ophthalmoscopy, a specialized instrument is used to illuminate the retina, enabling the ophthalmologist to observe the surface of the retina for the presence of abnormalities. Direct ophthalmoscopy, utilizing a direct lens, provides a magnified view of the retina, which is especially helpful in identifying the presence of a membrane or scar tissue.
Epiretinal membrane retinal scar tissue can be a tricky condition, affecting vision. While researching the complexities of this eye issue, I stumbled across some fascinating historical context about diseases. For example, the history of breast cancer, with its long and complex journey of diagnosis and treatment, offers a valuable comparison to the challenges faced with understanding and managing epiretinal membrane retinal scar tissue.
Ultimately, understanding the history of such diseases can shed light on the progress made in healthcare and the long road ahead in finding effective treatments for eye conditions like epiretinal membrane retinal scar tissue. history of breast cancer
Indirect ophthalmoscopy, employing an indirect lens, provides a broader field of view, useful for evaluating the entire retina. The presence of a pearly-white membrane or scar tissue with a slightly elevated appearance is often apparent during ophthalmoscopic examination.
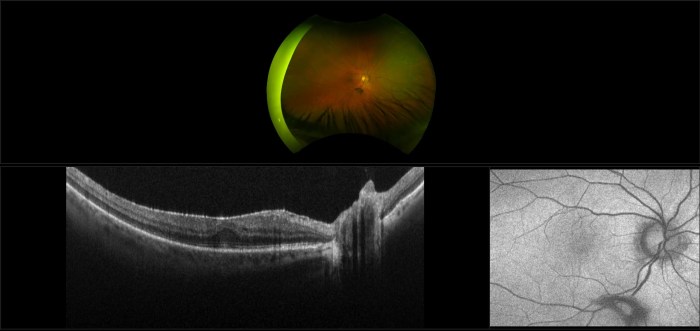
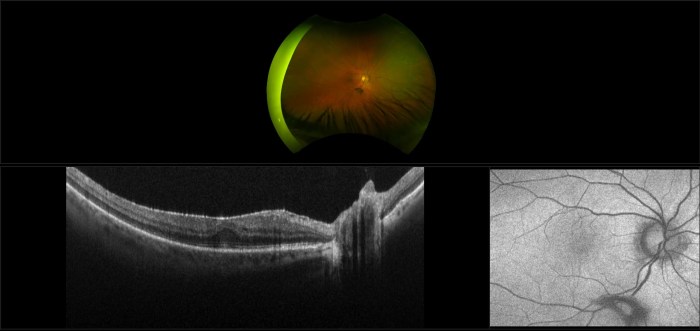
Optical Coherence Tomography (OCT)
Optical coherence tomography (OCT) is a non-invasive imaging technique that provides detailed cross-sectional images of the retina. OCT scans are particularly valuable in diagnosing ERM and retinal scar tissue because they offer high-resolution images of the retinal layers. The images generated by OCT reveal the precise location, thickness, and extent of the membrane or scar tissue, helping to distinguish it from other retinal conditions.
The OCT scan will reveal a distinct elevation of the retina where the epiretinal membrane is attached.
Summary of Diagnostic Tests
| Diagnostic Test | Procedure | Expected Result |
|---|---|---|
| Ophthalmoscopy | Visual examination of the retina using a specialized instrument. | Presence of a pearly-white, elevated membrane or scar tissue. |
| Optical Coherence Tomography (OCT) | Non-invasive imaging technique that provides detailed cross-sectional images of the retina. | Distinct elevation of the retina where the membrane or scar tissue is attached; precise measurement of the membrane’s thickness. |
Treatment Options
Epiretinal membrane (ERM) and retinal scar tissue can significantly impact vision. Fortunately, various treatment options are available, ranging from observation to surgical interventions. The best approach depends on the severity of the condition, the patient’s overall health, and the location of the ERM within the retina.Understanding the mechanisms of action of these treatments is crucial for patients and healthcare providers to make informed decisions about the best course of action.
Different modalities target different aspects of the disease, from reducing inflammation to removing scar tissue. This section will explore the diverse array of treatment strategies available for managing ERM and retinal scar tissue.
Available Treatment Options
A range of treatment options are available, from watchful waiting to surgical procedures, and anti-VEGF therapy. The optimal choice depends on the individual patient’s situation.
- Observation: In some cases, especially for early-stage or mild ERM, a period of watchful waiting may be appropriate. This approach involves regular eye examinations to monitor the progression of the condition. This is often a suitable option for patients who do not experience significant symptoms and whose ERM is not causing significant macular edema.
- Anti-VEGF Therapy: Vascular endothelial growth factor (VEGF) is a protein that plays a role in the development of new blood vessels. In ERM-related macular edema, VEGF can contribute to fluid buildup. Anti-VEGF medications, such as ranibizumab (Lucentis) or aflibercept (Eylea), work by blocking VEGF, thus reducing fluid leakage and inflammation in the macula, which is the central part of the retina.
This can help improve vision and slow the progression of the disease.
- Surgical Intervention: Surgical removal of the ERM is an option for patients who experience significant vision loss due to the ERM and macular edema. Surgical techniques involve carefully separating the ERM from the retina, often using specialized instruments. The procedure is typically performed by ophthalmologists experienced in vitreoretinal surgery.
Mechanism of Action
The specific mechanisms of action for each treatment modality vary depending on the method chosen.
- Anti-VEGF therapy targets the overproduction of VEGF, a key player in the formation of new blood vessels. By inhibiting VEGF, these medications reduce the fluid leakage that contributes to macular edema and retinal inflammation. This, in turn, can improve vision and slow the progression of the condition.
- Surgical intervention aims to physically remove the epiretinal membrane, reducing the pressure on the retina. The surgical approach can involve techniques like peeling the membrane off the retina, using specialized instruments and precise techniques. The goal is to improve retinal function and reduce macular edema by relieving the mechanical stress on the retina caused by the ERM.
Surgical Procedures for ERM Removal
Surgical procedures for ERM removal are typically performed by experienced ophthalmologists specializing in vitreoretinal surgery.
- Vitrectomy: This surgical procedure involves the removal of the vitreous humor, the gel-like substance that fills the eye. The removal of the vitreous creates space, making it easier to access and separate the ERM from the retina. Once the vitreous is removed, the ERM is carefully peeled away from the retina using specialized instruments. This procedure allows for better visualization and manipulation of the ERM and surrounding tissues, improving the likelihood of successful removal.
Role of Anti-VEGF Therapies
Anti-VEGF therapies play a crucial role in managing macular edema associated with ERM. The effectiveness of anti-VEGF therapy is often evaluated by the degree of improvement in visual acuity and the reduction in macular edema.
| Treatment Approach | Mechanism of Action | Risks | Benefits |
|---|---|---|---|
| Observation | Monitor condition without intervention | Potential for vision loss if condition progresses | Avoids potential risks of more invasive procedures |
| Anti-VEGF Therapy | Blocks VEGF, reducing fluid leakage | Potential for side effects (e.g., eye infections, retinal detachment), injections are required | Can improve vision, slow progression, and reduce macular edema |
| Surgical Intervention | Remove ERM from retina | Potential for complications (e.g., retinal detachment, infection), longer recovery time | Can significantly improve vision, particularly when macular edema is present |
Prognosis and Management: Epiretinal Membrane Retinal Scar Tissue
Epiretinal membrane (ERM) and associated retinal scar tissue can significantly impact vision. Understanding the potential outcomes and proactive management strategies is crucial for patients and their eye care professionals. This section will delve into the prognosis, emphasizing the importance of regular follow-ups and potential long-term complications. We will also explore strategies for managing the visual consequences.The prognosis for ERM varies greatly depending on several factors.
These include the extent of the membrane, its location on the retina, and the presence of other eye conditions. While some individuals experience minimal visual impairment, others may face more substantial reductions in vision quality.
Typical Prognosis
The typical prognosis for ERM depends on the extent of the membrane’s growth and its location on the retina. Early detection and prompt intervention are crucial for optimizing visual outcomes. In many cases, ERM does not cause significant vision loss. However, if the membrane is extensive or involves critical retinal areas, it can result in noticeable visual disturbances.
Importance of Regular Follow-up Appointments
Regular follow-up appointments are essential for monitoring the progression of ERM and associated retinal scarring. These appointments allow eye care professionals to track any changes in the membrane’s size or location, as well as assess the impact on vision. Early intervention can often prevent further vision loss. The frequency of follow-ups will depend on the individual’s specific case and the rate of membrane progression.
Potential Long-Term Complications
Potential long-term complications associated with ERM and retinal scar tissue include further vision loss, particularly if the membrane continues to grow or contract abnormally. In some instances, the membrane can cause distortion of the retinal image, leading to problems with central vision. The risk of these complications can be reduced with appropriate management and consistent follow-up care. Another potential complication is the development of macular edema, a swelling of the macula (the central part of the retina responsible for sharp vision).
This swelling can worsen existing vision problems.
Visual Outcomes Based on Stage and Treatment
| Stage of ERM | Treatment Options | Potential Visual Outcome |
|---|---|---|
| Early stage, minimal membrane | Observation, close monitoring | Minimal to no significant vision loss |
| Moderate stage, membrane affecting central vision | Laser photocoagulation, vitrectomy | Potential for some vision improvement or stabilization, some vision loss possible |
| Advanced stage, extensive membrane and significant retinal scarring | Vitrectomy with membrane peeling, potential for multiple treatments | Potential for partial or significant vision loss, depending on the extent of the membrane and scar tissue. Improvement is less likely. |
Note
* This table provides a general overview. Individual outcomes may vary based on several factors including the individual’s overall eye health and the response to treatment.
Epiretinal membrane retinal scar tissue can significantly impact vision, often causing distortions and blurry images. Understanding the intricate pathways of the ophthalmic nerve, including its anatomy, function, and significance, like this insightful article , is crucial to comprehending how these changes affect the transmission of visual information. Ultimately, a thorough knowledge of the ophthalmic nerve’s role is essential to effectively treating and managing epiretinal membrane retinal scar tissue.
Strategies for Managing Visual Consequences
Managing the visual consequences of ERM and retinal scar tissue involves a multi-faceted approach. This often includes:
- Close monitoring: Regular eye exams to track the progression of the condition and any changes in vision.
- Treatment options: Using laser therapy, vitrectomy, or other procedures to reduce the size or impact of the membrane and associated scar tissue.
- Management of other eye conditions: Addressing any other underlying eye conditions that may contribute to the progression of ERM or retinal scarring.
- Addressing symptoms: Managing any symptoms experienced, such as blurry vision or floaters, with appropriate measures.
- Rehabilitation strategies: Adapting to any changes in vision with assistive technologies and techniques.
The goal is to slow or stop the progression of the condition and improve or stabilize vision, whenever possible.
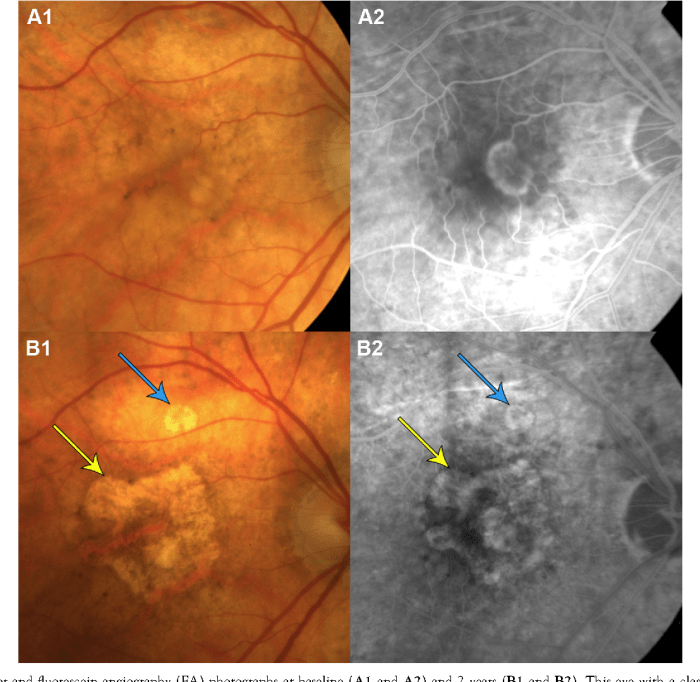
Illustrative Cases
Epiretinal membrane (ERM) can significantly impact vision, and understanding its progression and response to treatment is crucial. Real-world cases provide valuable insights into the complexities of ERM management and the variability in outcomes. These illustrative examples demonstrate the challenges and triumphs in managing ERM, highlighting both the potential for positive visual recovery and the need for careful patient-specific strategies.
Progression of ERM in a Patient Case Study
A 65-year-old female patient presented with a gradual blurring of vision over the past two years. Initial ophthalmic examination revealed an epiretinal membrane (ERM) with a mild degree of macular thickening. The patient’s visual acuity was 20/40 in the affected eye. Over the next year, the ERM gradually thickened, and the patient’s visual acuity deteriorated to 20/60.
This gradual progression is common in ERM cases, and careful monitoring is vital to detect and address potential exacerbations. Addressing this progression with appropriate intervention could potentially mitigate further decline in visual function.
Impact of Treatment on Visual Outcomes in a Specific Patient
A 72-year-old male patient presented with a moderate ERM and visual acuity of 20/80 in his right eye. He underwent a vitrectomy procedure to remove the ERM. Post-operative visual acuity improved to 20/50. This case illustrates how timely and appropriate intervention can lead to tangible improvements in visual function. The specific results will vary based on the severity of the ERM, the patient’s underlying health, and the success of the surgical procedure.
Visual Acuity and Other Parameters Before, During, and After Treatment
| Parameter | Before Treatment | During Treatment | After Treatment |
|---|---|---|---|
| Visual Acuity (Snellen) | 20/80 | 20/80 (Pre-vitrectomy) | 20/50 |
| ERM Thickness (µm) | 150 | 150 (Pre-vitrectomy) | 100 |
| Macular Oedema (Grading) | Moderate | Moderate (Pre-vitrectomy) | Mild |
| Intraocular Pressure (mmHg) | 16 | 16 | 16 |
| Comorbidities | Hypertension | Hypertension | Hypertension |
This table demonstrates the pre-treatment, during-treatment, and post-treatment parameters of a patient undergoing vitrectomy for ERM. These parameters are essential in assessing the effectiveness of the treatment. It is crucial to monitor these parameters in each patient to provide personalized and comprehensive care.
Management of ERM and Retinal Scar Tissue in a Patient with Comorbidities
A 55-year-old patient with diabetes and hypertension presented with an ERM and accompanying retinal scar tissue. The management plan prioritized meticulous monitoring of blood sugar and blood pressure to mitigate potential complications. The patient’s overall health status influenced the choice of treatment, and the surgical approach was tailored to minimize the risk of complications. Comprehensive care involving ophthalmologists and other specialists, including diabetologists and cardiologists, is crucial in cases with comorbidities.
This multidisciplinary approach ensures the patient receives holistic care, addressing the ERM and the associated systemic health concerns.
Case with Severe Visual Impairment due to ERM
A 78-year-old patient presented with a severe ERM causing significant visual impairment, with visual acuity of 20/200. The patient’s age and the severity of the ERM presented unique challenges in the treatment approach. Careful consideration was given to the potential risks and benefits of different surgical options. In such cases, a detailed discussion with the patient about the potential outcomes, risks, and realistic expectations is paramount.
This patient’s journey emphasizes the importance of individualized care plans and open communication between the healthcare team and the patient.
Research and Future Directions
Epiretinal membrane (ERM) and retinal scar tissue research is actively pursuing innovative strategies for improved diagnosis, treatment, and prevention. Understanding the intricate mechanisms behind ERM formation is crucial for developing more effective therapies and potentially preventing the condition altogether. This section explores current research areas, potential advancements, and the ongoing need for further investigation.
Current Research Areas
Current research into ERM and retinal scar tissue focuses on several key areas. Scientists are exploring the molecular mechanisms driving ERM formation, identifying specific cellular pathways and genetic factors involved. This includes investigating the role of inflammation, apoptosis, and extracellular matrix remodeling in the development of the scar tissue. Furthermore, research is examining the efficacy of various therapeutic approaches, including novel drug delivery systems and gene therapy techniques.
The ultimate goal is to develop personalized treatment strategies tailored to individual patient needs.
Potential Advancements in Treatment and Prevention
Several advancements hold promise for improving treatment and potentially preventing ERM. One promising avenue is the development of targeted therapies that directly address the underlying causes of ERM formation. This could involve inhibiting specific enzymes or signaling pathways that contribute to the disease process. Moreover, novel drug delivery systems may enhance the efficacy of existing treatments by increasing the concentration of active ingredients at the site of the ERM, minimizing systemic side effects.
Need for Further Research on ERM and Associated Pathologies
Despite significant progress, further research is critical to fully understand the complexities of ERM and its associated pathologies. A deeper understanding of the intricate interplay between genetic predisposition, environmental factors, and lifestyle choices in ERM development is needed. This would allow for more precise risk stratification and the development of preventive measures. Additionally, ongoing research into the long-term effects of existing treatments and the development of novel diagnostic tools is essential for optimizing patient outcomes.
Innovative Approaches to Diagnosing ERM and Retinal Scar Tissue
Innovative approaches to diagnosing ERM and retinal scar tissue include utilizing advanced imaging techniques. Optical coherence tomography (OCT) angiography is increasingly employed to visualize the retinal vasculature with greater precision, providing detailed information about the microcirculation and enabling early detection of subtle changes associated with ERM formation. Furthermore, artificial intelligence (AI) algorithms are being developed to analyze OCT images, potentially accelerating the diagnostic process and improving accuracy.
Potential Future Areas of Study on Mechanisms of ERM Formation
Future research should explore the role of specific cellular pathways and genetic factors in ERM formation. One potential area of investigation involves the study of cellular interactions between retinal pigment epithelial cells, photoreceptor cells, and glial cells. This could reveal crucial information about the precise sequence of events that lead to ERM development. Additionally, investigating the influence of environmental factors, such as oxidative stress and inflammation, on ERM pathogenesis will be critical for developing preventative strategies.
Conclusion
In conclusion, epiretinal membrane retinal scar tissue presents a complex challenge requiring a multifaceted approach to diagnosis and treatment. While the prognosis varies depending on the severity and stage of the condition, proactive management, including regular follow-up appointments and appropriate treatment, can significantly improve outcomes. Understanding the potential complications and long-term implications is crucial for effective patient care and informed decision-making.
This overview provides a solid foundation for understanding this often-overlooked retinal condition.