Comfort care vs hospice: Navigating these options can feel overwhelming, but understanding the nuances is key for making informed decisions. This exploration delves into the core philosophies, eligibility criteria, and practical considerations surrounding both approaches. We’ll examine the types of care provided, pain management strategies, family involvement, and even the ethical and financial aspects of each. It’s a journey into compassionate end-of-life care, and this guide aims to provide clarity and support in this often difficult process.
Comfort care focuses on improving quality of life by managing symptoms and providing emotional support, while hospice emphasizes comfort and support for those with life-limiting illnesses, generally when curative treatment is no longer an option. Key differences in goals and objectives, eligibility criteria, and service provisions will be highlighted throughout this comparison.
Defining Comfort Care and Hospice

Understanding the differences between comfort care and hospice care is crucial for navigating difficult decisions regarding end-of-life care. Both approaches aim to enhance the quality of life for individuals facing serious illnesses, but they differ significantly in their philosophies, goals, and timelines. This section will delineate the key distinctions between these two approaches.Comfort care focuses on managing symptoms and providing support to improve the patient’s overall well-being, while hospice care specifically addresses the needs of individuals with a life expectancy of six months or less.
Both aim to alleviate suffering and improve quality of life, but their approaches and timelines differ significantly.
Defining Comfort Care
Comfort care is a holistic approach to care that prioritizes symptom management and emotional support for individuals facing serious illnesses. It’s a fundamental aspect of healthcare, encompassing various strategies to improve the patient’s quality of life throughout their journey with a health condition. Comfort care doesn’t necessarily aim for a cure but rather focuses on ensuring comfort and minimizing pain and discomfort.
It can be provided alongside curative treatments or as the primary focus of care, depending on the patient’s wishes and prognosis. Comfort care encompasses a wide range of services, including pain management, medication adjustments, and emotional support.
Figuring out comfort care versus hospice can be tough, especially when dealing with health issues. Understanding your options is key, and knowing how to interpret your thyroid test results can be just as crucial. For example, if your thyroid levels are impacting your overall well-being, it could influence your choices regarding comfort care vs hospice. Ultimately, making the best decision for your health and quality of life requires careful consideration of all factors, including insights from interpret your thyroid test results , and a strong support system.
Understanding your options in comfort care and hospice is important, regardless of your thyroid status.
Defining Hospice Care
Hospice care is a specialized type of care designed for individuals with a life expectancy of six months or less, who are no longer seeking curative treatment. Its core philosophy emphasizes quality of life over curative measures. Hospice care teams work collaboratively to provide comprehensive support to the patient and their family, focusing on emotional, social, and spiritual well-being.
Key to hospice care is a holistic approach that considers the patient’s physical, emotional, and spiritual needs. Hospice care also provides support to the family through grief counseling and bereavement services.
Key Differences in Goals and Objectives
Comfort care and hospice care share the goal of improving quality of life, but their approaches and timelines differ significantly. Comfort care can be provided at any stage of an illness and alongside curative treatments. Hospice care, on the other hand, is specifically for individuals nearing the end of life, who are no longer seeking curative treatments. The primary objective of comfort care is to manage symptoms and provide support, while hospice care prioritizes comfort, emotional support, and bereavement services for the patient and their family.
Comparison of Comfort Care and Hospice Care
| Feature | Comfort Care | Hospice Care |
|---|---|---|
| Focus | Symptom management, pain relief, and overall well-being. Can be provided alongside curative treatment. | Providing comfort, emotional support, and bereavement services to patients and families. |
| Life Expectancy | Not limited to a specific time frame. | Typically for individuals with a life expectancy of six months or less. |
| Treatment Approach | Can include curative treatment alongside symptom management. | Focuses on comfort measures, not curative treatment. |
| Care Setting | Can be provided in various settings, including hospitals, nursing homes, and homes. | Typically provided in the patient’s home, hospice facility, or a skilled nursing facility. |
| Team Involvement | Involves various healthcare professionals, depending on the setting. | Involves a dedicated interdisciplinary team of professionals, including physicians, nurses, social workers, and counselors. |
Eligibility Criteria and Patient Selection: Comfort Care Vs Hospice
Choosing between comfort care and hospice care depends heavily on the individual patient’s needs and prognosis. Understanding the eligibility criteria for each approach is crucial for ensuring patients receive the most appropriate and compassionate care. This section delves into the specific criteria and provides examples to illustrate the distinctions.
Eligibility Criteria for Comfort Care
Comfort care focuses on providing relief from symptoms and improving the patient’s quality of life, rather than curing the underlying disease. Eligibility for comfort care is typically based on the patient’s overall condition and the goals of care. This means a patient may receive comfort care regardless of their prognosis or stage of illness. Key considerations often include the patient’s desire for comfort care, the presence of a serious illness, and the wishes of the patient and their family.
Eligibility Criteria for Hospice Care
Hospice care is a specialized approach for individuals with a life-limiting illness and a prognosis of six months or less if the disease runs its normal course. A key aspect of hospice eligibility is that curative treatments are no longer pursued. The focus shifts to managing symptoms and providing comfort and support to the patient and their family.
This type of care is typically delivered in the patient’s home or in a hospice facility.
Examples of Patients Benefiting from Each Approach
A patient with advanced cancer who is experiencing severe pain and wishes to focus on comfort rather than aggressive treatment may benefit from comfort care. Alternatively, a patient with a terminal illness such as ALS, who is approaching the end of their life, might qualify for hospice care to manage their symptoms and support their emotional needs. Comfort care can be appropriate for various conditions, including heart failure, chronic obstructive pulmonary disease (COPD), and dementia.
Hospice care, however, is specifically tailored for those nearing the end of life.
Transitions Between Comfort Care and Hospice
In some situations, a patient may transition from comfort care to hospice care. This typically happens when the patient’s condition deteriorates, their prognosis shortens, and they meet the criteria for hospice eligibility. For example, a patient receiving comfort care for a chronic illness may experience a rapid decline in health and meet the six-month prognosis criteria, triggering a shift to hospice.
Conversely, a patient initially enrolled in hospice might experience a temporary improvement in condition, allowing them to return to a focus on comfort care.
Table: Eligibility Requirements
| Criteria | Comfort Care | Hospice Care |
|---|---|---|
| Prognosis | No specific time frame, focused on symptom relief and quality of life | Life expectancy of six months or less if the disease runs its normal course; curative treatments are no longer pursued. |
| Treatment Goals | Symptom management and quality of life improvement | Symptom management, comfort, and support for the patient and family. |
| Patient Condition | Serious illness or condition | Terminal illness |
| Curative Treatment | May or may not be pursued, depending on patient preference and condition | Curative treatments are no longer pursued. |
Service Provision and Support
Navigating the complexities of comfort care and hospice requires a deep understanding of the services offered and the support systems available. This knowledge empowers patients and families to make informed decisions about the best course of action during challenging times. Comfort care focuses on improving the quality of life for individuals facing serious illness, while hospice care specifically supports those nearing the end of life.
Both approaches emphasize holistic well-being, recognizing the emotional and physical needs of patients and their families.
Types of Services Provided Under Comfort Care
Comfort care encompasses a wide range of services tailored to address the individual needs of patients. This care prioritizes symptom management, promoting comfort, and preserving dignity. Crucially, it’s about maximizing quality of life, not necessarily curing the illness.
- Symptom Management: Comfort care often involves managing symptoms like pain, nausea, shortness of breath, and anxiety. Medication adjustments and non-pharmacological interventions, such as relaxation techniques and guided imagery, play a vital role.
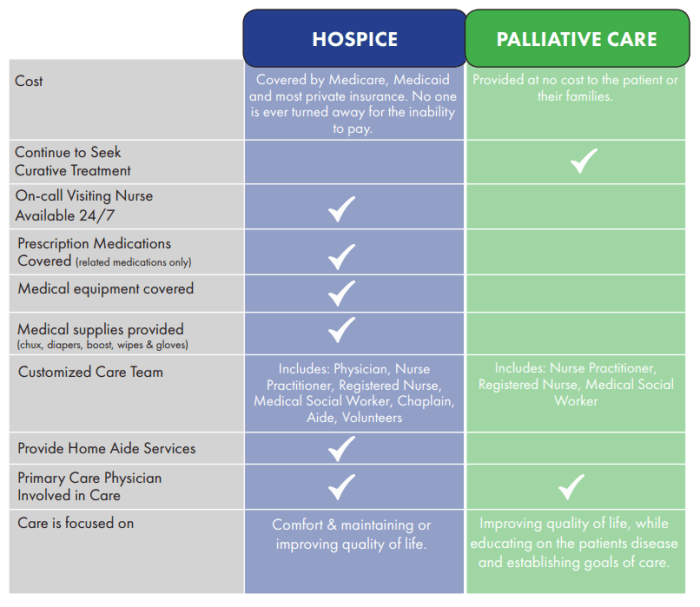
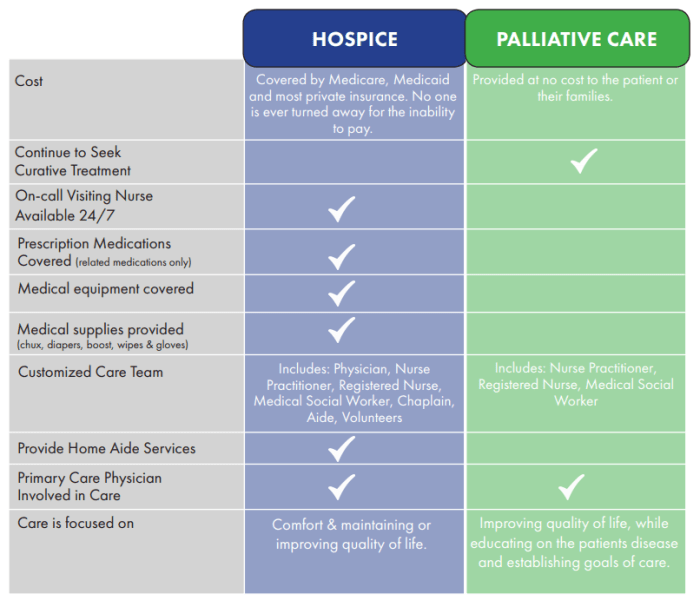
- Palliative Care: This includes specialized medical care focused on providing relief from the symptoms and stress of a serious illness. It is not limited to the end-of-life stage and can be provided alongside curative treatments.
- Emotional Support: Comfort care recognizes the emotional toll of serious illness on patients and their families. This support may include counseling, emotional support groups, and spiritual guidance.
- Practical Assistance: Helping with daily tasks like bathing, dressing, and meal preparation is sometimes incorporated into comfort care, making the experience less stressful for patients.
Types of Services Provided Under Hospice Care
Hospice care is specifically designed for individuals with a life expectancy of six months or less. It focuses on providing compassionate care and support to both the patient and their family. The goal is to enhance the quality of remaining life, emphasizing comfort and dignity.
- Symptom Management: Hospice care, like comfort care, prioritizes symptom management, including pain, nausea, and shortness of breath. Medication management is crucial, often focusing on symptom relief rather than curative treatment.
- Interdisciplinary Team: Hospice care often involves a team of professionals, including doctors, nurses, social workers, counselors, and spiritual advisors. This collaborative approach ensures a holistic approach to care.
- Emotional and Spiritual Support: Hospice care recognizes the importance of emotional and spiritual well-being for both the patient and family. Counseling, grief support, and spiritual guidance are often integrated into the care plan.
- Caregiver Support: Hospice recognizes the significant role caregivers play. They provide education, training, and respite care to help caregivers manage their own well-being.
- Bereavement Services: Hospice programs offer bereavement support to families after the loss of a loved one, providing resources and guidance through the grieving process.
Support Systems for Patients and Families
Both comfort care and hospice settings offer a range of support systems to help patients and families cope with the challenges of illness and loss.
- Family Support Groups: These groups provide a forum for sharing experiences, offering mutual support, and reducing feelings of isolation.
- Social Workers: Social workers help patients and families navigate the practical and emotional aspects of illness and loss, connecting them with necessary resources.
- Volunteers: Many hospice programs rely on volunteers to provide companionship, support, and assistance to patients and families.
- Spiritual Counselors: Spiritual guidance can be invaluable for providing comfort, support, and meaning during difficult times.
Role of Healthcare Professionals
Healthcare professionals play a critical role in both comfort care and hospice. Their expertise and compassion are essential in providing quality care.
- Doctors: Doctors assess patients’ needs, develop care plans, and prescribe medications.
- Nurses: Nurses provide direct patient care, monitor symptoms, and educate patients and families.
- Social Workers: Social workers address the psychosocial needs of patients and families, helping them navigate the complexities of illness and loss.
- Chaplains/Spiritual Counselors: These professionals provide spiritual guidance and support to patients and families.
Comparison of Care in Different Settings
| Setting | Comfort Care | Hospice Care |
|---|---|---|
| Focus | Improving quality of life for individuals with serious illness, regardless of prognosis. | Providing compassionate care and support to individuals with a life expectancy of six months or less. |
| Goal | Maximize comfort and well-being. | Enhance quality of remaining life and support families through grief. |
| Treatment Approach | May include curative treatments alongside symptom management. | Focuses on symptom management and comfort, with a primary goal of minimizing suffering. |
| Duration | Variable, depending on the individual’s condition and needs. | Typically for individuals with a life expectancy of six months or less. |
Pain Management and Symptom Control
Managing pain and symptoms effectively is crucial for both comfort care and hospice care, aiming to enhance the patient’s quality of life. A personalized approach is essential, considering the patient’s specific needs, preferences, and overall condition. This involves a multifaceted strategy encompassing various pharmacological and non-pharmacological interventions.
Pain Management in Comfort Care
Comfort care focuses on providing relief from distressing symptoms and maximizing comfort for patients with serious illnesses. Pain management in this setting emphasizes a proactive and individualized strategy, starting with non-pharmacological approaches and escalating to pharmacological interventions as needed. Early identification and intervention are key to preventing pain from escalating and impacting the patient’s well-being.
Pain Management in Hospice Care, Comfort care vs hospice
Hospice care, designed for patients with a life expectancy of six months or less, prioritizes symptom control and maintaining the patient’s comfort. Pain management is integral to the hospice philosophy, aiming to minimize discomfort and enhance the patient’s quality of life during this final stage.
Comparison of Symptom Management Strategies
Comfort care and hospice care share a common goal of symptom management, but hospice care often involves a more intensive and specialized approach due to the patient’s anticipated trajectory. Both utilize a combination of pharmacological and non-pharmacological methods, with a focus on individualized strategies to meet the unique needs of each patient. For instance, a patient receiving comfort care might benefit from medication adjustments based on changing symptoms, whereas a hospice patient might require more frequent and specialized symptom management as their condition progresses.
Role of Palliative Care in Symptom Control
Palliative care plays a vital role in both comfort care and hospice care, providing expert guidance and support in symptom management. Palliative care professionals work collaboratively with the healthcare team to develop comprehensive pain and symptom management plans, incorporating both pharmacological and non-pharmacological interventions. They offer expertise in pain assessment, medication titration, and the management of complex symptoms.
Specific Medications and Techniques
Various medications, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and adjuvant analgesics, are employed to manage pain. Non-pharmacological techniques, such as heat or cold therapy, massage, and guided imagery, are often incorporated into the overall pain management strategy. Specific techniques and medication choices are tailored to the individual patient’s response and needs. For example, a patient experiencing neuropathic pain might benefit from specific antidepressants or anticonvulsants.
Table of Pain Management Strategies
| Approach | Comfort Care | Hospice Care |
|---|---|---|
| Pharmacological Interventions | Utilize a range of medications, including NSAIDs, opioids, and adjuvant analgesics, to manage pain. | Emphasize the use of strong opioids and adjuvant medications to control severe pain, often with a focus on preventing breakthrough pain. |
| Non-Pharmacological Interventions | Employ techniques like relaxation exercises, massage, and heat/cold therapy to complement pharmacological treatments. | Utilize a wider range of non-pharmacological interventions, including acupuncture, music therapy, and guided imagery, to provide holistic comfort. |
| Pain Assessment | Regular assessment of pain intensity and impact on daily life. | Frequent and comprehensive pain assessment, including behavioral observations, to track changes and adjust treatments. |
| Symptom Management Approach | Proactive symptom management, aiming to prevent escalation of pain. | Focus on symptom control, addressing multiple symptoms concurrently, as the patient’s condition progresses. |
Family Involvement and Support
Families play a crucial role in the comfort and well-being of their loved ones facing serious illness, especially when navigating the complexities of comfort care and hospice. Understanding the unique roles and responsibilities of families in both settings, as well as the available support systems, is vital for ensuring the best possible quality of life for everyone involved. This section delves into the importance of family participation, emphasizing communication and support.
The Role of Families in Comfort Care
Families are integral to comfort care, providing emotional support and assisting with daily tasks. Their input is invaluable in understanding the patient’s preferences and ensuring that care aligns with their wishes. Comfort care focuses on alleviating suffering and enhancing quality of life, and families are essential partners in this process. They often become actively involved in decision-making regarding the patient’s care plan, and their insights are used to tailor the care to meet the specific needs of the individual.
The Role of Families in Hospice Care
Hospice care, unlike comfort care, is specifically designed for individuals facing a life-limiting illness with a prognosis of six months or less. Family involvement in hospice is not just important; it’s often central to the care plan. Families are actively encouraged to participate in every aspect of the patient’s care, from decision-making to emotional support. They are provided with resources and training to assist with the patient’s comfort and well-being.
The goal is not just to manage the patient’s symptoms but also to support the family through the emotional and practical challenges of the situation.
Support Systems for Families
Comprehensive support systems are crucial for families in both comfort care and hospice settings. These systems often include counselors, social workers, and spiritual advisors. They provide emotional support, practical guidance, and resources to assist families in navigating the challenges of the situation. These support systems are vital for the well-being of the entire family unit, ensuring they are equipped to cope with the emotional and practical demands of caring for a loved one.
Examples of Family-Centered Care
In comfort care, a family might participate in developing a personalized care plan that prioritizes the patient’s wishes and values. This might include specific dietary preferences, desired activities, and preferred communication methods. In hospice care, families often participate in grief counseling and support groups to prepare for the loss of their loved one. These programs can be instrumental in helping families process their emotions and cope with the difficult challenges ahead.
Importance of Communication
Clear and open communication between healthcare professionals and families is paramount in both comfort care and hospice. Honest discussions about the patient’s condition, prognosis, and treatment options are essential for informed decision-making. Regular updates and consistent communication channels are vital for maintaining trust and ensuring that everyone involved is on the same page. Active listening and empathy from healthcare professionals are crucial for understanding and addressing the unique needs of the family.
Family Involvement in Comfort Care and Hospice
| Activity | Comfort Care | Hospice Care |
|---|---|---|
| Decision-making | Families participate in developing care plans that reflect the patient’s wishes. | Families are active partners in decisions regarding the patient’s care and end-of-life choices. |
| Emotional Support | Families provide emotional support to the patient and each other. | Families receive support through grief counseling and support groups. |
| Practical Assistance | Families may assist with daily tasks and activities, like bathing or dressing. | Families receive support with practical tasks, such as arranging transportation and coordinating care. |
| Symptom Management | Families collaborate with healthcare professionals to manage symptoms like pain and discomfort. | Families are actively involved in symptom management, ensuring comfort and dignity. |
Ethical Considerations
Navigating the complexities of comfort care and hospice involves navigating a delicate landscape of ethical considerations. Decisions regarding end-of-life care are deeply personal, often involving family members, medical professionals, and spiritual advisors. These choices must be made with sensitivity and respect for the individual’s values and preferences, while also adhering to ethical principles.
Ethical Dilemmas in Comfort Care
Comfort care focuses on alleviating suffering and improving the quality of life for patients facing life-limiting illnesses. Ethical dilemmas often arise when decisions must be made regarding aggressive treatments versus prioritizing comfort. For instance, a patient may wish to continue aggressive treatments despite their potential to cause discomfort or hasten death, while family members may prefer comfort care to prioritize quality of life.
- Conflicting Goals: Disagreements may arise between the patient’s wishes and those of family members. These conflicts highlight the importance of open communication and shared decision-making. For example, a patient might desire aggressive treatment, but the family might feel it is futile and prefer comfort care. Mediation and clear communication channels can help resolve these disputes.
- Resource Allocation: Limited resources in healthcare settings can lead to difficult decisions about the allocation of medical care. Ethical principles, such as beneficence and justice, should guide these choices. For instance, if a hospital has limited beds or resources, it must decide which patients receive the highest priority, balancing the need for quality care with the limitations of resources.
- Unforeseen Circumstances: Unexpected events or changes in a patient’s condition can create ethical challenges. A patient’s preferences may not always align with their current situation, requiring a reevaluation of care plans. For example, a patient might initially desire aggressive treatment, but as their condition deteriorates, their preferences might shift. Adapting the care plan while respecting the patient’s evolving needs is crucial.
Ethical Dilemmas in Hospice Care
Hospice care prioritizes comfort and quality of life for patients nearing the end of life. Ethical dilemmas in hospice care can revolve around decisions about withholding or withdrawing life-sustaining treatments, managing pain and symptom control, and ensuring patient dignity.
Figuring out comfort care versus hospice can be tricky, especially when dealing with serious health conditions. While comfort care focuses on relieving symptoms and improving quality of life, hospice is a specialized form of care for those with a life expectancy of six months or less. Understanding how much creatine per day how much creatine per day might be beneficial for someone, though, is a completely separate matter and shouldn’t be confused with end-of-life care decisions.
Ultimately, the choice between comfort care and hospice depends on individual needs and preferences.
- Withholding/Withdrawing Treatment: Ethical considerations arise when decisions are made to withhold or withdraw life-sustaining treatments, such as feeding tubes or ventilators, in order to maintain comfort and dignity. These decisions must be made with the patient’s wishes and values in mind, as well as considering the family’s emotional needs. For instance, a patient might decline a feeding tube, while the family might have different preferences.
Clear documentation and communication are essential in such circumstances.
- Pain Management: Ensuring adequate pain management is a fundamental ethical principle in hospice care. However, managing pain in a way that does not hasten death can be challenging. Balancing the patient’s need for pain relief with the potential for accelerated death requires careful consideration. For example, using strong opioid analgesics may potentially hasten death, while withholding them can cause severe suffering.
- Patient Autonomy and Advance Directives: Patients have the right to make their own decisions about their care. Advance directives, such as living wills or durable powers of attorney, play a crucial role in guiding decisions about comfort care and hospice. However, interpreting these directives in complex situations can present ethical challenges. For example, a patient’s advance directive may not address a specific situation, necessitating careful consideration and consultation with legal and ethical experts.
Ethical Principles Guiding Decisions
Decisions about comfort care and hospice care should be guided by ethical principles, such as beneficence (acting in the best interest of the patient), non-maleficence (avoiding harm), respect for autonomy, and justice. These principles provide a framework for making difficult decisions and ensuring that care aligns with the patient’s values and preferences.
Figuring out comfort care versus hospice can be tough, but it’s all about what’s best for the patient. One important aspect of comfort care, especially as it relates to the end-of-life journey, is maintaining activity levels. Knowing how many calories you burn while walking can help you and your loved ones stay active and maintain a healthy lifestyle.
This is especially important in the context of comfort care, where maintaining a degree of mobility can significantly improve a patient’s quality of life, while exploring options like how many calories does walking burn can be a valuable tool in supporting this. Ultimately, the decision between comfort care and hospice depends on individual needs and goals.
Importance of Patient Autonomy and Shared Decision-Making
Patient autonomy is paramount in end-of-life care. Patients have the right to make informed decisions about their care, even if those decisions differ from the recommendations of medical professionals or family members. Shared decision-making involves actively engaging the patient in the decision-making process, fostering open communication, and ensuring the patient feels heard and respected. This process respects the patient’s values and preferences while ensuring everyone involved feels understood.
Cultural and Religious Influences
Cultural and religious beliefs significantly influence decisions about comfort care and hospice care. Different cultures and religions have varying perspectives on death, dying, and the use of medical interventions. Healthcare providers must be sensitive to these differences and provide culturally competent care. For example, some cultures may emphasize family involvement in decision-making, while others may place a greater emphasis on individual autonomy.
Understanding these variations is essential to ensure that care aligns with the patient’s values and preferences.
Cost Considerations and Insurance Coverage
Navigating the financial landscape of comfort care and hospice care can be daunting for families facing a serious illness. Understanding the associated costs and how insurance might cover them is crucial for making informed decisions. Knowing the potential financial burdens empowers families to plan ahead and explore available resources.
Costs Associated with Comfort Care
Comfort care, often provided within a hospital or nursing home setting, involves managing symptoms and improving quality of life for individuals with serious illnesses. Costs for comfort care vary greatly depending on the level of care needed. These costs typically include physician visits, medication, medical supplies, and nursing services. The duration of care also directly impacts the overall cost.
For example, frequent hospitalizations or specialized equipment rentals can significantly increase the financial burden.
Costs Associated with Hospice Care
Hospice care, focusing on comfort and supportive care for individuals with a life-limiting illness, often involves a range of services. Hospice care is generally more structured than comfort care, with a team of professionals like nurses, social workers, and counselors. Medicare and other insurance often cover hospice care, reducing the financial burden on patients and families. Costs include medical supplies, medications, and the services of hospice staff.
It’s important to note that the costs for hospice care can vary based on the type of services needed.
Insurance Coverage for Comfort Care and Hospice Care
Insurance coverage for comfort care and hospice care can differ significantly. Medicare, for example, usually covers comfort care services, but coverage may depend on the specific situation and the type of care provided. Medicare often covers a significant portion of hospice care costs, making it a valuable resource for those eligible. Private insurance plans also vary widely in their coverage of both comfort care and hospice care.
It’s essential to review your policy details and contact your insurance provider to understand the specific benefits and limitations.
Financial Assistance Programs
Several financial assistance programs are available to help families with the costs of comfort care and hospice care. These programs can provide financial aid to cover medications, medical supplies, and other related expenses. Local social service agencies, non-profit organizations, and government programs often offer support to those facing financial hardships. Organizations such as the National Hospice and Palliative Care Organization and the American Cancer Society offer resources to locate these programs.
Comparison of Care Costs in Different Settings
| Setting | Comfort Care (Estimated) | Hospice Care (Estimated) |
|---|---|---|
| Home | $500-$1500 per week | $100-$500 per week (Medicare-covered services) |
| Hospital | $1500-$5000+ per week | $100-$500 per week (Medicare-covered services) |
| Nursing Home | $2000-$8000+ per week | $100-$500 per week (Medicare-covered services) |
Note: These are estimated costs and can vary significantly depending on the specific needs of the individual, the level of care required, and the location. It’s crucial to consult with healthcare providers and insurance companies for personalized cost estimates.
Differences in Setting and Location
Comfort care and hospice care, while both focused on easing the end-of-life experience, differ significantly in their settings and locations. Understanding these differences is crucial for families navigating these difficult decisions. The availability and accessibility of care vary considerably depending on the chosen path.Comfort care is tailored to the patient’s needs and can be provided in various locations.
Hospice care, on the other hand, is specifically designed for patients with a limited life expectancy and often takes place in a designated hospice setting.
Comfort Care Settings
Comfort care is highly adaptable, allowing patients to receive care in the environment that best suits their needs and preferences. This flexibility can significantly improve the quality of life for the patient.
- Home: Many patients prefer to spend their final days surrounded by family and familiar comforts. At-home comfort care allows for personalized care, integrating with the patient’s existing support system.
- Nursing Homes/Assisted Living Facilities: Patients residing in these facilities often benefit from readily available medical staff and support services. Comfort care in these settings integrates seamlessly with the existing care plan, minimizing disruption for the patient and family.
- Hospitals: In situations where a patient requires intensive medical attention, comfort care can be provided within the hospital setting. This allows for immediate access to specialized medical equipment and personnel while focusing on symptom management and pain relief.
- Palliative Care Units: Dedicated palliative care units within hospitals provide a specialized environment for comfort care. These units often house interdisciplinary teams equipped to address the physical, emotional, and spiritual needs of patients.
Hospice Care Settings
Hospice care is structured to provide specialized care and support for individuals facing a life-limiting illness. The setting is crucial for ensuring the patient’s comfort and dignity during this challenging time.
- Hospice Facilities: Dedicated hospice facilities offer a supportive environment specifically designed for end-of-life care. These facilities often provide a comfortable and familiar space for patients and their families.
- Home: A significant portion of hospice care is delivered in the patient’s home. This allows patients to remain in a familiar environment, surrounded by loved ones.
- Nursing Homes/Assisted Living Facilities: Hospice care can also be provided in nursing homes or assisted living facilities. This option offers convenience and seamless integration with existing care routines.
- Hospitals: In certain cases, hospice care can be provided within a hospital setting. This is often the case when the patient requires continuous medical intervention while receiving hospice services.
Comparison of Services Across Locations
The availability of services can differ depending on the location where comfort care or hospice care is provided.
| Service | Home | Hospice Facility | Nursing Home | Hospital |
|---|---|---|---|---|
| Pain Management | Highly customizable; potentially fewer resources | Specialized pain management teams | Integrated with existing nursing staff | Immediate access to advanced pain management protocols |
| Symptom Control | Depending on resources, potential for delayed response | Dedicated symptom management teams | Integrated with existing care | Advanced symptom control protocols and equipment |
| Emotional Support | Relies on family and community resources | Dedicated social workers and counselors | Existing support services | Access to various support resources |
| Spiritual Support | Relies on personal networks | Chaplains and spiritual advisors | Potential access to pastoral care | Spiritual advisors available in many facilities |
Accessibility of Care
Accessibility of comfort care and hospice care varies based on location and individual circumstances.
- Geographic Location: Rural areas might face challenges in accessing specialized hospice care or comfort care facilities.
- Financial Constraints: Insurance coverage plays a crucial role in determining accessibility. Certain services might not be affordable for some families without adequate insurance.
- Patient Preferences: The patient’s personal preference for a specific care setting or comfort level significantly impacts the accessibility of care.
Transitioning Between Comfort Care and Hospice
Navigating the path from comfort care to hospice care can be a delicate and emotional process for both patients and families. Understanding the criteria, procedures, and support systems available is crucial for making informed decisions during this time. The goal is to ensure the patient’s comfort and dignity while honoring their wishes and the family’s emotional needs.
Criteria for Transition
Transitioning from comfort care to hospice care often hinges on a shift in the patient’s prognosis. Comfort care focuses on managing symptoms and improving quality of life, while hospice care focuses on providing comfort and support during the final stages of a terminal illness. This shift signifies a change in the expected course of the illness, moving towards a focus on end-of-life care.
Key indicators of a potential transition include a documented decline in the patient’s overall condition, a clear understanding of a limited life expectancy, and the need for more specialized care beyond comfort care’s scope. The patient’s physician, often in consultation with a hospice care team, plays a vital role in assessing the need for a transition.
Process for Transitioning
The transition from comfort care to hospice care involves a collaborative effort between the patient, family, and medical professionals. A key step is the formal referral to hospice services. This process typically begins with a conversation between the patient’s physician and a hospice care team. The hospice team will conduct an assessment of the patient’s needs, preferences, and the family’s support system.
Discussions about the patient’s goals for care, pain management strategies, and emotional support needs are crucial during this process. After the assessment, a plan of care is developed and implemented, ensuring a smooth transition for the patient and family.
Examples of Transitions
A patient with advanced cancer experiencing increasing pain and shortness of breath, despite comfort care measures, might transition to hospice care. Similarly, a patient with a progressive neurological condition who requires escalating levels of care and is expected to live for a limited time might transition to hospice. In these cases, the shift from comfort care to hospice care reflects the changing needs of the patient and the recognition that curative treatment is no longer the primary focus.
The focus shifts to maximizing comfort and providing support for the patient and family during the final stages of life.
Emotional and Practical Considerations
The transition between comfort care and hospice care often involves complex emotional and practical considerations for families and patients. The patient might experience anxieties related to the changing focus of care and the acceptance of their condition. Families may grapple with grief and uncertainty about the future. Open communication and support from the healthcare team are crucial.
The hospice team can provide emotional support, guidance, and practical assistance to the family, helping them navigate the practical aspects of end-of-life care, such as managing medications, coordinating appointments, and accessing resources. Hospice care also offers bereavement services to support families after the patient’s passing.
Closing Notes
In conclusion, the choice between comfort care and hospice is deeply personal and should be made in consultation with medical professionals and loved ones. This discussion underscores the importance of open communication, informed decision-making, and a comprehensive understanding of the available resources. Ultimately, the goal is to ensure the best possible quality of life for the patient and support for their family during this challenging time.