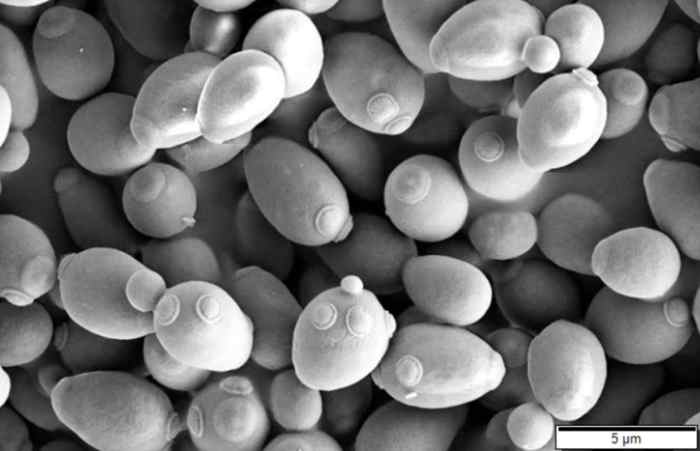
Yeast infections causes and risk factors are crucial to understand for women’s health. This comprehensive guide delves into the various types of yeast infections, their common symptoms, and the underlying causes that contribute to their development. We’ll explore the role of hormonal changes, antibiotic use, and lifestyle choices in increasing susceptibility to these infections. Additionally,…
Category: Women’s Health
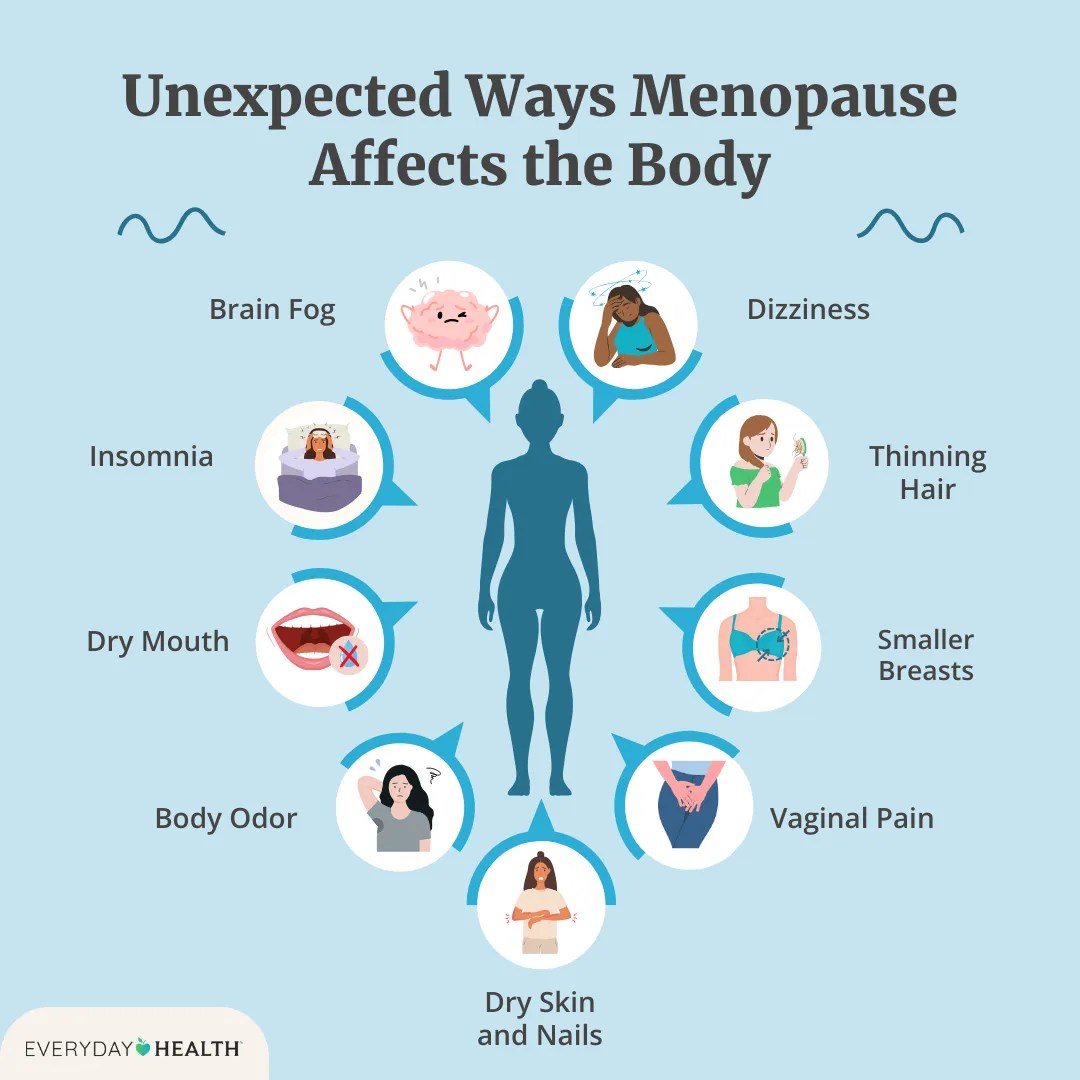
Menopause and Joint Pain Understanding the Connection
Menopause and joint pain often go hand-in-hand, creating a complex interplay of symptoms and underlying mechanisms. This exploration delves into the physiological changes during menopause that can affect joints, examining the types of pain experienced, and exploring the connection between hormonal fluctuations and discomfort. We’ll also look at diagnosis, treatment strategies, and crucial lifestyle recommendations…
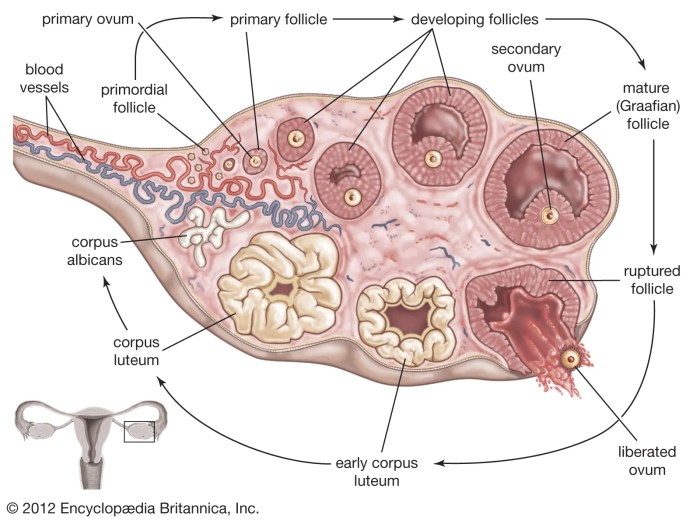
Things to Know About Your Ovaries and Ovulation
Things to know about your ovaries and ovulation: Dive deep into the fascinating world of female reproductive health. This comprehensive guide explores the intricate workings of your ovaries, the crucial ovulation process, and the overall menstrual cycle. From understanding ovarian anatomy to recognizing potential health concerns and fertility, you’ll gain valuable insights into your body’s…
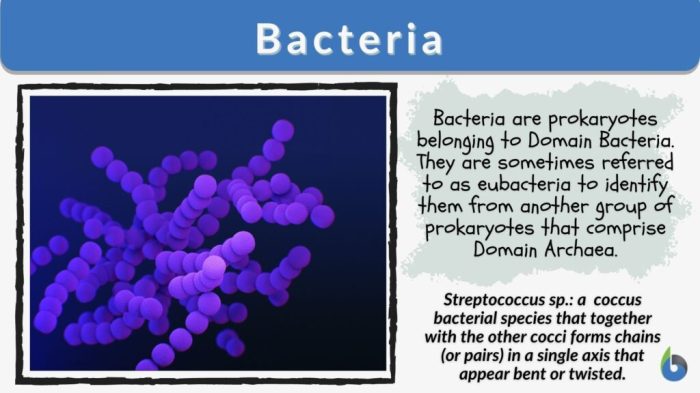
Bacterial Vaginosis Keeps Coming Back Understanding Recurrence
Bacterial vaginosis keeps coming back, frustrating many women. This recurring infection can be challenging to manage, impacting quality of life. This blog post delves into the reasons behind these recurring episodes, exploring everything from lifestyle factors to potential underlying health conditions. We’ll also look at diagnostic considerations, treatment strategies, and preventive measures you can take…
Does the Pill Work for PMDD Treatment?
Does the pill work as a PMDD treatment? This in-depth exploration delves into the complex relationship between hormonal birth control and Premenstrual Dysphoric Disorder (PMDD). We’ll examine the science behind the pill, its potential benefits, and drawbacks, while also considering individual variability and alternative approaches. Understanding the intricacies of PMDD management is crucial for navigating…
High Blood Pressure and PCOS A Deep Dive
High blood pressure and PCOS: understanding the connection is crucial for women’s health. High blood pressure, or hypertension, is a condition where the force of blood against your artery walls is consistently too high. Polycystic ovary syndrome (PCOS) is a hormonal disorder that affects women of reproductive age, often leading to irregular periods, excess hair…
PCOS Diagnosis Delays Adult Years
How could I not know that I had PCOS until adulthood? This journey explores the often-delayed diagnosis of Polycystic Ovary Syndrome (PCOS) in women. We’ll delve into why diagnosis might be delayed, the impact of this delay on health outcomes, and strategies for improving early detection. Many women experience a range of symptoms, some subtle,…
Turmeric Health Benefits for Women A Deep Dive
Turmeric health benefits for women are plentiful and fascinating, offering a natural approach to overall well-being. From hormonal balance to digestive health, bone strength, skin radiance, and immune support, turmeric’s active compound, curcumin, appears to play a key role in various aspects of women’s health. This exploration delves into the science behind turmeric’s effects, highlighting…
Ovarian Pain Causes and Treatment Explained
Ovary pain causes and treatment – Ovarian pain causes and treatment is a complex issue affecting many women. Understanding the intricacies of the female reproductive system, the various potential causes of discomfort, and the available treatment options is crucial for effective management. This exploration delves into the different types of ovarian pain, their potential origins,…
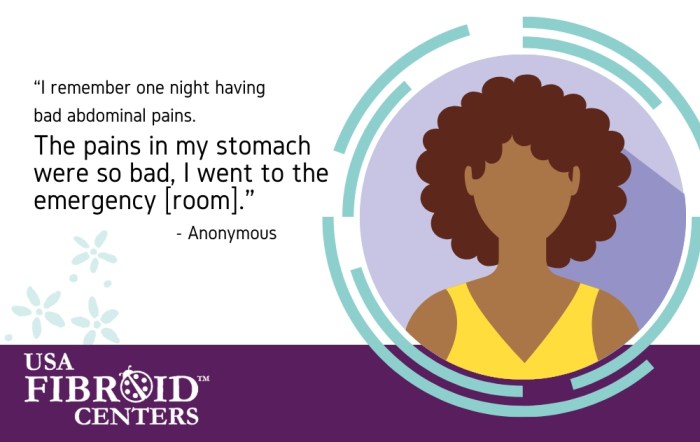
Nkem Osians Uterine Fibroid Story A Personal Account
Nkem osian uterine fibroid story – Nkem Osian’s uterine fibroid story is a powerful account of navigating a health challenge with resilience and grace. This journey delves into the personal experiences, medical treatments, and societal factors surrounding uterine fibroids. From understanding the condition itself to exploring the emotional and practical impacts, this narrative offers a…