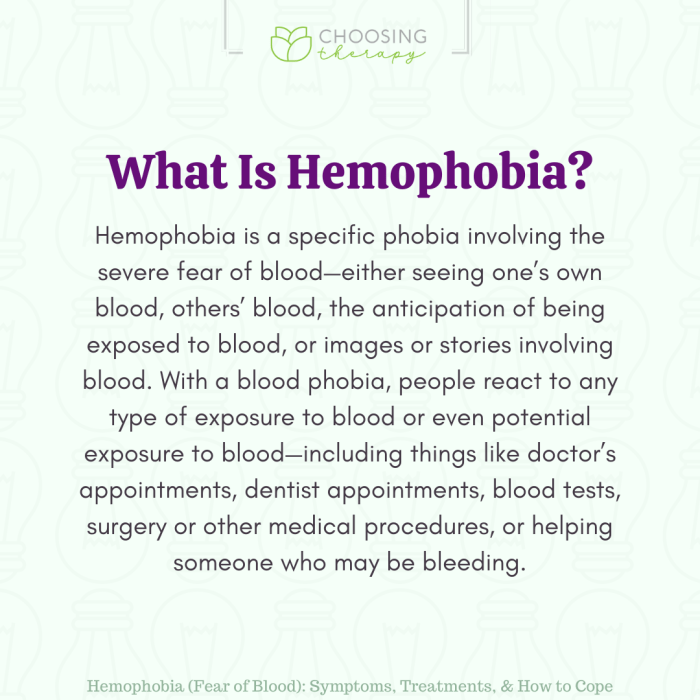
Hemophobia fear of blood – Hemophobia, fear of blood, is a specific phobia that can significantly impact a person’s life. This detailed exploration delves into the nuances of this condition, from its defining characteristics and symptoms to potential causes, effective treatments, and practical coping mechanisms. We’ll also examine the cultural and societal perspectives surrounding blood,…
Category: Mental Health
Signs of Depression in Men Hidden Struggles
Signs of depression in men often manifest differently than in women, leading to delayed recognition and treatment. Societal pressures and cultural norms frequently discourage men from seeking help, masking the underlying issue. This in-depth exploration delves into the various signs, from emotional and behavioral changes to subtle physical indicators. We’ll also discuss the challenges men…
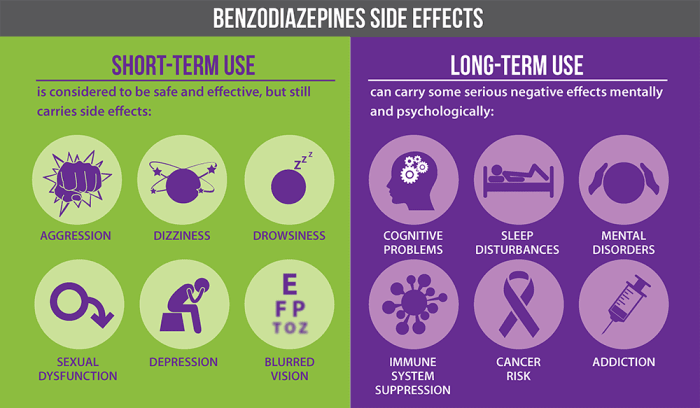
Benzodiazepines Uses, Types, and Risks
Uses types and risks of benzodiazepines – Benzodiazepines: Uses, Types, and Risks sets the stage for a detailed exploration of these medications. This in-depth look will cover everything from their chemical makeup and mechanism of action to their various applications, potential dangers, and long-term considerations. We’ll analyze different types, examining their potency, duration, and common…
Comparing Vyvanse vs Adderall A Deep Dive
Comparing Vyvanse vs Adderall: This comprehensive guide delves into the intricacies of these stimulant medications, exploring their chemical makeup, potential benefits and drawbacks, and patient experiences. We’ll examine the nuances of their formulations, their impact on various conditions, and provide a balanced overview for patients and healthcare providers alike. Both Vyvanse and Adderall are commonly…
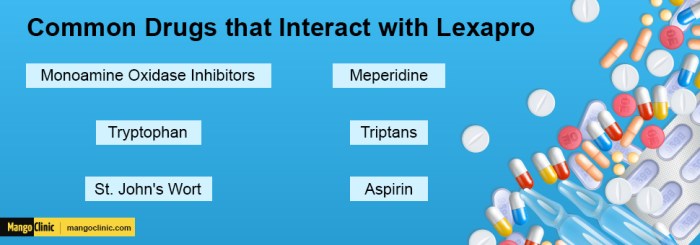
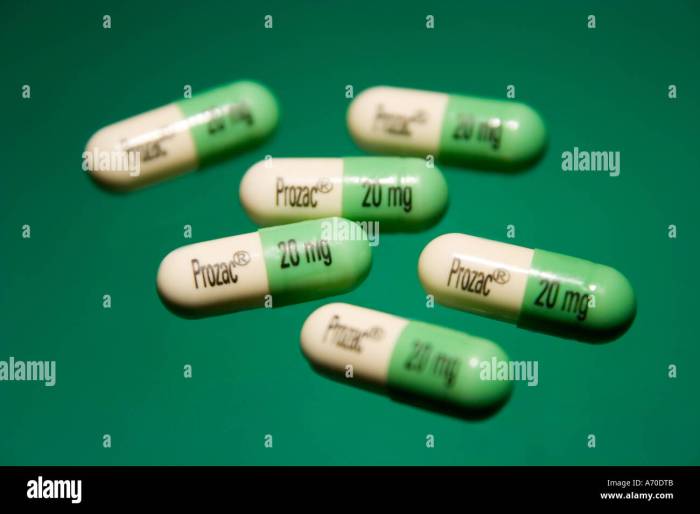
Prozac Fluoxetine vs Lexapro Escitalopram A Deep Dive
Prozac fluoxetine vs lexapro escitalopram: A comparison of these two popular antidepressants, both Selective Serotonin Reuptake Inhibitors (SSRIs), is crucial for individuals seeking effective treatment. This in-depth look examines their mechanisms of action, common side effects, dosage ranges, and potential interactions. Understanding the nuances between these drugs empowers informed decision-making with a healthcare professional. This…
Acute Trauma vs Chronic Trauma Understanding the Differences
Acute trauma vs chronic trauma: This exploration delves into the distinct impacts of sudden, intense experiences versus ongoing, pervasive stress. Understanding these differences is crucial for providing appropriate support and treatment. We’ll examine the physiological and psychological responses, the developmental effects, and the various treatment approaches. Acute trauma often stems from a single, shocking event…
Fear of People Anthropophobia Explained
Fear of people anthropophobia – Fear of people, anthropophobia, is a specific phobia characterized by an intense and persistent fear of other people. It’s different from general social anxiety, often focusing on a broad range of social situations rather than a specific fear of interaction. This fear can vary in severity, from mild discomfort to…
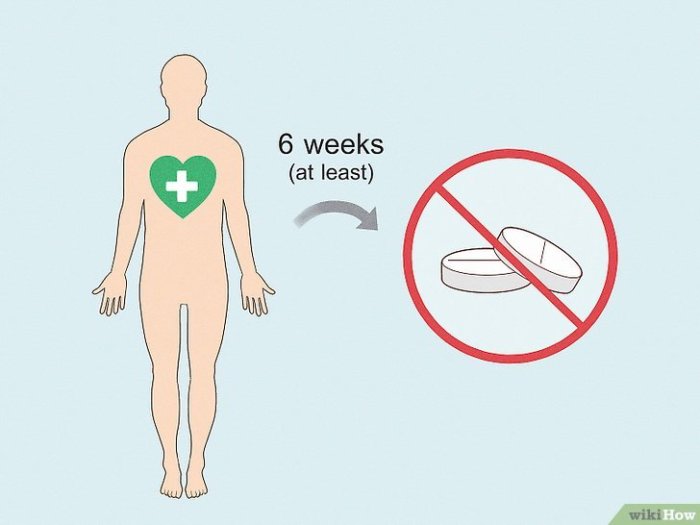
Taking Lexapro First Week Insights
Taking lexapro what to expect in the first week – Taking Lexapro: What to Expect in the First Week? This journey into the first week of Lexapro use delves into potential side effects, possible benefits, and crucial considerations. We’ll explore common symptoms, potential improvements, and vital precautions to navigate this initial phase effectively. Prepare for…
Prozac Fluoxetine vs Zoloft Sertraline A Deep Dive
Prozac fluoxetine vs Zoloft sertraline: A crucial comparison for understanding antidepressant options. These selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed, but their mechanisms, side effects, and efficacy can vary. This exploration dives deep into the specifics of each drug, highlighting key differences and offering insights for patients and healthcare providers alike. This detailed analysis…
Dysphoric Mood Warning Signs Coping Strategies
Dysphoric mood warning signs and how to cope is a crucial guide for understanding and managing emotional distress. This comprehensive resource delves into the nuances of dysphoric moods, from recognizing the initial signs to developing effective coping mechanisms and seeking professional help. We’ll explore various types of dysphoric moods, their triggers, and a range of…