Parasitic infections of the central nervous system are a significant global health concern. These infections, often insidious and diverse in their manifestations, can affect individuals worldwide. Understanding the various transmission routes, types of parasites involved, and the resulting pathologies is crucial for effective diagnosis and treatment.
This comprehensive exploration will delve into the complexities of parasitic CNS infections, examining their pathogenesis, symptoms, diagnostic methods, treatment strategies, and preventive measures. We’ll cover the diverse range of parasites causing these infections, from protozoa to helminths to arthropods, and analyze the geographical distribution of these diseases. The importance of multidisciplinary approaches to management will also be highlighted.
Introduction to Parasitic Infections of the Central Nervous System
Parasitic infections of the central nervous system (CNS) represent a significant global health concern, posing substantial risks to individuals’ neurological well-being. These infections, often overlooked or misdiagnosed, can lead to severe complications, including neurological dysfunction, disability, and even death. Understanding the various aspects of these infections is crucial for effective prevention, diagnosis, and treatment.These infections can manifest with a wide range of symptoms, from mild headaches and fever to more severe conditions like seizures, paralysis, and cognitive impairment.
Parasitic infections of the central nervous system can be seriously debilitating, impacting everything from movement to cognitive function. Fortunately, similar principles of targeted physical therapy, like those used in treating diastasis recti with physical therapy , can also be applied to rehabilitation after these infections. Recovering from such infections often involves a long and complex process, requiring a holistic approach to restoring both physical and mental well-being.
The insidious nature of some of these infections can lead to delays in diagnosis, thus emphasizing the need for heightened awareness and appropriate diagnostic tools.
Routes of Transmission
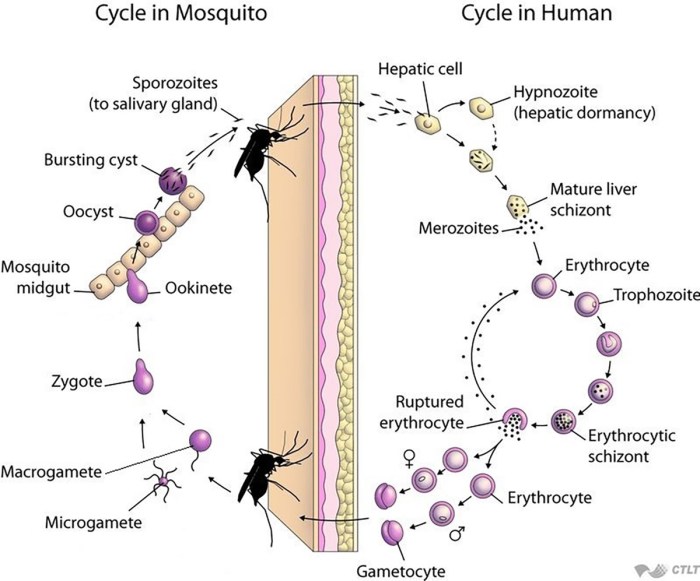
Various routes facilitate the transmission of parasitic infections to the CNS. Ingestion of contaminated food or water is a common mode of transmission, as certain parasites are present in contaminated environments. Vector-borne transmission, where parasites are carried by insects or other arthropods, is another important mechanism. Direct contact with infected individuals or animals can also lead to infection.
Types of Parasites Causing CNS Infections
A diverse array of parasites can invade the CNS, each with its unique life cycle and clinical presentation. Protozoa, helminths, and arthropods are among the primary culprits. The specific parasite involved often dictates the clinical picture and treatment approach.
Classification of CNS Parasitic Infections
| Category | Examples | Description |
|---|---|---|
| Protozoa | Toxoplasma gondii, Naegleria fowleri, Cryptosporidium | These single-celled organisms can cause meningitis, encephalitis, and other CNS disorders. Toxoplasma gondii, for example, is a common cause of CNS infection in immunocompromised individuals and can have devastating effects on the developing fetus. |
| Helminths | Schistosoma spp., Echinococcus spp., Cysticercus | These parasitic worms can cause granulomatous inflammation and other tissue damage within the CNS. Cysticercus, a larval stage of the pork tapeworm, is a significant cause of neurocysticercosis, a devastating infection that can lead to seizures, headaches, and other neurological complications. |
| Arthropods | Babesia spp., Plasmodium spp., Borrelia burgdorferi (Lyme disease) | Some arthropods act as vectors, transmitting parasites to humans. Babesia, transmitted by ticks, can cause severe hemolytic anemia and CNS involvement. |
Geographical Distribution and Prevalence
The geographical distribution of CNS parasitic infections varies considerably, reflecting factors like climate, sanitation, and human behavior. Regions with poor sanitation and inadequate access to clean water frequently experience higher prevalence rates of certain infections. Areas with high vector populations, such as tropical and subtropical regions, are often associated with higher rates of vector-borne parasitic infections.
| Parasite | High Prevalence Regions | Explanation |
|---|---|---|
| Toxoplasma gondii | Developing countries, particularly in regions with poor hygiene practices | The parasite is widespread, with transmission often linked to contaminated food and animal contact. |
| Cysticercus | Areas with high rates of pork consumption and poor hygiene practices | The pork tapeworm is prevalent in regions where pork is consumed without adequate cooking. |
| Naegleria fowleri | Warm freshwater bodies in various regions | This amoeba thrives in warm waters, posing a risk to those who swim or engage in water activities in contaminated environments. |
Pathogenesis and Symptoms
Parasitic infections of the central nervous system (CNS) represent a significant global health concern, impacting individuals across various demographics. These infections, often insidious in their onset, can lead to devastating neurological consequences if left untreated. Understanding the intricate mechanisms by which parasites invade and affect the CNS, along with the diverse clinical presentations, is crucial for effective diagnosis and management.The pathogenesis of CNS parasitic infections is multifaceted, involving the parasite’s ability to traverse host defenses, establish a foothold within the CNS, and elicit an inflammatory response.
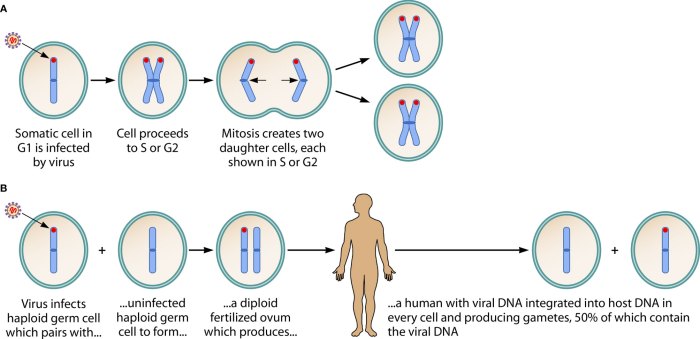
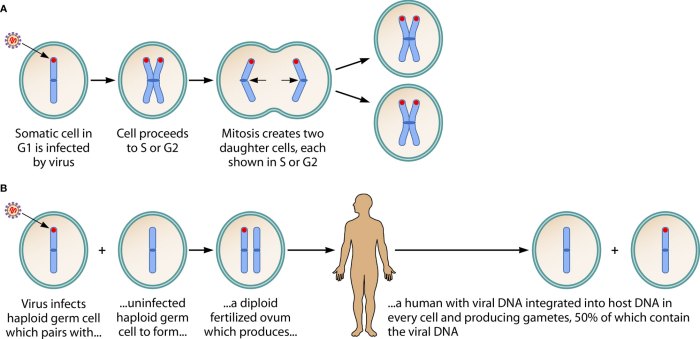
Different parasitic species utilize distinct strategies to achieve these goals. Some parasites directly invade the CNS through the bloodstream, while others may exploit the host’s immune system vulnerabilities or travel along neural pathways.
Mechanisms of CNS Invasion
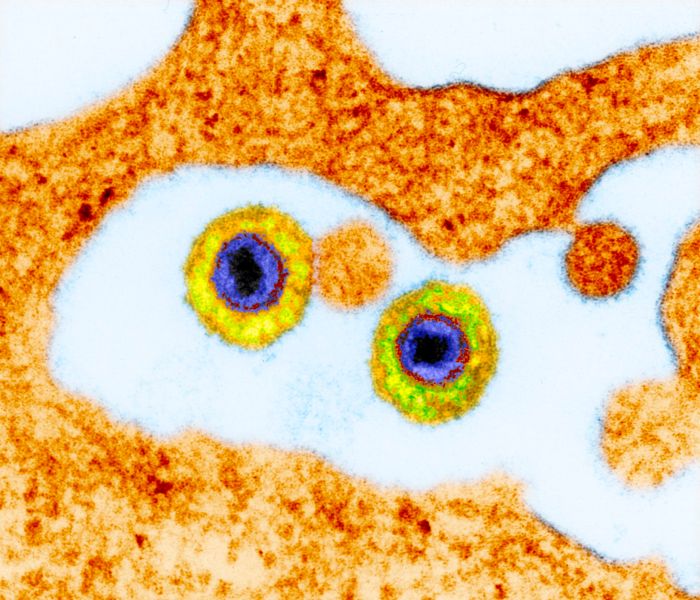
Parasites employ various strategies to gain access to and establish themselves within the CNS. Blood-borne dissemination is a common mechanism, where parasites circulate in the bloodstream and then cross the blood-brain barrier (BBB). This barrier, normally highly selective, can be compromised by inflammation or direct damage, allowing parasites to enter the brain parenchyma. Other routes of invasion include neural pathways, where parasites might migrate along nerve fibers, or by penetrating the meninges, the protective membranes surrounding the brain and spinal cord.
Stages of Parasitic Infection in the CNS
The progression of CNS parasitic infection typically involves distinct stages. The initial stage often involves the parasite’s entry into the bloodstream or the CNS. This is followed by multiplication and dissemination within the host. Subsequent stages encompass the development of a localized or systemic inflammatory response, which can result in tissue damage and neurological dysfunction. The duration and severity of each stage can vary significantly depending on the parasite species and the host’s immune response.
Clinical Presentations
The clinical presentations of CNS parasitic infections are highly variable, ranging from mild, nonspecific symptoms to severe, life-threatening neurological complications. Factors like the specific parasite species, the intensity of the infection, and the host’s immune status all contribute to the clinical spectrum. These infections can manifest with headache, fever, seizures, altered mental status, focal neurological deficits, and meningitis-like symptoms.
Diagnosis often requires a thorough understanding of the patient’s travel history, recent exposure to potential vectors, and epidemiological data in the region.
Parasitic infections of the central nervous system can be seriously debilitating. Understanding the complexities of these infections is crucial, and sometimes, treatment strategies for other neurological conditions can offer surprising parallels. For instance, comparing the similar yet distinct mechanisms of naloxone and naltrexone in their application for opioid overdose reversal versus long-term opioid dependence treatment can provide insights into managing these types of neurological disorders.
You can delve deeper into the specifics of naloxone vs naltrexone similarities and differences to appreciate the nuanced ways these medications work. Ultimately, a comprehensive approach to treating parasitic infections of the central nervous system, leveraging all available knowledge, is essential for effective patient care.
Neurological Manifestations
The neurological manifestations associated with CNS parasitic infections can be highly diverse. These manifestations depend on the specific parasite, the location of the infection within the CNS, and the host’s immune response. For instance, a cerebral abscess, caused by certain parasites, may present with focal neurological deficits like hemiparesis (weakness on one side of the body) or aphasia (language disturbance).
Similarly, meningitis-like symptoms, such as stiff neck, fever, and headache, are common in several parasitic infections. The presence of seizures, altered mental status, or cranial nerve palsies further contribute to the complex clinical picture.
Comparative Symptoms of CNS Parasitic Infections
| Parasite | Common Symptoms | Neurological Manifestations |
|---|---|---|
| Toxoplasma gondii | Headache, fever, malaise, seizures, focal neurological deficits, encephalitis | Focal deficits, cognitive impairment, hydrocephalus |
| Naegleria fowleri | Severe headache, fever, stiff neck, nausea, vomiting, altered mental status, seizures | Meningoencephalitis, rapid deterioration of neurological function |
| Cysticercus cellulosae | Headache, seizures, focal neurological deficits, intracranial hypertension | Hydrocephalus, intracranial mass lesions, seizures |
Note: This table provides a simplified overview. Specific symptoms and manifestations can vary depending on the individual and the stage of infection. Further diagnostic testing is essential for accurate identification and treatment.
Diagnostic Methods
Unraveling the mystery of parasitic infections affecting the central nervous system (CNS) hinges on accurate and timely diagnosis. Precise identification allows for appropriate treatment strategies and improves patient outcomes. A multi-faceted approach involving various diagnostic tools is crucial for accurate diagnosis, moving beyond a single test.Diagnostic strategies for CNS parasitic infections require a systematic approach, integrating clinical evaluation, laboratory investigations, and imaging techniques.
This comprehensive strategy helps differentiate between different parasitic entities and other possible neurological conditions. The interplay of these methods increases the probability of a correct diagnosis and facilitates targeted treatment plans.
Imaging Techniques
Imaging plays a vital role in visualizing the CNS and identifying potential parasitic lesions. Different imaging modalities offer varying levels of detail and sensitivity.
Parasitic infections of the central nervous system can be incredibly devastating, often leading to severe neurological problems. While seemingly unrelated, understanding conditions like hemophilia disease what is hemophilia disease can offer valuable insights into the broader spectrum of blood disorders and their impact on the body. Ultimately, though, focusing on parasitic infections of the nervous system reveals how these tiny invaders can wreak havoc on the delicate balance of our brains and spinal cords.
- Computed Tomography (CT) Scan: CT scans are valuable for detecting abnormalities in brain structure, including masses, calcifications, and edema. They provide rapid visualization of the brain, enabling quick assessment of potential intracranial pathology. However, CT scans may not always distinguish between different types of parasitic infections. For instance, a lesion indicative of cysticercosis might appear similar to other inflammatory conditions.
- Magnetic Resonance Imaging (MRI): MRI offers superior soft tissue contrast compared to CT, enabling more detailed visualization of CNS structures and lesions. MRI is particularly useful in identifying the extent of parasitic involvement and characterizing the lesions. For example, MRI can differentiate between the cystic appearance of neurocysticercosis and the solid appearance of toxoplasmosis. The high cost and longer acquisition time are limitations of this procedure.
- Magnetic Resonance Angiography (MRA): MRA provides detailed images of blood vessels in the brain, allowing for the identification of vascular anomalies associated with certain parasitic infections. This technique is particularly helpful in cases of vascular invasion by parasites, where blood vessel abnormalities are evident.
Cerebrospinal Fluid (CSF) Analysis
Cerebrospinal fluid (CSF) analysis is a critical diagnostic tool for identifying CNS parasitic infections. CSF contains diagnostic information about the central nervous system’s inflammatory state.
- CSF Collection Procedure: CSF is collected via a lumbar puncture (spinal tap), a procedure performed by a trained medical professional. The procedure involves inserting a needle into the lower back to access the subarachnoid space and collect CSF. Proper sterile technique is essential to prevent infection. The patient is typically positioned lying on their side with their knees drawn up towards their chest.
- CSF Analysis: Analysis of CSF involves several tests, including cell counts (white blood cell count), protein levels, glucose levels, and microscopic examination. Elevated white blood cell counts, protein levels, and abnormal glucose levels may indicate an inflammatory process. Microscopic examination of CSF sediment allows for direct visualization of parasites, eggs, or other characteristic features.
Microscopic Examination of Specimens
Microscopic examination of various specimens is a cornerstone of parasitic identification. Direct observation under a microscope can reveal crucial morphological characteristics of the parasite.
- Tissue Samples: Tissue biopsies, obtained from a suspected lesion, can be examined microscopically to identify parasites. Parasites may be present in tissue sections, allowing for their detailed morphological study.
- CSF Examination: Microscopic examination of CSF sediment allows for direct visualization of parasites, eggs, or other characteristic features. This direct visualization is crucial in the initial identification and subsequent classification of the parasite.
- Blood Samples: In certain cases, microscopic examination of blood samples can help identify circulating parasites or their components. These may be indicative of the parasitic load in the body and the extent of the infection.
Limitations of Diagnostic Methods
Diagnostic methods for CNS parasitic infections have inherent limitations. These limitations should be considered when interpreting results and designing diagnostic strategies.
- Sensitivity and Specificity: Not all diagnostic methods are equally sensitive and specific for detecting different parasitic infections. The sensitivity and specificity of each method can vary depending on the stage of infection, the parasite species, and the presence of other factors.
- Non-Specificity: Some findings on imaging or CSF analysis may be non-specific, suggesting a broad range of conditions, including infections. Differentiation among these conditions requires further investigation.
- Cost and Accessibility: Certain diagnostic methods, such as MRI, may be costly or less accessible in some settings. The choice of diagnostic method should consider the resources available.
Treatment Strategies
Treating parasitic infections of the central nervous system (CNS) requires a multifaceted approach, tailoring the strategy to the specific parasite, the extent of infection, and the patient’s overall health. The goal is to eliminate the parasite, manage symptoms, and prevent further complications. Success often hinges on early diagnosis and prompt, appropriate treatment.Effective treatment strategies for CNS parasitic infections vary considerably depending on the causative agent.
Some parasites respond well to specific medications, while others necessitate a more complex and prolonged treatment regimen. The choice of treatment often involves a careful evaluation of potential risks and benefits, taking into account factors such as the patient’s age, overall health, and the specific characteristics of the infection.
Available Treatment Options
Various antiparasitic drugs are employed to target the causative agents of CNS parasitic infections. These drugs can be broadly classified into different categories based on their mechanism of action. Some act by disrupting the parasite’s metabolic processes, others by inhibiting its reproduction, and some by directly killing the parasite. The choice of medication is often determined by the type of parasite and its susceptibility to particular drugs.
Effectiveness and Side Effects
The effectiveness of antiparasitic drugs varies depending on the parasite and the individual. Some drugs show high efficacy in eliminating the parasite, leading to a rapid resolution of symptoms. However, certain medications can induce adverse effects, ranging from mild gastrointestinal upset to more serious complications. It’s crucial to weigh the benefits of treatment against the potential risks and monitor patients closely for any signs of toxicity.
Factors Influencing Treatment Decisions, Parasitic infections of the central nervous system
Several factors influence the choice of treatment for CNS parasitic infections. The patient’s age, overall health, and the severity of the infection are key considerations. Pre-existing medical conditions, such as liver or kidney disease, can influence the selection of drugs and dosage. Furthermore, the specific location and extent of the infection within the CNS play a significant role in treatment decisions.
Genetic factors may also affect drug metabolism and response, thus requiring careful consideration.
Recommended Treatment Protocols
| Parasite | Treatment Protocol | Effectiveness | Potential Side Effects |
|---|---|---|---|
| Toxoplasma gondii | Combination therapy with pyrimethamine and sulfadiazine, potentially with leucovorin. | Generally effective, especially when initiated early. | Possible bone marrow suppression, nausea, rash. |
| Naegleria fowleri | Intravenous amphotericin B, sometimes with rifampin. | Limited efficacy; mortality rates remain high. | Nephrotoxicity, fever, and other serious adverse effects. |
| Cysticercus cellulosae | Anti-inflammatory medications, possibly albendazole. Surgical removal of cysts may be required. | Treatment efficacy varies depending on the extent of infection. | Possible allergic reactions to medications, surgical complications. |
Note: This table provides a simplified overview. Specific treatment protocols should be determined by healthcare professionals based on individual patient characteristics and disease presentation.
Multidisciplinary Approaches
Managing CNS parasitic infections requires a multidisciplinary approach, bringing together neurologists, infectious disease specialists, and other relevant healthcare professionals. This collaborative effort is crucial to ensure comprehensive patient care, addressing the neurological and infectious disease aspects of the condition. Early diagnosis, prompt treatment, and diligent monitoring are essential components of successful management. A team-based approach ensures that the patient receives a coordinated and holistic course of treatment, maximizing their chances of recovery.
Prevention and Control: Parasitic Infections Of The Central Nervous System
Preventing parasitic infections of the central nervous system (CNS) hinges on a multi-pronged approach targeting the life cycle of the parasites and the environments where they thrive. Effective prevention requires a comprehensive understanding of the specific parasite involved, its transmission routes, and the vulnerabilities of the human host. Successful control relies heavily on public health interventions, vector control, hygiene practices, and public education.Controlling the spread of these infections is not just about treating individual cases but also about creating a resilient community that actively participates in preventing transmission.
This involves a concerted effort from healthcare professionals, public health officials, and individuals to implement preventive measures and maintain a healthy environment.
Public Health Interventions
Public health initiatives play a critical role in managing the spread of CNS parasitic infections. These interventions often involve targeted campaigns focused on vulnerable populations and geographical areas. For instance, mass drug administration programs can significantly reduce parasite prevalence in endemic regions. Regular surveillance and monitoring of infection rates are essential for identifying emerging trends and adapting prevention strategies.
Effective communication channels are crucial for disseminating information about preventive measures and the importance of seeking timely medical attention.
Vector Control Measures
Vector control is paramount in preventing the transmission of many CNS parasitic infections. Vectors, such as mosquitoes and flies, act as intermediaries, carrying the parasites from one host to another. Effective vector control strategies include the use of insecticide-treated bed nets, the elimination of breeding grounds for vectors (like stagnant water), and the implementation of integrated pest management programs.
Targeted spraying of insecticides in affected areas can also significantly reduce vector populations. For instance, the successful control of malaria has been strongly linked to the widespread use of insecticide-treated bed nets.
Sanitation and Hygiene Practices
Maintaining proper sanitation and hygiene is fundamental to preventing parasitic infections. This involves ensuring access to clean water and sanitation facilities, promoting handwashing practices, and controlling the presence of contaminated food and water sources. Proper waste disposal and the management of animal waste are crucial to preventing the contamination of water sources and food. By adhering to these practices, individuals significantly reduce their risk of contracting parasitic infections.
For example, consistent handwashing after handling contaminated items can prevent the transmission of intestinal parasites, which sometimes affect the nervous system.
Education and Awareness Programs
Education and awareness programs play a vital role in promoting preventive measures and fostering community participation in infection control. These programs should focus on educating individuals about the various parasitic infections, their transmission routes, and the preventive measures that can be taken. This includes educating communities about the importance of handwashing, vector control strategies, and the proper disposal of waste.
For example, educational campaigns can promote the use of insecticide-treated bed nets and the elimination of stagnant water around homes, effectively reducing the risk of parasite transmission.
Case Studies and Examples
Delving into the realm of parasitic infections affecting the central nervous system (CNS) reveals a tapestry of complex clinical presentations, diagnostic hurdles, and treatment challenges. Understanding these intricacies through real-world case studies provides valuable insights into the diverse manifestations of these infections and guides clinicians in the development of appropriate management strategies. These case studies, while anonymized to protect patient privacy, illuminate the diagnostic process and highlight the importance of considering parasitic infections in the differential diagnosis of neurological symptoms.
Illustrative Case Studies
Parasitic infections of the CNS can present with a wide spectrum of neurological symptoms, making diagnosis difficult. A crucial aspect of successful management lies in recognizing the potential for these infections and applying a systematic diagnostic approach. This section presents illustrative case studies, highlighting variations in clinical presentations, diagnostic challenges, and treatment outcomes.
| Case Study | Presenting Symptoms | Diagnostic Findings | Treatment and Outcome |
|---|---|---|---|
| Case 1: Neurocysticercosis | Headache, seizures, focal neurological deficits | CT scan showing intracranial cysts, serologic testing for Taenia solium | Surgical removal of cysts, anti-parasitic medication (e.g., albendazole), supportive care. Favorable outcome with resolution of symptoms. |
| Case 2: African trypanosomiasis | Progressive neurological dysfunction, fever, headache | Blood smear showing trypomastigotes, serological tests confirming the diagnosis. | Specific anti-parasitic treatment (e.g., eflornithine or nifurtimox), supportive care. Outcome varied depending on the stage of infection and promptness of treatment. |
| Case 3: Toxoplasmosis | Subacute encephalitis, focal neurological deficits, fever | MRI showing brain lesions, serological tests for Toxoplasma gondii, PCR testing for parasite DNA. | Anti-parasitic medication (e.g., pyrimethamine, sulfadiazine), supportive care. Favorable outcome with appropriate treatment. |
Hypothetical Case Scenario
A 35-year-old male presents to the clinic with a 2-week history of progressive headache, fever, and worsening confusion. He reports a recent trip to a rural area in a tropical country. He denies any other significant medical history or recent trauma.
Diagnostic Workup and Management
Given the patient’s travel history and constellation of symptoms, a strong suspicion for a parasitic CNS infection exists. The diagnostic workup would include:
- Detailed travel history, including specific locations and duration.
- Complete blood count (CBC), blood cultures, and serological tests for various parasitic infections (e.g., malaria, trypanosomiasis, toxoplasmosis, and cysticercosis).
- Neuroimaging (e.g., CT scan or MRI) to assess for intracranial lesions or abnormalities.
- Lumbar puncture (LP) for cerebrospinal fluid (CSF) analysis, including cell counts, protein levels, and Gram stain.
- Molecular diagnostics, such as PCR, for confirmation of specific parasite presence in the CSF or other tissues if indicated.
Parasitic Infections Affecting Specific CNS Regions
Parasitic infections can target different regions of the CNS, leading to varying neurological presentations.
- Brain Abscesses: Certain parasites, such as Naegleria fowleri, can directly invade the brain parenchyma, leading to the formation of brain abscesses. This often presents with focal neurological deficits and severe headache. Prompt diagnosis and surgical intervention are crucial.
- Meningitis: Cysticercus cellulosae larvae can cause meningitis, manifesting with severe headache, fever, and neck stiffness. The diagnosis can be challenging due to the need to differentiate from other causes of meningitis.
- Cerebral Vasculitis: Parasitic infections can trigger inflammatory responses in the cerebral blood vessels, leading to vasculitis and potentially causing stroke or other neurological complications. The clinical presentation can mimic other neurological disorders.
Emerging Trends and Future Directions
Parasitic infections of the central nervous system (CNS) continue to pose a significant global health challenge, particularly in resource-limited settings. Understanding emerging trends, identifying knowledge gaps, and leveraging technological advancements are crucial for improving diagnosis, treatment, and prevention strategies. The ongoing evolution of these infections demands a proactive approach to research and development.
Epidemiology of CNS Parasitic Infections
The epidemiology of CNS parasitic infections is dynamic and influenced by various factors, including climate change, migration patterns, and socioeconomic conditions. Increased travel and globalization contribute to the spread of parasites across geographical boundaries. Emerging trends highlight a rise in infections in previously unaffected regions and a shift in the predominant parasite species affecting specific populations. This underscores the need for ongoing surveillance and epidemiological studies to understand the changing landscape of these infections.
Research and Development Needs
Several areas require further research and development to combat CNS parasitic infections effectively. These include improving diagnostic tools, developing novel and more effective treatments, and understanding the complex interactions between parasites and the host immune system. Improved diagnostic methods, particularly for early detection, are essential for timely intervention and reducing the severity of neurological complications. Furthermore, research into the mechanisms of parasite invasion and immune evasion is critical for developing more effective and targeted therapies.
Role of New Technologies
Technological advancements are revolutionizing the diagnosis and treatment of CNS parasitic infections. Molecular diagnostics, such as polymerase chain reaction (PCR), offer highly sensitive and specific detection of parasitic DNA or RNA, allowing for rapid and accurate identification of the causative agent. Furthermore, advancements in imaging techniques, like magnetic resonance imaging (MRI) and advanced computed tomography (CT), provide detailed visualization of brain lesions associated with parasitic infections.
These technologies can aid in precise diagnosis and guide treatment strategies.
Developing Effective and Accessible Treatments
The current treatment options for CNS parasitic infections often have limitations, including toxicity, side effects, and limited efficacy. Developing more effective and accessible treatments is a high priority. This necessitates research into new drug targets, exploring alternative treatment approaches, and optimizing existing treatments for improved efficacy and safety. The development of affordable and readily available drugs is critical for treating infections in resource-limited settings.
Ongoing Research Efforts
Several research groups worldwide are actively investigating CNS parasitic infections. These efforts include exploring new drug targets, evaluating the efficacy of existing drugs in combination therapies, and studying the pathogenesis of parasitic infections. Research into the development of vaccines is also ongoing, with the goal of preventing infection in the first place. For example, studies are exploring the use of monoclonal antibodies to target specific parasite antigens, potentially leading to novel therapeutic strategies.
Collaborative research efforts and knowledge sharing are essential for accelerating progress in this field.
Final Wrap-Up
In conclusion, parasitic infections of the central nervous system present a multifaceted challenge requiring a thorough understanding of the underlying biology, clinical presentations, and diagnostic procedures. The intricate interplay between parasite, host, and environment underscores the importance of comprehensive prevention strategies, effective treatment protocols, and ongoing research to combat these infections. This discussion has hopefully provided a clear and accessible overview of this complex medical area.