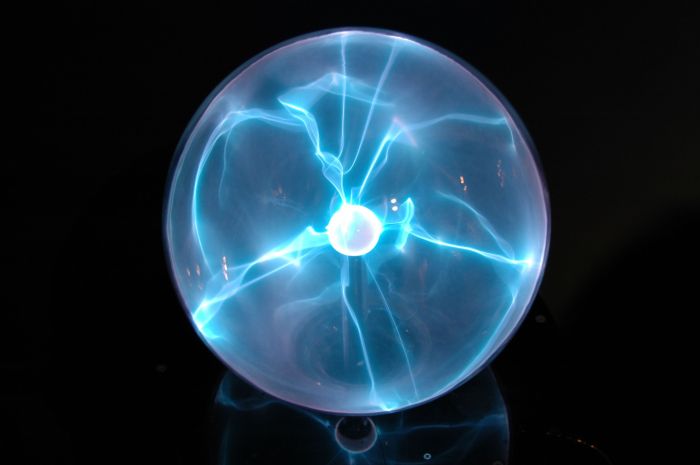
What is plasma in the body? It’s the liquid part of your blood, making up a significant portion – roughly 55% – of your blood volume. This vital component isn’t just a passive carrier; it plays a crucial role in transporting essential nutrients, hormones, and waste products throughout your body. Understanding plasma’s composition, function, and role in various bodily processes is key to comprehending your overall health.
Plasma, a yellowish liquid, is primarily composed of water, proteins, and electrolytes. These components work together to maintain osmotic pressure, facilitate immune responses, and enable the transport of crucial substances throughout your body. Let’s explore the intricate details of this fascinating bodily fluid.
Introduction to Plasma in the Body
Plasma is the liquid component of blood, making up roughly 55% of its total volume. It’s a pale yellow fluid that acts as a vital transport medium, carrying essential nutrients, hormones, and waste products throughout the body. Understanding plasma’s composition and function is key to comprehending the intricate workings of the circulatory system and overall human physiology.Plasma plays a crucial role in maintaining homeostasis.
It facilitates the delivery of oxygen from the lungs to the tissues, carries away carbon dioxide waste, and transports vital nutrients absorbed from the digestive system to cells needing them. This constant circulation ensures that cells receive the necessary resources for their metabolic functions and eliminate harmful byproducts.
Plasma Composition
Plasma is primarily composed of water, which acts as a solvent, allowing for the transportation of various substances. Dissolved within this watery matrix are a multitude of essential components, each contributing to the diverse functions of plasma.
Key Components of Plasma
Plasma’s diverse makeup is crucial for its function. It’s not just a simple fluid; it’s a complex solution of various substances working in concert to maintain the body’s delicate balance. Understanding these components is key to grasping plasma’s significance in human physiology.
| Component | Function | Example |
|---|---|---|
| Water | Acts as a solvent for dissolved substances, facilitating their transport throughout the body. Its high volume allows for efficient distribution of nutrients and removal of waste products. | |
| Proteins | Perform a wide array of functions, including maintaining osmotic pressure, transporting various molecules (like hormones and lipids), and contributing to the immune response. Different types of proteins have specific roles. | Albumin, globulins, fibrinogen |
| Electrolytes | Maintain the body’s fluid balance, facilitate nerve impulse transmission, and regulate muscle contractions. These include sodium, potassium, calcium, and chloride. | Sodium, Potassium, Calcium, Chloride |
| Nutrients | Provide essential building blocks for cell growth and repair. Examples include glucose, amino acids, and fatty acids. | Glucose, Amino acids, Fatty acids |
| Waste Products | Transport metabolic waste products from tissues to the organs responsible for their elimination (e.g., kidneys). | Urea, Creatinine |
| Gases | Transport oxygen from the lungs to the tissues and carbon dioxide from the tissues to the lungs. This crucial exchange is essential for cellular respiration. | Oxygen, Carbon dioxide |
| Hormones | Convey chemical signals throughout the body, regulating various physiological processes, such as growth, metabolism, and reproduction. | Insulin, Growth Hormone |
Composition of Plasma: What Is Plasma In The Body
Plasma, the liquid portion of blood, is a complex solution containing various components crucial for maintaining homeostasis. It’s not just a simple liquid; it’s a dynamic environment teeming with proteins, electrolytes, and other substances that facilitate a multitude of physiological processes. Understanding the composition of plasma is vital for comprehending how the body functions and diagnosing potential health issues.The intricate balance of these components is essential for proper blood function and overall health.
Imbalances in plasma composition can signify underlying health problems, highlighting the importance of regular health checkups and monitoring of blood parameters.
Plasma, the liquid part of your blood, plays a crucial role in many bodily functions. It’s essentially the transportation system for nutrients, hormones, and waste products throughout your body. Understanding the difference between conditions like osteoarthritis and rheumatoid arthritis, for example, osteoarthritis vs rheumatoid arthritis , can highlight how important healthy blood flow is to joint health.
So, next time you think about plasma, remember its vital role in keeping your body running smoothly.
Plasma Proteins
Plasma proteins are a diverse group of macromolecules with a wide array of functions. They contribute significantly to the osmotic pressure, transport of substances, and blood clotting. Their presence in plasma plays a vital role in maintaining the body’s equilibrium and facilitating crucial biological processes.
| Protein Type | Structure | Function |
|---|---|---|
| Albumin | Small, globular protein; predominant protein in plasma. | Maintains osmotic pressure, transports hormones, fatty acids, and drugs. |
| Globulins | Larger, diverse group of proteins; subdivided into alpha, beta, and gamma globulins. | Transport lipids, hormones, and antibodies; play a role in immunity. |
| Fibrinogen | Large, fibrous protein. | Crucial for blood clotting; converted to fibrin during clot formation. |
Electrolytes in Plasma
Electrolytes are essential minerals that carry an electrical charge and are vital for numerous bodily functions, including nerve impulse transmission, muscle contraction, and fluid balance. The precise concentration of electrolytes in plasma is critical for maintaining normal physiological processes.
| Electrolyte | Normal Range (approximate) | Function |
|---|---|---|
| Sodium (Na+) | 135-145 mEq/L | Maintains fluid balance, nerve impulse transmission, muscle contraction. |
| Potassium (K+) | 3.5-5.0 mEq/L | Crucial for nerve impulse transmission, muscle contraction, and regulating heart function. |
| Calcium (Ca2+) | 8.5-10.5 mg/dL | Essential for bone health, muscle contraction, nerve function, blood clotting. |
Important Note: The normal ranges for electrolytes can vary slightly depending on the laboratory and specific testing methods. Consult with a healthcare professional for personalized interpretations.
Plasma’s Role in Transport
Plasma, the liquid component of blood, acts as a vital transportation network throughout the body. It’s not just a passive carrier; it actively participates in delivering essential nutrients, hormones, and oxygen to tissues while removing waste products. This crucial role is essential for maintaining homeostasis and overall health.Plasma’s role extends far beyond simply moving substances. It provides a medium for various chemical reactions and maintains the appropriate osmotic pressure within the circulatory system, ensuring that cells receive the necessary fluids.
The efficient transport of these diverse materials relies on a complex interplay of factors, including plasma proteins and the specific properties of the transported substances.
Nutrients Transport
Plasma plays a critical role in transporting nutrients absorbed from the digestive system to various cells throughout the body. This is essential for cellular function and growth. These nutrients include sugars, amino acids, fatty acids, and vitamins. The specific mechanisms for transporting these substances vary depending on their chemical nature. For example, glucose, a simple sugar, is transported in dissolved form, while larger molecules like proteins are often bound to plasma proteins.
Hormone Transport
Hormones, chemical messengers produced by endocrine glands, regulate numerous bodily functions. Plasma serves as a crucial transport medium for hormones, ensuring they reach their target cells and exert their effects. The binding of hormones to specific plasma proteins influences their transport efficiency and duration of action. Different hormones have different binding affinities to these proteins. For example, thyroid hormones primarily bind to thyroxine-binding globulin (TBG), while some peptide hormones circulate freely in plasma.
Waste Product Removal
Plasma is also responsible for transporting waste products generated by cellular metabolism. These waste products, such as urea, creatinine, and bilirubin, are toxic to the body and need to be eliminated. Plasma proteins facilitate the transport of these substances to the kidneys, where they are filtered and excreted. Changes in the kidney’s function can directly impact the efficiency of waste product removal.
Plasma Proteins and Transport
Plasma proteins play a pivotal role in the transport of various substances. Albumin, the most abundant plasma protein, acts as a carrier for many substances, including hormones, fatty acids, and waste products. Globulins, another group of plasma proteins, also participate in transport, including binding to hormones and transporting lipids. Fibrinogen, crucial for blood clotting, is also a plasma protein.
These proteins bind to substances, preventing their loss from the blood and ensuring their safe delivery to target tissues.
Changes in Plasma Composition
Variations in plasma composition can significantly impact transport efficiency. For example, a decrease in albumin levels can lead to a reduction in the capacity to transport various substances. This can affect the delivery of nutrients, hormones, and waste products. Similarly, imbalances in other plasma proteins can also alter transport efficiency. The liver’s role in synthesizing plasma proteins is crucial in maintaining the overall efficiency of this transport system.
Plasma and Blood Clotting
Plasma, the liquid component of blood, plays a crucial role in the intricate process of blood clotting. This vital process prevents excessive blood loss from wounds, ensuring the body’s integrity. The coagulation cascade, a complex series of reactions, is initiated and facilitated by components within the plasma, leading to the formation of a fibrin clot that stops bleeding.The intricate web of plasma proteins and cellular elements orchestrates this cascade, transforming a liquid state into a solid clot.
Understanding this process is vital for diagnosing and treating bleeding disorders, which can result from deficiencies in these crucial plasma components.
Plasma, the liquid part of your blood, is essential for transporting nutrients and oxygen throughout your body. Sometimes, though, you might experience cramps without a period, which can be a sign of various underlying issues. If you’re experiencing this, it’s always a good idea to check out resources on cramps but no period to better understand the potential causes and when to seek medical attention.
Ultimately, understanding plasma’s role in your overall health is key to recognizing when something isn’t quite right.
Components Contributing to Clot Formation
Plasma contains a variety of proteins that contribute to the blood clotting process. These proteins, often circulating in an inactive form, are activated in a specific sequence to form a fibrin clot.
- Fibrinogen: A soluble protein that is converted into insoluble fibrin, the primary structural component of a blood clot. This conversion is a critical step in the coagulation cascade.
- Clotting Factors: A group of proteins that are activated sequentially. These factors are essential for the cascade’s progression and fibrin formation. Examples include factors like VIII, IX, and X.
- Platelets: Although not strictly a plasma component, platelets are crucial participants in clot formation. They adhere to damaged blood vessels and release substances that initiate the clotting process.
The Coagulation Cascade
The coagulation cascade is a complex sequence of enzymatic reactions, where one activated protein activates the next, culminating in the formation of a fibrin clot. This cascade is crucial for preventing excessive blood loss.
- Initiation: The cascade begins with the activation of clotting factors in response to tissue damage or vascular injury. This initial activation can occur via the intrinsic or extrinsic pathways.
- Amplification: The initial activation triggers a cascade of further activations, amplifying the response and leading to the formation of a larger clot. Positive feedback loops within the cascade ensure rapid and effective clot formation.
- Termination: The coagulation cascade must be regulated to prevent excessive clot formation. Certain proteins, such as antithrombin, work to inhibit the activation of clotting factors, ensuring the clot remains localized to the site of injury.
Effects of Plasma Protein Deficiencies on Clotting
Deficiencies in plasma proteins can significantly impact the blood clotting process, potentially leading to bleeding disorders. For example, hemophilia A is a genetic disorder characterized by a deficiency in factor VIII, leading to prolonged bleeding.
- Hemophilia: In hemophilia, a deficiency in specific clotting factors, most commonly factor VIII or factor IX, results in an inability to form a stable clot, leading to excessive bleeding.
- Von Willebrand Disease: This condition involves a deficiency or dysfunction of von Willebrand factor, a protein essential for platelet function and the activation of factor VIII. This can result in prolonged bleeding.
- Vitamin K Deficiency: Vitamin K is essential for the synthesis of several clotting factors. A deficiency can impair clot formation and lead to bleeding.
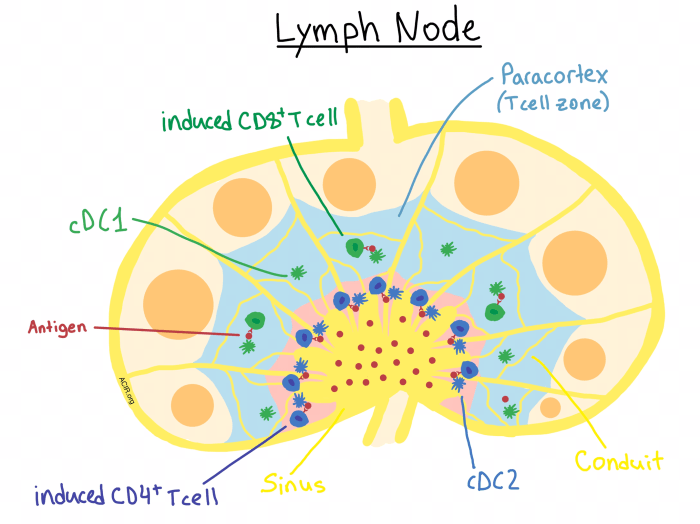
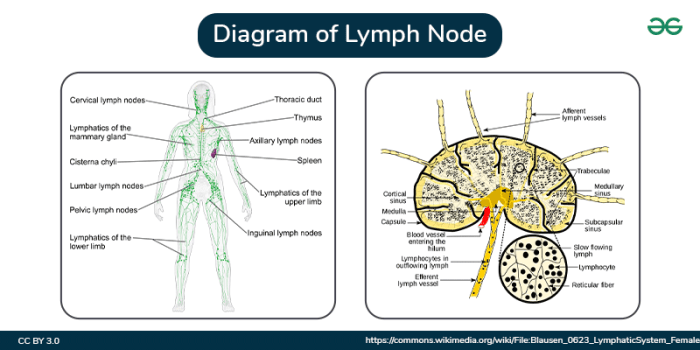
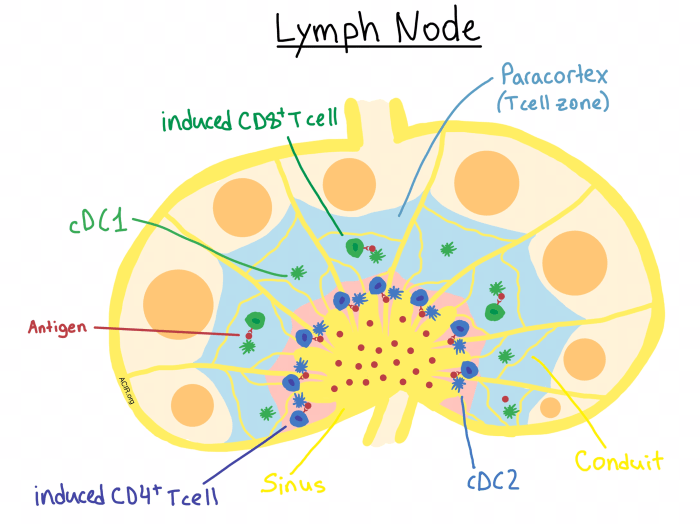
Plasma and Immunity
Plasma, the liquid component of blood, plays a crucial role in the body’s immune response. It acts as a transport system for immune cells and molecules, delivering them to sites of infection or injury. Understanding the interactions between plasma and the immune system is essential for comprehending how the body fights off disease.
Plasma Proteins and Immune Defense
Plasma is not just a simple liquid; it’s a complex solution teeming with proteins vital for various bodily functions, including immunity. These proteins act as messengers, signaling molecules, and effectors in the immune response. Their diverse roles in the immune system are essential for a robust defense mechanism.
Antibodies and Their Production
Antibodies, specialized proteins produced by the immune system, are crucial components of the humoral immune response. Plasma, as the primary transport medium, carries these antibodies throughout the body. The presence of antibodies in plasma is a key indicator of the body’s immune response to a specific pathogen. Plasma plays a pivotal role in recognizing and neutralizing pathogens.
Specific Proteins Involved in Immune Defense, What is plasma in the body
Several plasma proteins are critical players in the immune system. Complement proteins, for example, act as a cascade of enzymes, enhancing the ability of antibodies to destroy pathogens. Another important class is the acute-phase proteins, which increase in concentration during infection, reflecting the body’s inflammatory response.
- Complement System: This system comprises a collection of proteins that work together to enhance the ability of antibodies and phagocytes (cells that engulf pathogens) to eliminate pathogens. Activation of the complement system often leads to the lysis (destruction) of pathogen cells, a crucial aspect of the immune response. The complement system plays a vital role in both innate and adaptive immunity.
Plasma, the liquid part of your blood, is crucial for transporting nutrients and oxygen throughout your body. It’s fascinating how vital this component is for overall health. Interestingly, some believe that remedies like oscillococcinum can help with various health issues, and exploring its potential benefits might be worth your time. health benefits of oscillococcinum are a subject of ongoing discussion, but understanding the role of plasma in supporting bodily functions remains important.
Regardless of your views on supplements, maintaining a healthy balance of fluids and nutrients in your body is key to overall well-being, and plasma plays a central part in this.
- Acute-Phase Proteins: These proteins, including C-reactive protein (CRP), are produced in the liver in response to inflammation. Increased levels of acute-phase proteins often indicate an ongoing infection or inflammatory process. Monitoring these proteins can be useful in diagnosing and monitoring diseases.
- Antibodies (Immunoglobulins): Antibodies, also known as immunoglobulins, are proteins that specifically recognize and bind to foreign substances (antigens). They are essential components of the adaptive immune response. Different classes of antibodies (IgG, IgM, IgA, IgE, IgD) have unique roles in neutralizing pathogens and activating other immune cells. These antibodies circulate in the plasma and play a direct role in pathogen elimination.
Relationship Between Plasma and Antibody Function
Plasma provides the transport mechanism for antibodies to reach their targets throughout the body. The concentration of specific antibodies in the plasma reflects the body’s ongoing immune response to a particular pathogen. Measuring antibody levels can be a valuable diagnostic tool.
Clinical Significance of Plasma
Plasma, the liquid component of blood, holds immense clinical significance. Its analysis provides invaluable insights into a patient’s overall health and aids in diagnosing a wide range of conditions. From identifying infections to assessing organ function, plasma tests are essential tools in modern medical practice. Understanding the intricacies of plasma analysis empowers healthcare professionals to make informed decisions and deliver targeted treatments.
Plasma in Medical Diagnostics
Plasma serves as a rich source of information regarding a patient’s health status. Numerous substances, including proteins, electrolytes, hormones, and waste products, are dissolved within it. Variations in these components can signal various diseases or conditions. Analyzing plasma composition allows healthcare providers to identify abnormalities and guide treatment strategies.
Examples of Plasma Analysis in Disease Diagnosis
Plasma analysis is pivotal in diagnosing a multitude of conditions. Elevated levels of certain proteins, such as C-reactive protein (CRP), can indicate inflammation, often associated with infections or autoimmune diseases. Abnormal liver function tests, often derived from plasma samples, can suggest liver damage or disease. Electrolyte imbalances, detectable through plasma analysis, can point to dehydration, kidney dysfunction, or other underlying issues.
For instance, a low potassium level in plasma might indicate Addison’s disease.
Significance of Plasma in Blood Transfusions
Plasma plays a critical role in blood transfusions, particularly in cases of severe blood loss or specific deficiencies. Fresh frozen plasma (FFP) is a crucial component in treating patients with clotting disorders or those who have experienced significant blood loss. The plasma component in FFP contains clotting factors, which are essential for preventing bleeding. Furthermore, plasma can be used to replenish lost volume and maintain blood pressure in such situations.
Plasma Collection and Processing
Plasma is typically collected from blood donors. The blood is first drawn and then separated into its components through a process known as centrifugation. This technique allows the separation of plasma from red blood cells and other cellular components. The separated plasma is then processed and stored under controlled conditions to maintain its quality and effectiveness. The procedure is carefully regulated to ensure safety and quality control.
Plasma Tests and Their Clinical Applications
Plasma analysis encompasses a wide range of tests, each designed to assess specific components and their levels. A comprehensive overview of various plasma tests and their clinical applications is provided in the table below.
| Plasma Test | Clinical Application | Expected Result |
|---|---|---|
| Complete Blood Count (CBC) | Assessment of overall blood health; detection of anemia, infection, and other blood disorders. | Normal ranges for red blood cells, white blood cells, and platelets. |
| Liver Function Tests (LFTs) | Evaluation of liver health; detection of liver damage, disease, or dysfunction. | Normal levels of enzymes (ALT, AST) and bilirubin. |
| Kidney Function Tests (KFTs) | Assessment of kidney function; detection of kidney disease or damage. | Normal levels of creatinine and blood urea nitrogen (BUN). |
| Electrolyte Panel | Evaluation of electrolyte balance (sodium, potassium, calcium, etc.); detection of imbalances. | Electrolytes within normal ranges, specific to individual needs. |
| Lipid Profile | Assessment of cholesterol and triglyceride levels; detection of cardiovascular risk factors. | Desirable levels of cholesterol and triglycerides. |
| Coagulation Studies | Evaluation of blood clotting factors; detection of bleeding disorders or clotting problems. | Normal clotting factor levels. |
Maintaining Plasma Balance
Plasma, the liquid component of blood, is a dynamic solution constantly adjusting to maintain a stable composition. This delicate balance is crucial for optimal bodily functions. Maintaining the right concentration of water, electrolytes, and proteins within plasma is essential for transporting nutrients, removing waste products, and regulating various physiological processes. Disruptions in this balance can lead to a range of health problems.Maintaining plasma balance involves a complex interplay of several bodily systems, particularly the kidneys, liver, and the body’s intricate regulatory mechanisms.
These systems work in concert to maintain the appropriate levels of various substances, ensuring the health and well-being of the body.
Renal Regulation of Plasma Volume and Electrolyte Concentration
The kidneys play a pivotal role in regulating plasma volume and electrolyte concentration. They meticulously filter blood, reabsorbing essential substances and excreting waste products. This process allows the kidneys to fine-tune the composition of plasma to maintain homeostasis. For instance, if the body loses significant amounts of water through sweating, the kidneys increase water reabsorption, reducing urine output and restoring plasma volume.
Conversely, if plasma volume becomes excessive, the kidneys increase urine output to maintain equilibrium. The kidneys also regulate electrolyte concentrations like sodium, potassium, and calcium, crucial for nerve and muscle function.
Hepatic Contribution to Plasma Protein Levels
The liver is the primary site for synthesizing many crucial plasma proteins, including albumin, globulins, and clotting factors. Albumin, in particular, is essential for maintaining the osmotic pressure of plasma, preventing fluid leakage from blood vessels. Liver damage or disease can significantly impair the synthesis of these proteins, leading to edema (swelling) and other complications. For example, cirrhosis of the liver often results in decreased albumin production, leading to fluid buildup in the body’s tissues.
A healthy liver is thus vital for maintaining the correct protein levels within plasma.
Dietary Importance for Plasma Health
A balanced diet plays a critical role in maintaining plasma health. A diet rich in essential nutrients, including proteins, vitamins, and minerals, supports the proper function of all the bodily systems involved in plasma regulation. Sufficient protein intake is essential for the liver to synthesize plasma proteins. Adequate hydration is crucial for maintaining plasma volume. A diet deficient in essential nutrients can compromise the liver’s ability to produce plasma proteins, and also lead to electrolyte imbalances, affecting plasma composition and impacting overall health.
For example, a diet lacking in vitamin K can impair blood clotting, impacting plasma’s ability to form clots.
Epilogue
In summary, plasma is a dynamic and essential component of blood, acting as a vital transport system for nutrients, hormones, and waste products. Its composition, including water, proteins, and electrolytes, directly influences its various functions, from maintaining osmotic balance to supporting immune responses and blood clotting. Understanding plasma’s role is crucial for comprehending overall health and the complex interplay of bodily processes.
The next time you think about your blood, remember the critical role of plasma. It’s the unsung hero behind many of the essential functions that keep you alive and healthy.