Serratus anterior muscle anatomy is crucial for understanding upper body movement. This detailed exploration delves into the muscle’s location, function, and intricate relationships with surrounding structures. We’ll examine its origin and insertion points, fiber arrangement, innervation, and blood supply, ultimately connecting these elements to its vital role in actions like pushing, reaching, and protraction. Prepare to unravel the secrets of this essential muscle!
Understanding the serratus anterior muscle is vital for anyone interested in human anatomy, physical therapy, or sports performance. Its function in scapular movement and overall posture is significant. This detailed look at its structure, function, and clinical relevance will provide a comprehensive understanding.
Overview of the Serratus Anterior Muscle
The serratus anterior muscle, a vital component of the upper body’s musculature, plays a crucial role in shoulder stability and movement. Its unique structure and location contribute significantly to a wide range of activities, from simple arm movements to complex athletic endeavors. Understanding its anatomical relationships with surrounding structures is key to appreciating its function and potential for injury.The serratus anterior, a broad, fan-shaped muscle, originates along the surface of the ribs and inserts on the medial border of the scapula.
This positioning allows it to act as a powerful stabilizer and mover of the scapula, which in turn affects the position and movement of the entire upper limb. Its complex interplay with other shoulder muscles ensures coordinated and controlled motion.
Anatomical Location and Function
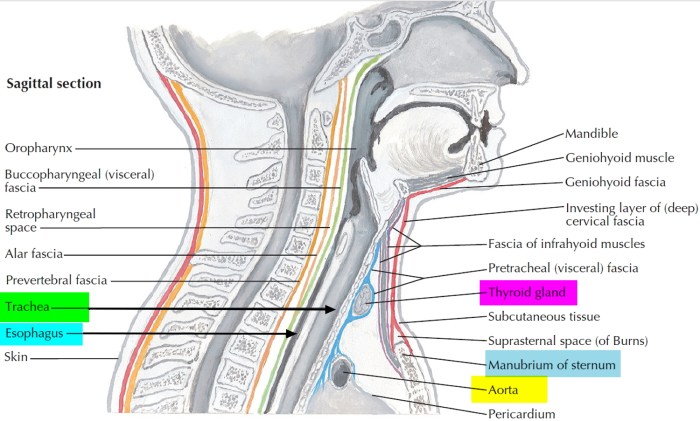
The serratus anterior muscle is situated deep to the pectoral muscles, spanning the lateral portion of the chest wall. It’s characterized by its serrated or saw-toothed appearance, reflecting its origin from multiple ribs. This unique anatomical arrangement allows for efficient force transmission and diverse movement patterns. Its function is multifaceted, encompassing both stabilization and dynamic movement.
| Anatomical Location | Function | Related Structures |
|---|---|---|
| Located deep to the pectoral muscles, spanning the lateral chest wall, originating from the upper ribs and inserting on the medial border of the scapula. | Stabilizes the scapula against the thoracic cage, facilitating upward rotation of the scapula. It also plays a crucial role in protraction (pushing the scapula forward) and upward rotation of the scapula, essential for reaching and pushing movements. | Pectoral muscles, ribs, scapula, trapezius, rotator cuff muscles, and the clavicle. Its relationship with the scapula is particularly critical for maintaining the proper positioning of the shoulder girdle. |
Significance in Upper Body Movement
The serratus anterior’s contribution to upper body movement is substantial. Its role in protracting and upwardly rotating the scapula is vital for activities like pushing, reaching, and throwing. Without proper serratus anterior function, the scapula can become improperly positioned, potentially leading to impingement syndromes or reduced range of motion. This improper positioning can restrict the full potential of the shoulder joint and create compensations in other muscles, potentially leading to pain or injury.
Relationships with Surrounding Structures
The serratus anterior interacts closely with several crucial upper body structures. Its proximity to the ribs allows for effective leverage during respiration, and its relationship with the scapula is fundamental to shoulder function. Its intricate connection with the rotator cuff muscles ensures coordinated movement and stability. Understanding these relationships is crucial for recognizing potential impairments and promoting optimal shoulder health.
Understanding the serratus anterior muscle’s anatomy is crucial for appreciating its role in shoulder blade movement. This intricate muscle, vital for proper scapular function, is closely connected to the overall mechanics of the body. Similar to how the circle of willis anatomy function and significance ( circle of willis anatomy function and significance ) dictates the brain’s blood supply, the serratus anterior’s proper form and function is essential for maintaining a healthy range of motion in the shoulder and upper back.
A deep understanding of its anatomy is key to recognizing potential problems and maintaining its vital role in the upper body.
Origin and Insertion
The serratus anterior muscle, a crucial component of the shoulder girdle, plays a vital role in scapular movement and stability. Understanding its origin and insertion points is essential for comprehending its function and how it interacts with surrounding muscles. These attachments are critical for proper shoulder mechanics and preventing injuries.The serratus anterior’s origin and insertion points are unique, contributing to its multifaceted role in the body.
Its complex attachments allow it to exert forces on the scapula in various directions, facilitating a wide range of arm movements. A thorough understanding of these attachment points is necessary for assessing muscle imbalances and designing effective rehabilitation strategies.
Understanding the serratus anterior muscle’s intricate anatomy is crucial for physical therapists and athletes alike. This muscle, vital for shoulder blade movement and proper posture, plays a key role in everyday functions. However, sometimes, concerning symptoms like a headache can arise, potentially signaling something more serious, such as a brain aneurysm. Learning how long a brain aneurysm headache typically lasts can be incredibly valuable in recognizing the urgency of such situations.
how long does a brain aneurysm headache last This knowledge, combined with a deep understanding of the serratus anterior muscle, empowers individuals to take the necessary precautions and seek appropriate medical attention. Ultimately, focusing on healthy movement and paying attention to unusual sensations are vital for overall well-being.
Origin Points
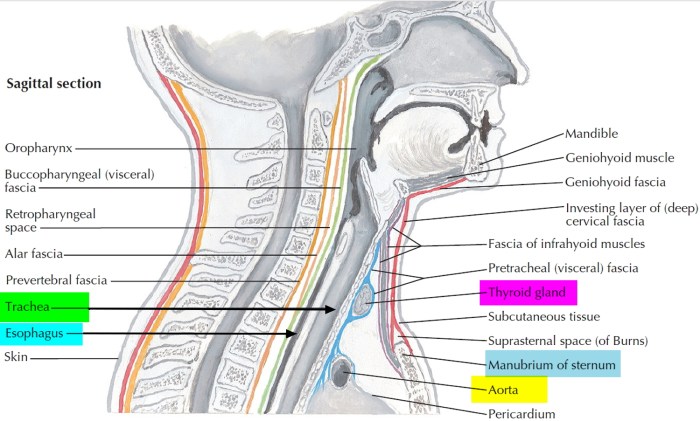
The serratus anterior originates from a series of small, serrated, bony projections along the upper eight ribs. These attachments provide a broad surface area for muscle fibers to attach, enabling significant force generation. This expansive origin allows the muscle to exert considerable pulling power on the scapula.
Insertion Points
The serratus anterior inserts along the entire anterior surface of the medial border of the scapula. This insertion point ensures that the muscle can effectively pull the scapula forward and upward, crucial for arm elevation and protraction. This extensive insertion area allows for precise control of scapular movement.
Comparison with Neighboring Muscles
The serratus anterior’s origin and insertion points differ significantly from those of neighboring muscles, reflecting its unique function. For example, the pectoralis minor, while also involved in scapular movement, originates from ribs 3-5 and inserts on the coracoid process of the scapula. This distinct origin and insertion pattern differentiates its action from that of the serratus anterior. The trapezius, another important shoulder muscle, has a more superior and lateral origin, while its insertion point is spread across the clavicle and scapula.
This different arrangement allows the trapezius to play a vital role in shoulder elevation and rotation, functions that differ from the serratus anterior’s primary functions of scapular protraction and upward rotation.
Table of Origin and Insertion Points
| Muscle | Origin | Insertion |
|---|---|---|
| Serratus Anterior | Anterior surfaces of upper eight ribs | Anterior surface of medial border of scapula |
| Pectoralis Minor | Ribs 3-5 | Coracoid process of scapula |
| Trapezius | Occipital bone, spinous processes of thoracic vertebrae | Clavicle, scapula (acromion and spine) |
Anatomical Structure and Fiber Arrangement
The serratus anterior, a vital muscle for shoulder stability and upper body movement, boasts a complex anatomical structure. Understanding its fiber arrangement is key to appreciating its diverse functions. This intricate design allows the muscle to effectively interact with the scapula, enabling a wide range of arm motions. Its layered organization and specific fascicle orientations are critical to its overall performance.The serratus anterior’s function is not just about brute force; its precise control over scapular movement is essential for fine motor skills and complex tasks.
Its fiber arrangement contributes significantly to this precision. The arrangement and structure of the muscle fibers directly impact how the muscle moves and interacts with surrounding structures, ensuring efficient and controlled scapular movement.
Fiber Arrangement and Fascicles
The serratus anterior muscle is comprised of multiple fascicles, which are bundles of muscle fibers. These fascicles run obliquely across the muscle, contributing to its broad and fan-like appearance. This oblique orientation allows for a range of movement and force generation. The arrangement of these fascicles is not uniform; they are grouped into layers, further optimizing the muscle’s functionality.
Layers and Fascicle Organization
The muscle’s fibers are arranged in a series of approximately 20 or more layers, not rigidly distinct but overlapping in a complex arrangement. These layers aren’t easily separated, but their presence is crucial for the nuanced control of the scapula. Each layer contributes to a specific aspect of scapular movement, ensuring coordinated and efficient action.
Understanding the serratus anterior muscle’s anatomy is crucial for its function in shoulder blade movement. However, cognitive function can also be impacted by conditions like early-onset Alzheimer’s, which can be screened for using tests like the Stroop test. Learning more about this test and how it helps identify potential issues can be valuable. what is the stroop test screening early alzheimers This highlights the interconnectedness of various bodily systems, and how even seemingly isolated issues like muscle function can be linked to broader health concerns.
A healthy understanding of the serratus anterior is key for overall upper body strength and movement.
Anatomical Features Contributing to Form and Function
Several anatomical features contribute to the serratus anterior’s distinctive form and function. Its broad origin on the ribs, combined with its wide insertion on the medial border of the scapula, allows for a large range of motion. The oblique arrangement of fibers is a significant factor, facilitating the complex interplay needed for scapular movement. The muscle’s attachments also play a crucial role in its mechanical advantage and the generation of force for a variety of tasks.
Illustration of Fiber Arrangement
Imagine the serratus anterior as a broad, fan-shaped structure. The fibers, like the ribs they originate from, are not vertical but run obliquely downward and outward from the ribs. This diagonal orientation is critical for its function, allowing the muscle to both elevate and rotate the scapula. The individual fascicles interweave and overlap, creating a complex, layered structure.
At the point where the muscle inserts on the scapula, the fibers converge and attach, transmitting force effectively to the scapula. The muscle’s broad, fan-like form, coupled with its oblique fiber orientation, allows it to generate a considerable pulling force on the scapula, facilitating a wide array of movements.
Innervation and Blood Supply
The serratus anterior, a vital muscle for scapular stability and movement, relies on a precise network of nerves and blood vessels for proper function. Understanding these pathways is crucial for diagnosing and treating injuries or conditions affecting this muscle. Disruptions to the innervation or blood supply can lead to significant functional limitations and pain, highlighting the importance of a comprehensive understanding of these systems.
Nerve Innervation
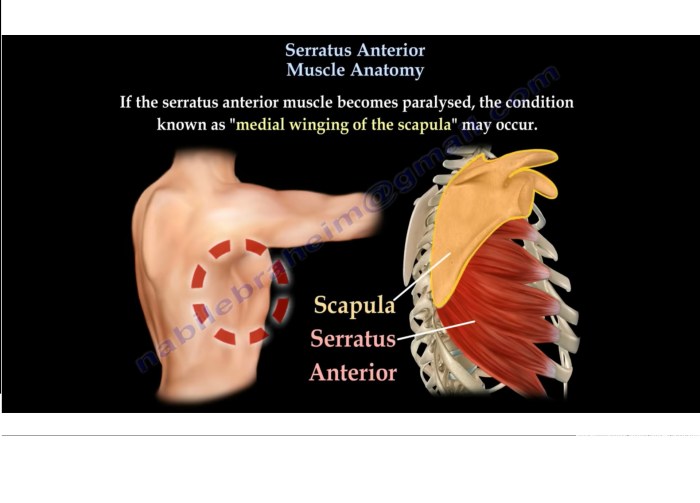
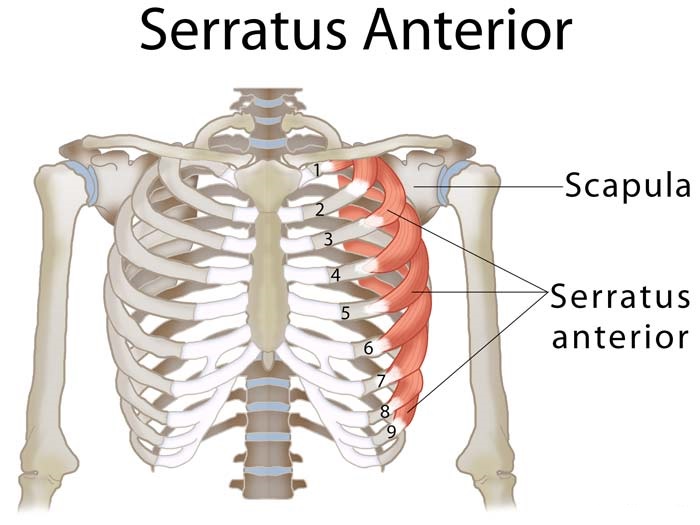
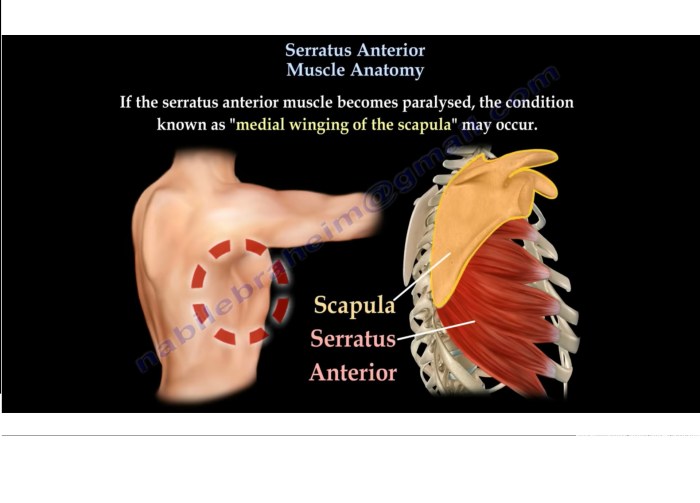
The serratus anterior muscle is primarily innervated by the long thoracic nerve. This nerve, originating from the C5, C6, and C7 nerve roots, travels along the lateral aspect of the thorax, providing motor signals to the muscle fibers. Damage to the long thoracic nerve, often due to injury or surgical procedures, can result in a condition known as serratus anterior paralysis.
This paralysis can lead to winging of the scapula, a noticeable protrusion of the scapula’s medial border, impacting shoulder function and range of motion. This impairment is a classic example of how disruption in nerve pathways can directly affect muscle function.
Blood Supply
The serratus anterior receives its blood supply primarily from branches of the superior thoracic artery, the lateral thoracic artery, and the subscapular artery. These arteries provide oxygenated blood to the muscle, enabling proper cellular function. The distribution of blood vessels ensures a sufficient supply to all portions of the muscle, crucial for maintaining its structural integrity and contractile abilities.
A compromised blood supply, such as in cases of severe trauma or vascular disease, can lead to muscle ischemia, potentially causing significant pain and weakness. A thorough understanding of the blood supply is essential for developing effective treatment plans in such situations.
Clinical Significance of Disruptions
Disruptions to the innervation or blood supply of the serratus anterior muscle can have significant clinical implications. Serratus anterior paralysis, as mentioned earlier, can lead to noticeable scapular winging, affecting shoulder function and potentially contributing to pain and discomfort. Furthermore, impaired blood supply could lead to muscle atrophy and weakness, impacting the individual’s ability to perform activities involving shoulder movement and stability.
Proper diagnosis and treatment are critical in these cases to restore normal function and prevent long-term complications.
Comparison of Nerve and Blood Supply to Nearby Muscles
| Muscle | Nerve Supply | Blood Supply |
|---|---|---|
| Serratus Anterior | Long thoracic nerve (C5, C6, C7) | Superior thoracic artery, Lateral thoracic artery, Subscapular artery |
| Pectoralis Major | Medial and lateral pectoral nerves (C5-T1) | Thoracoacromial artery, Lateral thoracic artery, Superior thoracic artery |
| Trapezius | Accessory nerve (CN XI), spinal accessory nerve (C3-C4) | Occipital artery, superficial branches of the posterior scapular artery, transverse cervical artery, suprascapular artery |
| Rhomboids | Dorsal scapular nerve (C4, C5) | Dorsal scapular artery, branches of the subscapular artery |
This table provides a concise overview of the nerve and blood supply for the serratus anterior muscle, as well as a comparison with some nearby muscles. It emphasizes the variations in innervation and blood supply between muscles, highlighting the unique characteristics of each. Recognizing these differences is essential for understanding the potential implications of injuries or pathologies affecting the musculoskeletal system.
Actions and Movements: Serratus Anterior Muscle Anatomy
The serratus anterior muscle, a vital player in upper body movement, isn’t just about aesthetics; it’s about functionality. Its unique anatomical structure, with fibers running obliquely across the ribs, gives it a powerful role in stabilizing and moving the scapula (shoulder blade), enabling a wide range of upper body actions. Understanding its actions is crucial for comprehending how we perform tasks like pushing, reaching, and throwing.The serratus anterior’s primary function revolves around scapular protraction, upward rotation, and stabilization.
This intricate interplay of movements unlocks a variety of upper body actions, influencing everything from reaching for a high shelf to performing a powerful push-up. It’s a silent powerhouse, contributing significantly to the fluidity and precision of our upper body movements.
Primary Actions
The serratus anterior muscle exhibits several key actions crucial for upper body mechanics. Its primary role is to protract the scapula, pulling it forward and away from the spine. This action is essential for reaching, pushing, and many other upper body movements. Beyond protraction, the serratus anterior also contributes to scapular upward rotation and helps to stabilize the scapula during these movements.
Scapular Movement
The serratus anterior’s impact on scapular movement is profound. Its attachment points allow it to effectively pull the scapula forward and upward, facilitating a wide range of motions. Without proper serratus anterior function, scapular stability and coordinated movement are compromised. This can lead to issues with shoulder positioning and range of motion, potentially impacting everyday tasks and athletic performance.
Proper scapular movement is crucial for preventing injury and optimizing performance in activities involving the upper body.
Role in Upper Body Movements
The serratus anterior is instrumental in several upper body movements. Let’s explore how it contributes to these actions:
- Pushing: When performing a push-up or bench press, the serratus anterior powerfully protracts the scapulae, providing stability to the shoulder girdle and enabling the necessary force generation for pushing movements. This stabilization prevents the shoulders from collapsing inwards, allowing for a more efficient and controlled movement.
- Reaching: Extending the arm forward requires protraction of the scapula, a task primarily handled by the serratus anterior. This action allows for a full range of motion and the ability to reach objects overhead or far in front of the body.
- Protraction: The serratus anterior is the primary muscle responsible for protracting the scapula. This movement is critical for activities that involve pushing, reaching, and maintaining shoulder stability during a variety of upper body actions.
Movement Summary Table
This table summarizes the actions of the serratus anterior in different upper body movements.
| Movement | Muscle Action |
|---|---|
| Pushing (e.g., push-ups, bench press) | Protraction of scapula, upward rotation, and stabilization |
| Reaching (e.g., overhead reaching, throwing) | Protraction and upward rotation of scapula |
| Protraction | Primary action of protracting the scapula |
| Pulling (e.g., rowing) | Stabilizing the scapula and assisting with upward rotation |
Clinical Relevance
The serratus anterior muscle, crucial for shoulder stability and movement, is susceptible to various injuries and conditions. Understanding these issues is vital for accurate diagnosis and effective treatment. Proper assessment and management of serratus anterior problems can significantly impact a patient’s overall shoulder health and functional capacity.Common conditions affecting the serratus anterior muscle can range from minor strains to more serious pathologies.
These issues can manifest in different ways, impacting daily activities and requiring tailored treatment plans. Identifying the specific cause and extent of the problem is paramount for successful rehabilitation.
Common Conditions Affecting the Serratus Anterior
The serratus anterior, often overworked or underused, can experience a range of issues. Common conditions include:
- Serratus Anterior Strain/Sprain: Overuse or sudden forceful movements can lead to strains or sprains in the serratus anterior muscle. This often results from repetitive overhead activities or sudden impacts. Pain, tenderness, and reduced range of motion are common symptoms.
- Serratus Anterior Winging: This condition involves the scapula (shoulder blade) “winging” or protruding outward, particularly noticeable when the arm is raised. This is often a sign of underlying weakness or dysfunction in the serratus anterior muscle. Potential causes include nerve damage (e.g., long thoracic nerve injury), muscle weakness, or postural issues.
- Scapular Dyskinesis: This is a broader term encompassing altered scapular movement patterns. Serratus anterior dysfunction is frequently implicated in scapular dyskinesis, as its role in scapular stabilization is crucial. Symptoms can range from subtle discomfort to noticeable postural changes.
- Thoracic Outlet Syndrome (TOS): While not solely a serratus anterior issue, TOS can involve compression of nerves and blood vessels in the area surrounding the serratus anterior. Symptoms may include pain, numbness, and tingling in the shoulder, arm, or hand.
Symptoms Associated with Serratus Anterior Muscle Injuries or Dysfunction
Symptoms vary depending on the specific condition and severity. Common symptoms include:
- Pain: Localized pain in the shoulder, upper back, or chest region, which may worsen with specific movements or activities.
- Tenderness: Pain upon palpation (touching) of the serratus anterior muscle.
- Weakness: Difficulty performing activities requiring serratus anterior activation, such as pushing, pulling, or overhead movements.
- Scapular Winging: Visually observable outward protrusion of the scapula, particularly noticeable when the arm is raised.
- Numbness or Tingling: If the underlying cause involves nerve compression, numbness or tingling may occur in the arm or hand.
Diagnostic Procedures for Assessing Serratus Anterior Problems
Diagnosing serratus anterior issues involves a combination of methods:
- Patient History: Gathering information about the patient’s activities, recent injuries, and symptoms is crucial for identifying potential causes.
- Physical Examination: A thorough physical examination, including palpation (touching), range-of-motion assessment, and specific muscle strength testing, can help identify muscle weakness or dysfunction.
- Imaging Studies (e.g., X-rays, MRI): These may be necessary to rule out other conditions or evaluate the extent of the injury. Imaging is often not the first line of investigation, but can be helpful in cases of suspected underlying pathology.
- Nerve Conduction Studies: In cases of suspected nerve involvement, nerve conduction studies can help assess the health and function of the nerves.
Potential Treatment Options for Serratus Anterior Issues
Treatment approaches vary depending on the severity and cause of the condition:
- Conservative Treatment: Rest, ice, and physical therapy are often the initial approaches for minor strains or sprains. This often includes exercises focusing on strengthening the serratus anterior and surrounding muscles, improving posture, and addressing any underlying postural imbalances.
- Manual Therapy: Techniques like massage or mobilization may be used to address any restrictions in soft tissues or joints.
- Medications: Pain relievers or anti-inflammatory medications may be used to manage symptoms.
- Surgical Intervention: In cases of significant nerve damage or severe muscle tears, surgical repair may be necessary. Surgery is typically a last resort and reserved for cases where conservative treatments have not been successful.
Long-Term Implications of Untreated Serratus Anterior Problems
Untreated serratus anterior problems can lead to chronic pain, persistent shoulder dysfunction, and potential postural deformities. This can affect daily activities and long-term quality of life.
Implications of Serratus Anterior Weakness on Overall Posture and Shoulder Function
Serratus anterior weakness directly impacts scapular stability and position. This, in turn, can lead to postural imbalances, including rounded shoulders and altered upper back curvature. Compromised shoulder function can hinder a wide range of activities, from simple reaching to more complex overhead movements.
Variations and Anomalies
The serratus anterior muscle, while generally consistent in its structure, can exhibit variations in its morphology. These variations, often subtle, can influence its function and potentially lead to subtle or significant consequences. Understanding these variations is crucial for accurate diagnosis and treatment in clinical settings.
Variations in Morphology
The serratus anterior muscle’s morphology can vary in several ways, impacting its size, shape, and attachments. These variations are often subtle and may not always manifest as clinically significant problems. However, a thorough understanding of these potential anomalies is important for differentiating them from more significant pathological conditions.
Variations in Attachments
The serratus anterior muscle’s origin and insertion points can exhibit variability. For example, the origin may extend slightly further superiorly or inferiorly along the ribs, or the insertion may vary slightly on the scapula. These changes, while often minor, can affect the muscle’s leverage and consequently its ability to perform its primary actions. Sometimes, the muscle might be partially or completely absent.
Such variations can be associated with other congenital musculoskeletal anomalies.
Variations in Size
The size of the serratus anterior muscle can vary significantly between individuals, even within the normal range. Factors such as age, physical activity, and overall body composition can influence muscle size. However, significantly smaller or larger serratus anterior muscles might be indicative of underlying conditions or developmental issues. For example, individuals with significantly reduced muscle mass may have difficulty with scapular protraction and upward rotation, potentially impacting shoulder function.
Impact on Function
Variations in serratus anterior muscle morphology can potentially impact its function. A smaller muscle size, for instance, may lead to reduced strength during protraction and upward rotation of the scapula. Variations in attachments can also alter the muscle’s mechanical advantage, affecting its ability to perform its designated movements. This can impact activities such as throwing, pushing, and overhead reaching.
In some cases, a significant variation might lead to shoulder instability.
Comparison of Typical and Variant Anatomical Structures, Serratus anterior muscle anatomy
| Anatomical Feature | Typical Structure | Variant Structure | Potential Impact on Function |
|---|---|---|---|
| Origin | Anterior surfaces of upper 8-9 ribs | Superior or inferior extension of origin along ribs | Slight alteration in leverage and potential reduction in protraction strength |
| Insertion | Anterior surface of the medial border of the scapula | Slight variations in insertion point on scapula | Minor changes in mechanical advantage, potentially affecting upward rotation and scapular stabilization |
| Size | Moderately sized muscle with consistent shape | Significantly smaller or larger than average | Reduced strength in protraction/upward rotation, potential shoulder instability, or possible underlying conditions |
Comparative Anatomy (Optional)
The serratus anterior muscle, crucial for scapular stability and movement, exhibits variations in structure and function across different species. Understanding these comparative aspects reveals insights into the evolutionary pressures shaping the muscle and its role in diverse locomotor strategies. This exploration examines the adaptations of the serratus anterior across various species, highlighting how its characteristics reflect the specific functional needs of each organism.
Structural Variations Across Species
The serratus anterior’s morphology displays significant diversity. In some species, the muscle’s size and shape are directly correlated with the animal’s lifestyle and locomotion. For instance, arboreal primates often exhibit a more robust serratus anterior, supporting the significant overhead movements and climbing actions. Conversely, terrestrial mammals may have a less pronounced muscle, as their movement patterns place less emphasis on scapular protraction and upward rotation.
Functional Adaptations in Different Species
The serratus anterior’s function adapts to the specific locomotor requirements of each species. In flying mammals, such as bats, the muscle’s role in maintaining wing posture and generating the necessary forces for flight is profoundly important. This necessitates a powerful and well-developed serratus anterior, allowing for precise wing manipulation. In contrast, the serratus anterior’s role in a quadrupedal mammal might be more focused on stabilizing the scapula during locomotion, while in a bipedal species, it is vital for shoulder girdle stability during walking and running.
These adaptations demonstrate the profound influence of functional demands on muscle morphology.
Evolutionary Implications of Serratus Anterior Characteristics
The evolution of the serratus anterior reflects the changing demands of locomotion and posture. The development of more complex movements, such as arboreal locomotion or flight, led to the selection for larger and more robust serratus anterior muscles. This demonstrates the direct relationship between evolutionary pressures and the structural and functional adaptations of the muscle.
Comparative Analysis Table
| Species | Locomotion | Serratus Anterior Size & Shape | Primary Function | Adaptations |
|---|---|---|---|---|
| Human | Bipedal | Moderate size, fan-shaped | Scapular protraction, upward rotation, stabilization | Supports complex arm movements, posture maintenance |
| Chimpanzee | Arboreal, quadrupedal | Robust, well-developed | Scapular protraction, upward rotation, support during climbing | Supports significant overhead movements, arboreal locomotion |
| Dog | Quadrupedal | Relatively smaller, less prominent | Scapular stabilization during locomotion, some protraction | Supports simpler, terrestrial locomotion |
| Bat | Flight | Large, powerful | Wing posture maintenance, force generation for flight | Adaptations crucial for generating forces for flight |
Closure
In conclusion, the serratus anterior muscle is a complex and crucial component of the upper body. Its intricate anatomy, diverse functions, and clinical implications make it a fascinating subject for study. This exploration has provided a comprehensive overview, highlighting its role in various movements and its vulnerability to injury. Hopefully, this in-depth analysis has broadened your understanding and appreciation for this vital muscle.