How to select the correct needle size for an injection is crucial for patient safety. Using the wrong size can lead to complications, from discomfort to serious health risks. This comprehensive guide will delve into the factors influencing needle size selection, the methods for determining the appropriate gauge, and the essential safety precautions to follow. Understanding the relationship between needle size and patient safety is paramount.
We’ll explore various needle types and their applications, providing clear explanations and practical examples.
Choosing the right needle size is essential for administering medications effectively and safely. Factors like the medication’s viscosity, the patient’s size and health conditions, and the injection site all play a role. We’ll examine the nuances of these factors and how they affect needle selection. The guide will include tables and charts to visually illustrate the key concepts.
Introduction to Needle Size Selection
Choosing the correct needle size for an injection is crucial for patient safety and treatment efficacy. An improper needle gauge can lead to complications ranging from discomfort and bruising to more serious issues like tissue damage or infection. The appropriate needle size directly impacts the injection process, ensuring the medication reaches its intended target with minimal harm.Selecting the correct needle size is paramount to patient well-being.
A needle that is too small may cause discomfort and hinder the flow of the medication, potentially requiring multiple attempts or increasing the risk of extravasation. Conversely, a needle that is too large can cause excessive tissue trauma, leading to bleeding, pain, and potentially damaging surrounding tissues. Proper needle size selection is a critical component of safe and effective injection practices.
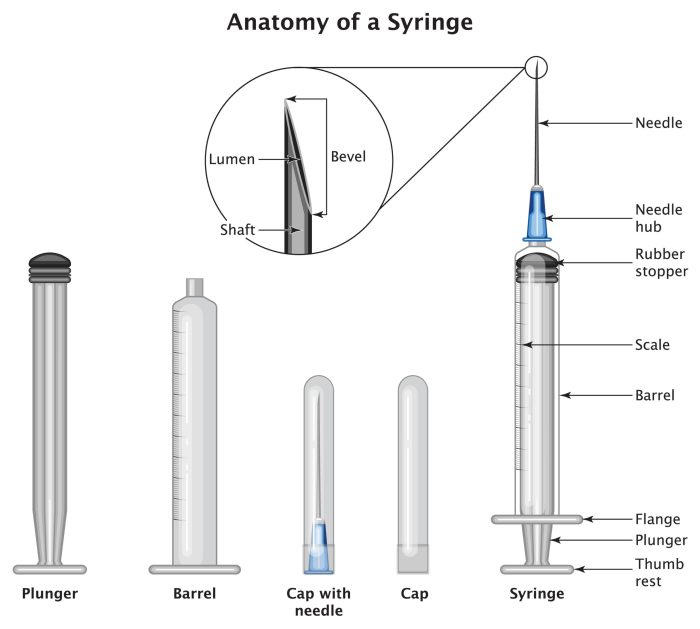
Needle Gauge and Diameter Relationship
Needle gauges and diameters are inversely related. A higher gauge number corresponds to a smaller diameter. This relationship is fundamental to understanding how needle size impacts the injection process. This knowledge allows healthcare professionals to select the optimal needle for different medications and patient populations.
Needle Gauge and Diameter Chart
| Needle Gauge | Approximate Diameter (mm) | Typical Uses |
|---|---|---|
| 25G | 0.36 mm | Small volumes of medication, intradermal injections, or when minimal tissue penetration is needed. |
| 23G | 0.48 mm | Subcutaneous injections, such as insulin or other medications requiring minimal tissue penetration. |
| 21G | 0.62 mm | Intramuscular injections, such as vaccinations or depot medications, and medications requiring deeper penetration. |
| 19G | 0.9 mm | Larger volume injections, intramuscular medications, or in situations where rapid absorption is desired. |
| 18G | 1.1 mm | Intravenous injections, blood draws, and medications that require significant penetration depth and rapid delivery. |
Understanding the correlation between needle gauge and diameter is vital for proper selection.
Potential Risks of Incorrect Needle Size Selection
Using an inappropriate needle size can lead to various adverse events. An excessively small needle can cause prolonged injection time, discomfort, and possible difficulty delivering the medication. Conversely, an oversized needle may cause excessive tissue trauma, potentially leading to complications like bleeding, bruising, or nerve damage. The selection of the appropriate needle gauge is critical for patient safety and the effectiveness of the treatment.
Factors Influencing Needle Size Choice
Choosing the right needle size for an injection is crucial for patient comfort and safety. Incorrect needle gauge can lead to complications like pain, bruising, and even tissue damage. Understanding the factors influencing needle size selection allows healthcare professionals to tailor injections to individual needs.The optimal needle size depends on several interconnected factors, including the medication’s viscosity, the injection site, the patient’s characteristics, and the type of injection.
Carefully considering these elements helps ensure a smooth and effective injection process.
Medication Viscosity and Needle Size
The viscosity of a medication significantly impacts needle size selection. Thicker medications, like some suspensions or viscous solutions, require larger-gauge needles to facilitate smooth flow. Smaller-gauge needles can cause resistance and potentially lead to discomfort or injection failure.
- Thicker medications, such as suspensions or viscous solutions, typically necessitate larger-gauge needles for efficient flow. A larger gauge facilitates easier and smoother injection, minimizing discomfort and improving patient experience.
- Conversely, thinner solutions like saline or certain medications require smaller-gauge needles to minimize discomfort and prevent unnecessary tissue trauma.
Types of Injections and Needle Size Requirements
Different types of injections have specific needle size recommendations. Intramuscular (IM) injections, for example, often require larger needles than subcutaneous (SC) injections to reach the targeted muscle layer. Subcutaneous injections, on the other hand, necessitate smaller needles to avoid excessive tissue damage.
- Intramuscular (IM) injections, targeting deeper muscle layers, usually demand larger needles to reach the desired site and administer the medication effectively.
- Subcutaneous (SC) injections, administered into the fatty tissue beneath the skin, require smaller needles to avoid damaging the underlying tissues.
- Intravenous (IV) injections are administered directly into a vein, and the needle gauge is determined by the size of the vein and the medication’s characteristics. A too-small needle may lead to extravasation or discomfort.
Needle Size Considerations for Different Patient Populations
Patient characteristics, such as age and body composition, also play a vital role in needle size selection. Children, for example, often require smaller needles due to their smaller body size and more delicate tissues. The elderly, on the other hand, may benefit from smaller needles to reduce the risk of bruising or discomfort.
Choosing the right needle size for an injection is crucial, especially when considering the different methods and potential side effects of procedures like total parenteral nutrition. For example, understanding the intricacies of total parenteral nutrition uses methods side effects can help you determine the appropriate needle gauge for optimal delivery. Ultimately, selecting the right needle size depends on the specific medication, patient factors, and the overall procedure.
This knowledge is vital to ensure safety and effectiveness.
- Children generally have smaller tissues and require smaller needles to minimize discomfort and prevent complications. Consider the specific needs of each child based on their age and size.
- The elderly may have more fragile tissues, so smaller needles can help minimize the risk of bruising or other adverse effects.
- Patients with conditions that affect their skin or underlying tissues, such as diabetes or peripheral neuropathy, may also require adjustments to needle size based on their individual needs and the advice of a healthcare professional.
Needle Gauge Comparison for Different Medication Viscosities
The following table provides a general comparison of needle gauges for various medication viscosities. Note that these are guidelines, and specific recommendations may vary depending on the medication and the individual patient.
| Medication Viscosity | Recommended Needle Gauge (Example) |
|---|---|
| Low Viscosity (e.g., Saline Solution) | 25-27 Gauge |
| Medium Viscosity (e.g., Aqueous Solutions) | 23-25 Gauge |
| High Viscosity (e.g., Suspensions, Some Injectable Oils) | 21-23 Gauge |
Note: Gauge numbers are inversely related to needle size. A higher gauge number corresponds to a smaller needle.
Choosing the right needle size for an injection is crucial, impacting comfort and potential complications. Factors like the medication type and the patient’s anatomy play a role. Understanding the potential for nerve damage, especially in situations like those discussed in the spotlight on phantom pain , emphasizes the importance of precision. A smaller needle, for example, can minimize discomfort and reduce the risk of nerve damage, making it a safer choice in many cases.
Ultimately, careful consideration of these factors ensures the most effective and least painful injection experience.
Methods for Determining Appropriate Needle Size
Choosing the right needle size is crucial for safe and effective injections. Incorrect needle gauge can lead to discomfort for the patient, hinder medication absorption, and even cause complications. Understanding the factors influencing needle size selection, along with the methods used to determine the appropriate gauge, empowers healthcare professionals to provide optimal patient care.Determining the correct needle size is a multi-faceted process that considers various factors.
It’s not a one-size-fits-all approach; the ideal needle size depends on the specific medication, the patient’s characteristics, and the injection site. This section details the methods used to select the appropriate needle gauge, offering a practical guide for healthcare professionals.
Medication Viscosity
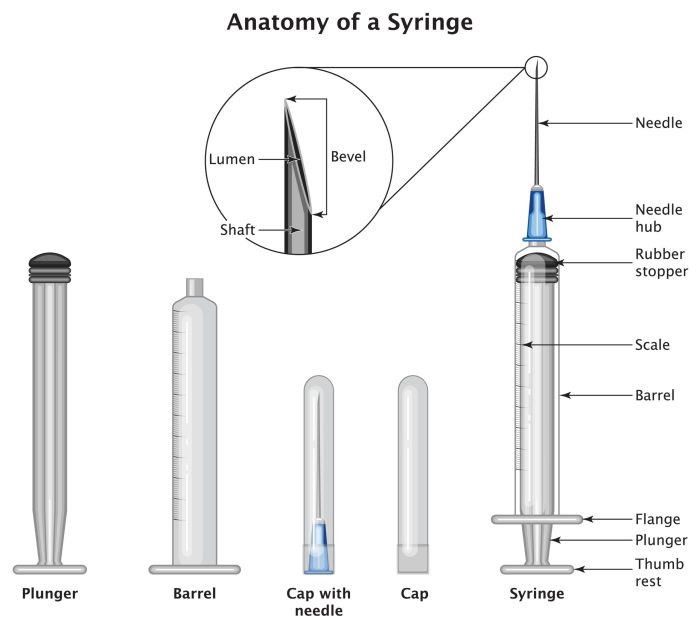
Medication viscosity significantly impacts needle selection. Highly viscous medications require larger gauges to facilitate smooth flow and minimize resistance during injection. This is because a larger gauge (smaller number) offers a larger lumen (opening) through which the medication can pass. Conversely, less viscous solutions can be administered using smaller needles, as the reduced resistance allows for effective delivery.
Consider the consistency of the medication—is it thick and syrupy, or thin and watery? This fundamental observation is essential for appropriate needle selection.
Patient Characteristics
Patient factors play a vital role in needle size determination. Patient size and weight are critical considerations. Smaller patients generally require smaller needles to minimize discomfort and potential complications. A larger needle in a small patient can cause tissue trauma. Additionally, consider the patient’s overall health condition and any pre-existing medical conditions that might influence needle selection.
For instance, patients with reduced subcutaneous fat may require smaller needles to avoid nerve or blood vessel damage. Careful assessment of the patient’s physical characteristics is essential.
Reference Charts and Tables, How to select the correct needle size for an injection
Reference charts and tables are valuable tools for quickly determining appropriate needle sizes. These resources often provide guidelines based on medication viscosity and patient characteristics. Such tables typically cross-reference medication type, desired injection site, and patient size with the recommended needle gauge. This organized format simplifies the selection process and reduces the risk of error. Examples of these charts may display different injection sites, medication types, and the corresponding recommended needle gauges.
Patient Size and Weight
Patient size and weight are crucial factors to consider. Generally, smaller patients necessitate smaller needles. A larger needle in a smaller patient can cause unnecessary tissue trauma, discomfort, and potentially more severe complications. This principle is crucial for minimizing harm and ensuring patient safety. For instance, a pediatric patient would require a significantly smaller needle than an adult patient receiving the same medication.
Injection Site Recommendations
The injection site also influences needle size selection. Different sites have varying thicknesses of subcutaneous tissue. This table provides general guidelines for needle size recommendations based on common injection sites:
| Injection Site | Needle Gauge Recommendation (Typical Range) |
|---|---|
Intramuscular (IM)
|
22-25G |
Intramuscular (IM)
|
22-25G |
Subcutaneous (SC)
|
25-27G |
Subcutaneous (SC)
|
25-27G |
Subcutaneous (SC)
|
25-27G |
| Intradermal | 25-27G |
This table offers a general guide. Individual patient needs and medication characteristics may necessitate adjustments to these recommendations. Consult relevant resources and guidelines for specific scenarios.
Safety Precautions and Considerations: How To Select The Correct Needle Size For An Injection
Choosing the right needle size is crucial for safe injections, but equally important are the safety precautions taken throughout the process. Neglecting these precautions can lead to serious complications for both the patient and the healthcare professional. This section Artikels essential safety measures and potential risks associated with improper needle selection.
Essential Safety Precautions During Needle Selection
Careful consideration of safety measures is paramount during the needle selection process. Adherence to these precautions minimizes the risk of accidental needle-stick injuries and other safety hazards.
- Use of Sharps Containers: Always use appropriate sharps containers for the disposal of used needles. These containers are specifically designed to prevent accidental punctures and should be readily available and accessible in all injection settings. Failure to use designated sharps containers increases the risk of needle-stick injuries for healthcare professionals and others who may come into contact with the discarded needles.
- Proper Handling of Needles: Avoid unnecessary handling of needles. Handle needles with care and use needle-less systems whenever possible. Improper handling of needles can result in accidental punctures or exposure to infectious materials.
- Pre-Injection Assessment: Assess the patient’s condition and the injection site before selecting a needle. Consider factors such as the patient’s skin type, the location of the injection site, and any pre-existing medical conditions. A thorough pre-injection assessment is vital for selecting an appropriate needle gauge and length, minimizing the risk of complications such as bleeding or discomfort.
- Needle Size Verification: Double-check the needle size against the prescribed dosage and the patient’s specific needs. Mismatching the needle size to the intended use can lead to inaccurate medication administration or complications. This step ensures the correct dose is delivered effectively.
Proper Disposal Methods for Used Needles
Proper disposal of used needles is critical for preventing accidental exposure to bloodborne pathogens and promoting environmental safety. Failure to follow proper disposal protocols can have serious consequences.
- Designated Sharps Containers: Used needles should be immediately placed into appropriately labeled and puncture-resistant sharps containers. These containers are specifically designed to prevent accidental punctures and should be readily available at all injection sites.
- Container Security: Ensure that sharps containers are securely sealed and disposed of according to local regulations. Improperly sealed containers can lead to leakage and potential contamination of the environment.
- Disposal Procedures: Follow the established protocols for the disposal of sharps containers. This may include specific guidelines for transporting, storing, and ultimately disposing of the containers, ensuring adherence to safety and environmental regulations.
Significance of Standard Precautions During Injection Procedures
Following standard precautions during injection procedures is essential for preventing the transmission of infectious diseases. These precautions protect both the patient and the healthcare professional from potential exposure to bloodborne pathogens.
- Hand Hygiene: Thoroughly wash hands with soap and water before and after each injection. This practice prevents the transmission of microorganisms and promotes aseptic conditions, reducing the risk of infection.
- Personal Protective Equipment (PPE): Wear appropriate personal protective equipment (PPE), such as gloves and gowns, during injection procedures to protect against exposure to potentially infectious materials. Proper use of PPE minimizes the risk of accidental exposure to bloodborne pathogens.
- Safe Injection Practices: Follow safe injection practices, such as using single-use needles and avoiding recapping needles. These practices are critical for preventing accidental needle-stick injuries and promoting a safe environment.
Potential Complications Arising from Improper Needle Selection
Choosing an inappropriate needle size can lead to several complications, impacting patient comfort and safety. Understanding these potential complications is vital for ensuring optimal patient care.
- Pain and Discomfort: An excessively large needle can cause significant pain and discomfort during injection. Conversely, an excessively small needle can hinder the proper flow of the injected substance.
- Hematoma Formation: Improper needle selection can increase the risk of hematoma formation at the injection site. This complication can lead to localized bleeding and bruising.
- Inaccurate Dosage Delivery: Choosing the wrong needle size can lead to inaccurate dosage delivery, potentially resulting in underdosing or overdosing of the medication. This can have serious consequences, especially in the case of medications with narrow therapeutic ranges.
- Infection: Improper needle selection can increase the risk of infection at the injection site. This is especially true when using a contaminated or reused needle.
Potential Hazards of Using an Inappropriate Needle Size
The following table Artikels the potential hazards associated with using an inappropriate needle size during injections.
| Needle Size Mismatch | Potential Hazards |
|---|---|
| Needle too large | Increased pain, discomfort, hematoma formation, tissue damage |
| Needle too small | Difficult injection, inaccurate dose delivery, potential for infection |
| Incorrect needle gauge for medication | Medication leakage, poor absorption, incorrect drug delivery |
Practical Application and Examples
Choosing the right needle size for an injection is crucial for patient safety and treatment efficacy. A precise needle gauge ensures the medication is delivered effectively, minimizing discomfort and potential complications. This section explores practical applications, case studies, and different injection techniques, highlighting the importance of selecting the correct needle size.Understanding the diverse needs of various injection types is vital.
Different medications, administration routes, and patient factors influence the optimal needle size selection. Proper application involves considering the viscosity of the solution, the depth of the injection site, and the patient’s specific anatomy.
Real-World Injection Examples
Selecting the appropriate needle size depends heavily on the type of injection. For example, administering insulin requires a very fine needle to minimize discomfort and prevent tissue damage. Subcutaneous injections, which deposit medication under the skin, necessitate a smaller needle size compared to intramuscular injections, which target muscle tissue. Intravenous injections, delivered directly into the bloodstream, use larger-gauge needles to accommodate the flow rate of the medication.
Case Studies of Incorrect Needle Size Selection
Using an incorrect needle size can have serious implications. For instance, employing a needle that is too large for a subcutaneous injection can cause excessive tissue trauma, leading to bruising, hematoma formation, and pain. Conversely, using a needle that is too small for an intramuscular injection can result in insufficient drug delivery, hindering treatment efficacy. A thorough understanding of the intended medication and administration route is essential to avoid such pitfalls.
Different Injection Techniques and Needle Sizes
Various injection techniques require specific needle sizes. Intradermal injections, delivered into the dermis layer, employ very small needles. Subcutaneous injections, targeting the fatty layer beneath the skin, use slightly larger needles. Intramuscular injections, penetrating deeper into muscle tissue, necessitate larger needles to ensure proper medication distribution. Intravenous injections, directly into a vein, require the largest gauge needles to facilitate fluid flow.
Needle Types and Recommended Sizes
Different needle types are designed for specific applications. Insulin needles, for example, are exceptionally thin and short, making them suitable for subcutaneous insulin administration. Subcutaneous needles are longer and have a wider range of gauges to accommodate different medications and injection sites. A detailed comparison table can aid in understanding the differences.
| Needle Type | Typical Gauge Range | Typical Length Range (mm) | Common Applications |
|---|---|---|---|
| Insulin Needles | 30-33G | 4-8mm | Administering insulin subcutaneously |
| Subcutaneous Needles | 25-27G | 6-12mm | Administering medications subcutaneously |
| Intramuscular Needles | 22-25G | 19-38mm | Administering medications intramuscularly |
| Intravenous Needles | 18-25G | 25-50mm | Administering medications intravenously |
Troubleshooting and Error Prevention
Choosing the right needle size for injections is crucial for patient safety and treatment efficacy. Mistakes can lead to discomfort, complications, and even serious adverse effects. This section focuses on common errors, troubleshooting steps, and preventative measures to ensure accurate needle selection.Incorrect needle size selection can result in various complications. A needle that’s too small may cause difficulty in administering the medication, leading to pain and potential tissue trauma.
Conversely, a needle that’s too large can cause excessive bleeding or tissue damage. Understanding potential errors and how to address them is essential for safe and effective injection practices.
Common Errors in Needle Size Selection
Common errors include misinterpreting patient factors, neglecting medication viscosity, and overlooking the specific injection site. Inaccurate estimations of patient size or body composition can lead to inappropriate needle selection. Likewise, failing to consider the viscosity of the medication, which impacts the ease of flow, can result in an unsuitable needle gauge. Poor site selection or improper technique can also contribute to complications.
Troubleshooting an Incorrect Needle Selection
Troubleshooting an incorrect needle selection involves a systematic approach to identify and rectify the error. Following these steps will help ensure the correct needle size is chosen.
- Assess the Situation: Carefully review the patient’s medical history, including any known sensitivities, comorbidities, and previous injection experiences. Determine the type of medication and its viscosity. Consider the injection site and its characteristics. Accurate documentation of all relevant information is critical.
- Identify the Discrepancy: Compare the chosen needle size with the recommended guidelines. Examine the patient’s anatomical characteristics and the medication’s physical properties. Identify if there are any inconsistencies between the selected needle size and these factors. Did the viscosity of the medication, patient size, or injection site affect the choice?
- Re-evaluate the Selection Criteria: If the initial needle size selection was incorrect, re-evaluate the factors that influenced the initial choice. Consult reference materials, such as drug information leaflets, medical guidelines, and established protocols, to ensure compliance with best practices. Determine if the chosen needle size meets the requirements for the particular medication and patient.
- Correct the Error: Select a needle size that aligns with the re-evaluated criteria. Consider the injection site, medication characteristics, and patient factors. If necessary, consult with a healthcare professional to ensure the correct needle size is used. Confirm the revised selection against the appropriate guidelines and standards.
- Verify the Corrected Selection: Double-check the chosen needle size against the established guidelines. Confirm that the selected needle size aligns with the medication’s characteristics and the patient’s needs. This step ensures that the selected needle size is appropriate for the specific circumstances.
Preventing Mistakes in Needle Size Selection
Prevention is key to avoiding errors in needle size selection. Developing a systematic approach and adhering to established protocols can minimize the risk of complications.
Choosing the right needle size for an injection depends heavily on the medication and the patient’s anatomy. For example, administering a medication through a bronchopleural fistula, a hole between the lung and the chest cavity, what is a bronchopleural fistula , requires a different needle gauge than a standard intramuscular injection. Ultimately, precision in needle size selection is crucial for both patient comfort and the effectiveness of the treatment.
- Establish Clear Protocols: Develop and implement comprehensive protocols for needle size selection, incorporating guidelines for various medications, patient types, and injection sites. These protocols should be easily accessible and regularly reviewed for updates.
- Regular Training and Education: Provide ongoing training and education for healthcare professionals on proper needle size selection techniques. Regular updates on best practices and new guidelines are essential to maintaining competency.
- Utilize Standardized Charts and Tools: Implement standardized charts, tables, or software applications to aid in the selection process. These tools can provide a visual guide and streamline the decision-making process. Use of reliable reference materials is also essential.
- Documentation and Review: Maintain detailed documentation of needle size selection, including patient information, medication details, and rationale for the chosen size. Regularly review these records to identify patterns and areas for improvement.
Assessing and Correcting Errors
A structured approach to assessing and correcting errors is crucial for preventing recurrence. This involves a thorough review of the entire process, identifying the root cause of the error, and implementing corrective actions. This ensures continuous improvement in injection practices.
Troubleshooting Flowchart
[A flowchart illustrating the troubleshooting process would be displayed here. It would visually guide users through the steps described above, showing decision points and potential outcomes. For example, it could start with a question like “Is the selected needle size appropriate for the patient’s size and the medication?” with branches leading to “Yes” (correct choice) or “No” (inappropriate choice), and then subsequent questions to help identify the reason for the discrepancy.]
Resources and Further Reading

Deepening your knowledge about selecting the right needle size for injections requires exploring various reliable resources. This section provides valuable pathways for further learning, encompassing reputable organizations, informative articles, and insightful websites. Understanding the diverse perspectives and guidelines offered by these resources will enhance your understanding and practical application of safe injection techniques.
Reputable Organizations and Guidelines
Numerous organizations contribute to the development and dissemination of best practices in healthcare, including injection techniques. These organizations often publish guidelines, protocols, and recommendations for needle size selection, which are crucial for ensuring patient safety and procedural efficacy.
- The Centers for Disease Control and Prevention (CDC) provides comprehensive information on infection control and safe injection practices. Their guidelines often incorporate evidence-based recommendations on needle size selection tailored to different scenarios and patient populations.
- The World Health Organization (WHO) offers global health guidelines and recommendations. These encompass diverse injection practices and emphasize safety protocols, including appropriate needle gauge selection, based on scientific evidence and practical experience.
- Professional medical organizations, such as the American Society of Anesthesiologists (ASA), offer specific guidelines and recommendations tailored to the needs of their respective specialties. These organizations contribute to standardized practices and ensure consistency in medical care.
Relevant Articles and Publications
Staying updated with the latest research and publications is crucial for professionals in the healthcare field. These resources often present the most recent findings, research results, and evidence-based approaches to injection procedures, including the appropriate needle gauge selection.
- Numerous peer-reviewed journals, including the “Journal of the American Medical Association” (JAMA) and “The Lancet,” publish articles on various aspects of healthcare. These publications provide access to recent research and clinical trials concerning injection techniques, including discussions of optimal needle size for different scenarios.
- Search databases like PubMed can help locate relevant research articles on injection techniques and appropriate needle gauge selection for specific purposes. This research is essential for staying current with the latest findings and evidence-based recommendations.
Websites Offering Information on Injection Techniques
Reliable websites offer a wealth of information on injection procedures, including the critical aspect of selecting the correct needle size. These resources are valuable tools for enhancing knowledge and proficiency in safe and effective injection practices.
- Websites from reputable medical institutions, such as the Mayo Clinic and Cleveland Clinic, provide detailed information on various injection techniques and the principles of selecting the correct needle gauge. These sites are excellent resources for professionals and patients seeking to enhance their knowledge.
- Online medical training platforms often offer courses and modules dedicated to injection techniques. These interactive resources enable learners to explore practical aspects of selecting appropriate needle gauges and performing injections safely.
Recommended Resources
The table below presents a summary of recommended resources for learning about needle size selection and injection procedures. These resources are carefully curated for their reliability and the comprehensive information they offer.
| Resource | Description | Website/Publication |
|---|---|---|
| Centers for Disease Control and Prevention (CDC) | Comprehensive guidelines on infection control and safe injection practices. | cdc.gov |
| World Health Organization (WHO) | Global health guidelines and recommendations for injection techniques and safety. | who.int |
| American Society of Anesthesiologists (ASA) | Specific guidelines and recommendations tailored to anesthesiology practices. | asa.org |
| Mayo Clinic | Detailed information on injection techniques and needle gauge selection. | mayoclinic.org |
| Cleveland Clinic | Extensive information on various medical procedures, including injections. | clevelandclinic.org |
Summary
In conclusion, selecting the right needle size for an injection is a critical step in ensuring patient safety and successful treatment outcomes. By understanding the factors influencing needle size selection, the methods for determining the appropriate gauge, and the safety precautions involved, healthcare professionals can minimize risks and maximize positive outcomes. This guide provides a comprehensive overview, offering practical tools and examples to help you navigate this essential aspect of injection procedures.
Remember to prioritize patient safety in every injection.