Surgery not needed for rotator cuff tears is a growing area of interest for those experiencing pain and discomfort in their shoulders. This in-depth exploration delves into the various non-surgical treatment options available, providing a comprehensive overview of how to effectively manage rotator cuff tears without resorting to surgery. From physical therapy and medication to lifestyle modifications and alternative therapies, we’ll uncover the strategies that can lead to recovery and long-term well-being.
This post explores the conditions where surgery isn’t necessary for rotator cuff tears, providing a detailed look at non-surgical treatment options. We will cover everything from conservative treatments and physical therapy to activity modifications and the role of patient expectations in the decision-making process.
Introduction to Rotator Cuff Tears
A rotator cuff tear is a common injury affecting the shoulder joint. It occurs when one or more of the tendons that make up the rotator cuff are damaged or torn. These tendons surround the shoulder joint, providing stability and enabling a wide range of motion. Understanding the causes, symptoms, and treatment options is crucial for effective management and recovery.The rotator cuff is a complex group of muscles and tendons that surround the shoulder joint.
Its primary function is to stabilize the shoulder, allowing for a wide range of movement. Tears can occur due to a variety of factors, often combining repetitive stress, acute trauma, or the natural aging process.
So, you’ve got a rotator cuff tear, and you’re thinking surgery is the only way? Think again! Often, conservative treatments like physical therapy and rest are enough to manage the pain and discomfort associated with these tears. This can be especially important for women, as low testosterone in women can impact recovery from injuries and affect muscle strength.
While surgery might be necessary in severe cases, it’s definitely not the first resort for most rotator cuff tears.
Common Causes of Rotator Cuff Tears
Rotator cuff tears are often the result of a combination of factors. Repetitive overhead movements, such as those performed by athletes or workers in certain professions, can put significant stress on the rotator cuff tendons, leading to micro-tears over time. Acute trauma, such as a fall onto an outstretched arm, can cause a sudden and severe tear. Furthermore, the natural aging process can contribute to the degeneration of the tendons, making them more susceptible to tears.
The presence of underlying conditions like arthritis can also increase the risk of rotator cuff tears.
Symptoms of Rotator Cuff Tears
Individuals with rotator cuff tears may experience a variety of symptoms. Pain, often described as a dull ache or sharp stabbing sensation, is a common symptom. This pain may be localized around the shoulder or radiate down the arm. Weakness in the shoulder and arm is another common symptom. Limited range of motion, particularly in overhead movements, is frequently observed.
Night pain, which can interfere with sleep, is also a possible symptom. These symptoms can vary in intensity and may be more pronounced with certain activities or positions.
Types of Rotator Cuff Tears
Rotator cuff tears are categorized as either partial-thickness or full-thickness tears. A partial-thickness tear involves only a portion of the tendon being damaged, while a full-thickness tear extends completely through the tendon. The extent of the tear impacts the treatment options and prognosis. Partial tears may heal with conservative management, while full-thickness tears often require more aggressive intervention.
Non-Surgical Treatments for Rotator Cuff Tears
Non-surgical treatment options for rotator cuff tears are often explored as a first-line approach. These options aim to manage pain, reduce inflammation, and improve function without the need for surgery. Physical therapy plays a crucial role in restoring strength and range of motion. Rest and activity modification are also essential components of non-surgical management. Medications, such as pain relievers and anti-inflammatory drugs, can help to alleviate pain and inflammation.
Injections, such as corticosteroid injections, may also be considered to reduce inflammation and pain.
Comparison of Common Non-Surgical Treatment Options
| Treatment Type | Description | Duration | Success Rate | Potential Side Effects |
|---|---|---|---|---|
| Physical Therapy | Exercises and stretches to improve strength, flexibility, and range of motion. | Variable, typically several weeks to months. | High, depending on the severity of the tear. | Possible muscle soreness, discomfort during exercises. |
| Rest and Activity Modification | Avoiding activities that aggravate the pain and inflammation. | Variable, depending on the severity and individual response. | Moderate, often necessary in conjunction with other treatments. | Potential for deconditioning if not managed properly. |
| Medications (e.g., NSAIDs) | Pain relievers and anti-inflammatory drugs to reduce pain and inflammation. | Variable, as prescribed by a physician. | Moderate, may not address the underlying cause of the tear. | Potential for gastrointestinal upset, kidney problems with long-term use. |
| Injections (e.g., Corticosteroids) | Injections to reduce inflammation and pain. | Immediate relief, but effects may be temporary. | Moderate, often used in conjunction with other treatments. | Potential for joint infection, tendon rupture, and temporary increase in pain. |
Conservative Treatment Options
Dealing with a rotator cuff tear doesn’t always necessitate surgery. Many individuals find relief and recovery through conservative treatment methods. These approaches focus on pain management, restoring function, and promoting healing without invasive procedures. Understanding these options is crucial for making informed decisions about your care.
Non-Surgical Pain Management Techniques
Conservative treatment often starts with managing pain and inflammation. Rest, ice, compression, and elevation (RICE) are frequently employed. Applying ice packs to the affected area for 15-20 minutes at a time, several times a day, can help reduce swelling and pain. A compression bandage can also aid in minimizing inflammation. Elevation helps by reducing the pooling of blood in the injured area.
While rest is crucial, complete immobilization is often discouraged, as it can lead to stiffness and reduced range of motion. A balance between rest and controlled movement is vital.
Physical Therapy Exercises
Physical therapy plays a pivotal role in conservative treatment. Specific exercises are tailored to strengthen the rotator cuff muscles, improve range of motion, and restore functionality. These exercises are designed to gradually increase the load on the muscles, promoting healing and preventing further injury. Progressive exercises are essential to avoid overexertion.
| Exercise Name | Description | Sets/Reps | Frequency |
|---|---|---|---|
| Pendulum Exercises | Gentle arm swings to improve shoulder mobility. Start with small circles and gradually increase the range. | 3 sets of 10-15 repetitions, each direction | 2-3 times daily |
| Isometric Strengthening Exercises | Exercises involving holding a position against resistance without moving the joint. | 3 sets of 10-15 seconds hold | 2-3 times daily |
| Resistance Band Exercises | Using resistance bands to progressively strengthen the rotator cuff muscles. | 2-3 sets of 10-15 repetitions | 1-2 times daily |
| Scapular Exercises | Exercises targeting the muscles around the shoulder blade to improve posture and support the shoulder joint. | 2 sets of 10-15 repetitions | 1-2 times daily |
Medications for Pain Management
Various medications can help manage the pain associated with a rotator cuff tear. Over-the-counter pain relievers, such as ibuprofen or naproxen, can be effective in reducing inflammation and pain. In some cases, a doctor might prescribe stronger pain relievers or anti-inflammatory medications to manage more severe pain. It’s crucial to follow the prescribed dosage and seek guidance from a healthcare professional.
Applying Ice and Heat
Proper application of ice and heat can significantly impact recovery. Ice is typically used in the initial stages of injury to reduce inflammation and pain. Apply an ice pack to the affected area for 15-20 minutes at a time, several times a day. Using a thin cloth or towel between the ice pack and skin is crucial to prevent skin irritation.
Sometimes, a rotator cuff tear doesn’t require surgery. Learning about alternative treatments can be incredibly helpful, and understanding the various options available for managing these types of injuries is key. For instance, exploring non-surgical approaches to gynecological issues is also important, and resources like gynecology surgery and procedures 101 can provide valuable insight into the different surgical and non-surgical paths available.
Ultimately, making informed decisions about your health, whether it’s for rotator cuff tears or other conditions, is crucial.
Heat is often used later in the recovery process to increase blood flow and promote healing. Applying a heating pad or warm compress for 15-20 minutes at a time, several times a day, can aid in easing muscle stiffness and soreness.
Non-Surgical Management Strategies
Avoiding surgery for a rotator cuff tear is often a desirable goal for patients. Non-surgical management strategies focus on minimizing pain, improving function, and promoting healing without the need for invasive procedures. These approaches can be highly effective for individuals with less severe tears or those who are not ideal candidates for surgery. Understanding the different strategies and their potential benefits and limitations is crucial for making informed decisions about treatment.
So, you’ve got a rotator cuff tear, and surgery isn’t necessarily the only answer. Sometimes, focusing on alternative treatments like gentle exercises and physical therapy can be just as effective. Plus, if you’re experiencing a dry scalp, there are plenty of natural remedies you can try at home, like using a homemade apple cider vinegar rinse or applying a nourishing oil mask.
Home remedies for dry scalp can be surprisingly helpful in managing discomfort, and similar approaches can sometimes help with rotator cuff issues too. Ultimately, a holistic approach often yields the best results, even when it comes to things like rotator cuff tears.
Activity Modification
Modifying activities that exacerbate pain is a cornerstone of non-surgical rotator cuff tear management. This involves identifying specific movements or tasks that cause discomfort and finding alternative methods to complete those tasks. For example, if overhead reaching aggravates pain, using tools with longer handles or employing assistive devices can reduce strain on the injured area. Gradual and progressive return to activities, under the guidance of a physical therapist, is essential to prevent re-injury.
Pain should be a primary guide in determining activity modification; pushing through pain can hinder healing.
Proper Posture and Ergonomics
Maintaining proper posture and ergonomic principles is vital for preventing rotator cuff strain. Poor posture can lead to muscle imbalances and increased stress on the shoulder joint, potentially exacerbating existing tears or hindering healing. This includes maintaining a neutral spine alignment, using proper sitting posture, and utilizing ergonomic tools and equipment at work or during daily activities. Regular reminders and adjustments to posture can help prevent further issues.
Ergonomic assessments can identify specific issues related to workplace setups.
Bracing and Supportive Devices
Various bracing and supportive devices are available to provide targeted support and stability to the shoulder. These devices can help reduce pain, promote healing, and allow for a more comfortable range of motion. Shoulder slings, wraps, and braces are examples of common supportive devices. Each device may provide varying levels of support, depending on the individual needs and characteristics of the tear.
Slings are often used initially to allow the shoulder to rest.
Benefits and Limitations of Strategies
| Strategy | Benefits | Limitations ||—|—|—|| Activity Modification | Reduced pain, prevention of further injury, and gradual return to function. | Requires patient self-monitoring and discipline, potential for frustration in achieving desired activity levels, and may not be effective for severe tears. || Proper Posture and Ergonomics | Prevention of further injury, reduced stress on the shoulder joint, and potential for long-term pain relief.
| Requires conscious effort and practice, may not be effective in cases with significant postural abnormalities, and may require assistive devices or ergonomic modifications. || Bracing and Supportive Devices | Reduced pain, improved stability, and enhanced support during daily activities. | Potential for skin irritation or discomfort, limited mobility in some devices, and not a replacement for other treatments. |
When Surgery is NOT Needed: Surgery Not Needed For Rotator Cuff Tears
Choosing between surgery and non-surgical treatment for a rotator cuff tear hinges on careful consideration of several factors. The decision isn’t solely based on the severity of the tear, but also on the patient’s lifestyle, expectations, and overall health. This section will delve into the criteria for determining when surgery is unnecessary and the factors influencing the choice of non-surgical management strategies.Non-surgical treatment options for rotator cuff tears are often effective for managing pain and restoring function, particularly in specific circumstances.
This approach prioritizes conservative methods to address the underlying issues and allow the body to heal naturally.
Criteria for Determining Non-Surgical Treatment
Determining whether surgery is necessary for a rotator cuff tear involves evaluating various factors beyond just the tear’s size. The presence of significant pain and functional limitations are key considerations, but the tear’s location and the patient’s overall health also play a role. A comprehensive assessment by a healthcare professional is crucial in making this decision.
Factors Influencing the Decision Against Surgery
Several factors influence the decision to pursue non-surgical treatment. These include the size and location of the tear, the patient’s age and overall health, and the presence of other conditions that might affect the healing process. Furthermore, the patient’s level of activity and their expectations regarding recovery play a significant role. For example, a patient with a small, asymptomatic tear who leads a sedentary lifestyle might be an excellent candidate for non-surgical treatment.
Comparison of Non-Surgical Treatment Situations
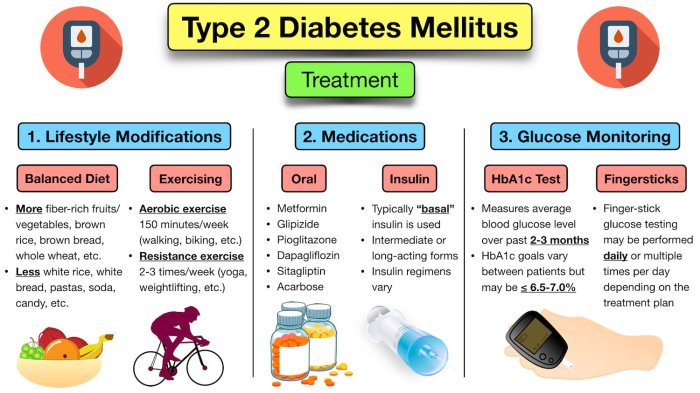
Non-surgical management strategies encompass a range of approaches, each tailored to specific patient needs. Physiotherapy plays a crucial role in restoring strength and flexibility, while pain management strategies, such as medication and injections, can help alleviate discomfort. Lifestyle modifications, such as activity modification and weight management, can also contribute to successful outcomes.
- Physiotherapy: This is often the cornerstone of non-surgical treatment, focusing on strengthening the muscles surrounding the shoulder joint. Exercises are tailored to the individual’s needs and progress, aiming to improve range of motion and reduce pain.
- Pain Management: Non-steroidal anti-inflammatory drugs (NSAIDs) and corticosteroid injections can help alleviate pain and inflammation. However, these are often used in conjunction with other treatments, and their use is carefully monitored by a healthcare professional.
- Lifestyle Modifications: Avoiding activities that aggravate the condition and maintaining a healthy weight are crucial for healing. Modifying activities and employing proper lifting techniques can significantly reduce strain on the rotator cuff.
Role of Patient Expectations and Lifestyle
Patient expectations and lifestyle significantly influence the choice between surgical and non-surgical treatments. Patients with realistic expectations and a willingness to participate actively in their rehabilitation program are more likely to achieve favorable outcomes with non-surgical approaches. A sedentary lifestyle might be better suited for non-surgical management compared to a physically demanding job or athletic lifestyle.
Characteristics of Good Candidates for Non-Surgical Treatment
Patients who are good candidates for non-surgical treatment typically have smaller tears, minimal pain, and a willingness to engage in a structured rehabilitation program. They often have a lower level of activity compared to those requiring surgical intervention. Their overall health is generally good, and they understand the potential limitations and time commitment of non-surgical rehabilitation.
Examples of Successful Non-Surgical Management
Numerous cases demonstrate the effectiveness of non-surgical treatment in managing rotator cuff tears. A patient with a moderate-sized tear who diligently followed a physiotherapy program and modified their activities experienced significant pain relief and improved shoulder function within several months. Another example includes a patient with a small, asymptomatic tear who opted for a conservative approach and achieved satisfactory results without undergoing surgery.
Alternatives to Surgery for Rotator Cuff Tears

Choosing the right path for rotator cuff tears is a personal decision. Many patients, after careful consideration of their symptoms, lifestyle, and overall health, opt for non-surgical interventions. This approach allows them to explore healing strategies beyond the operating room, potentially avoiding the risks and recovery time associated with surgery. These alternatives often involve a multifaceted approach combining various therapies to manage pain, improve function, and promote tissue healing.
Reasons for Choosing Alternatives
Patients may choose non-surgical options for a variety of reasons. These may include a desire to avoid the potential complications of surgery, a preference for less invasive treatment, concerns about the recovery period associated with surgery, or a personal belief in the effectiveness of alternative therapies. Some patients may also have pre-existing medical conditions that make surgery a higher risk.
Ultimately, the decision to pursue non-surgical treatment is a personal one, made in consultation with a healthcare professional.
Different Types of Alternative Therapies
A range of alternative therapies can play a significant role in managing rotator cuff tears. These therapies are often integrated with conventional physical therapy and may include:
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body. Acupuncture is believed to stimulate the flow of energy, reduce pain, and promote healing. Some studies suggest that acupuncture can help reduce pain and improve function in patients with musculoskeletal conditions.
- Massage Therapy: Massage therapy aims to release muscle tension, improve blood flow, and reduce pain. Different types of massage techniques, such as deep tissue massage, trigger point therapy, and sports massage, can target specific areas affected by the rotator cuff tear. Regular massage sessions can help alleviate pain, increase flexibility, and improve range of motion.
- Physical Therapy: While often considered a conventional treatment, physical therapy plays a vital role in many non-surgical approaches. A physical therapist will create a tailored exercise program to strengthen the muscles surrounding the rotator cuff, improve range of motion, and restore function. The goal is to improve the patient’s ability to perform daily activities without pain.
- Nutritional Changes: Proper nutrition plays a key role in overall health and healing. A diet rich in anti-inflammatory foods and nutrients that support tissue repair can contribute to a faster recovery. This might include incorporating foods rich in vitamins, minerals, and omega-3 fatty acids.
Success Stories with Alternative Therapies
While anecdotal evidence can be compelling, scientific research plays a crucial role in evaluating the effectiveness of alternative therapies. Success stories often involve a combination of therapies and a patient’s commitment to their treatment plan. For example, a patient experiencing moderate rotator cuff tear pain might find relief through a regimen that includes acupuncture, massage, and specific strengthening exercises prescribed by a physical therapist.
Sustained improvement over time often relies on consistency and a proactive approach to healing.
Potential Risks and Benefits of Alternative Therapies
Alternative therapies, while promising, come with potential risks and benefits.
- Benefits: Many patients find relief from pain and improved function through alternative therapies. These approaches often integrate well with conventional physical therapy, offering a holistic approach to healing.
- Risks: While generally considered safe, some alternative therapies can pose risks if not performed by qualified practitioners. For example, improper acupuncture techniques can lead to infection or nerve damage. Carefully consider the practitioner’s credentials and experience before undergoing any alternative therapy.
Comparison of Alternative Therapies, Surgery not needed for rotator cuff tears
| Therapy | Description | Potential Benefits | Potential Risks |
|---|---|---|---|
| Acupuncture | Insertion of thin needles into specific points on the body. | Potential pain relief, improved blood flow, and promotion of healing. | Infection, nerve damage, allergic reaction to needles. |
| Massage Therapy | Techniques to release muscle tension, improve blood flow, and reduce pain. | Pain relief, increased flexibility, improved range of motion. | Bruising, soreness, potential for injury if performed improperly. |
| Physical Therapy | Tailored exercise program to strengthen surrounding muscles, improve range of motion. | Improved strength, flexibility, functional improvement. | Potential for muscle soreness, need for consistent commitment. |
| Nutritional Changes | Diet rich in anti-inflammatory foods and nutrients supporting tissue repair. | Improved overall health, potentially faster recovery. | Potential for nutritional deficiencies or adverse reactions to dietary changes. |
Prognosis and Long-Term Outcomes

Navigating the path to recovery from a rotator cuff tear without surgery requires a nuanced understanding of potential outcomes. Factors such as the severity of the tear, the patient’s age and activity level, and their adherence to the treatment plan all play a significant role in determining the long-term success of conservative management. This section delves into the critical elements of prognosis and long-term functional outcomes for those choosing non-surgical intervention.
Factors Influencing Prognosis
Various factors influence the success of non-surgical treatment for rotator cuff tears. These include the size and location of the tear, the presence of other associated conditions, and the patient’s overall health. A smaller, less-displaced tear in a younger, more active patient has a better chance of healing without surgery. Conversely, a larger, more extensive tear in an older individual with comorbidities may require a more cautious approach and a longer recovery period.
Importance of Patient Compliance
Patient compliance with the prescribed non-surgical treatment plan is paramount for achieving positive outcomes. This includes diligently performing exercises, maintaining prescribed rest periods, and adhering to any dietary or lifestyle modifications. A patient’s commitment to the rehabilitation program directly correlates with the likelihood of successful healing and improved functional capacity. Without consistent effort, the healing process can be significantly hampered, potentially prolonging recovery and leading to less favorable outcomes.
Long-Term Functional Outcomes
Data from various studies indicate that a substantial number of patients experience significant improvement in their functional capacity and pain levels following non-surgical management. However, the extent of improvement can vary depending on the factors mentioned earlier. For instance, patients with smaller tears, a younger age, and consistent adherence to treatment are more likely to regain a substantial portion of their pre-injury function.
Longitudinal studies have demonstrated that many individuals with rotator cuff tears can return to their pre-injury activity levels with conservative management, though the recovery timeline can differ.
Potential Complications of Prolonged Non-Surgical Treatment
While non-surgical treatment is often a viable option, prolonged periods without surgical intervention can lead to potential complications. These may include persistent pain, limited range of motion, and progressive weakness. Furthermore, the tear may not fully heal, leading to ongoing discomfort and decreased functional ability. In such cases, the patient may need to explore surgical options to achieve better long-term outcomes.
It is important to monitor the patient’s condition closely during the non-surgical treatment phase and consider surgical intervention if the conservative approach is not yielding satisfactory results.
Comparison of Surgical vs. Non-Surgical Outcomes
Comparing the long-term outcomes of surgery and non-surgical management for rotator cuff tears is complex and not always straightforward. While surgery can often provide rapid restoration of function, it carries the risk of complications, such as infection or nerve damage. Non-surgical treatment, on the other hand, is less invasive but may require a longer recovery period and may not always result in complete restoration of function.
The decision to proceed with either surgical or non-surgical management should be made in consultation with a medical professional who can assess the specific circumstances of the individual case. Ultimately, the optimal approach is determined by factors such as the size and location of the tear, the patient’s age and activity level, and the patient’s overall health. In some instances, a combination of both approaches may be beneficial.
Wrap-Up
In conclusion, managing rotator cuff tears without surgery is a viable and often preferred path for many individuals. This approach considers various factors, including the patient’s overall health, lifestyle, and expectations. The exploration of non-surgical strategies, from conservative treatments to alternative therapies, offers a comprehensive perspective on managing rotator cuff tears effectively. Ultimately, the decision to pursue non-surgical options hinges on a careful evaluation of individual circumstances and a strong partnership between the patient and healthcare provider.