What are these spots on my MRI? This question is understandably unsettling, and it’s completely valid to want clear answers about these markings. An MRI, a powerful diagnostic tool, uses magnetic fields and radio waves to create detailed images of the body’s internal structures. Understanding the purpose of the scan, the types of scans, and common reasons for getting one is crucial for interpreting any results, including those potentially revealing spots.
This exploration will cover the normal appearances of various tissues and structures, as well as the importance of your medical history in understanding the significance of any anomalies.
We’ll delve into how spots or abnormalities manifest on MRI images, examining various types based on location and appearance. Potential causes, ranging from benign to malignant conditions, will be explored, along with factors influencing the spot’s appearance. Different types of lesions, their characteristics, and how their presence impacts the diagnostic process will be discussed. Ultimately, this information is vital to understanding the potential severity of the spots, considering factors like size, shape, location, and surrounding tissue changes.
We’ll also analyze how the context of your symptoms plays a role in assessing the significance of these findings.
Understanding the Context
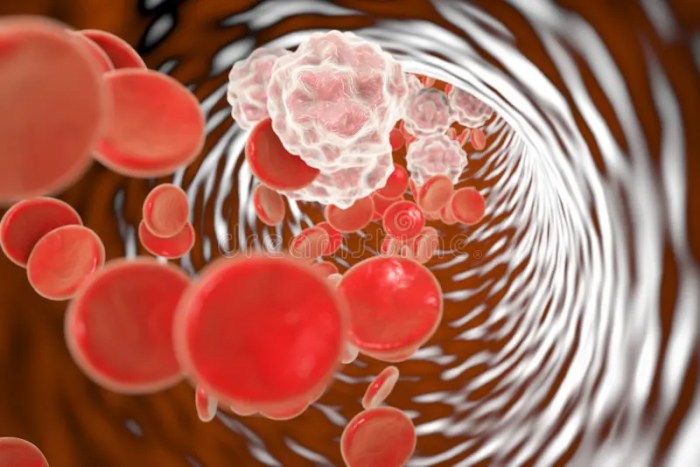
Magnetic Resonance Imaging (MRI) is a powerful diagnostic tool used to visualize the internal structures of the body without the need for invasive procedures like surgery. It utilizes a powerful magnetic field and radio waves to create detailed images of tissues and organs, providing crucial information for medical diagnoses and treatment planning. This allows doctors to see soft tissues, like muscles, ligaments, tendons, and organs, in great detail, which often isn’t possible with X-rays or CT scans.MRI technology relies on the magnetic properties of hydrogen atoms, which are abundant in the body’s tissues.
The technique essentially maps the distribution of hydrogen atoms, revealing anatomical structures and any abnormalities. This non-invasive approach minimizes potential risks compared to other imaging methods.
Types of MRI Scans and Applications
Different types of MRI scans are tailored for specific purposes. A basic anatomical MRI provides a comprehensive view of the region of interest, while specialized scans can target specific tissues or functions. For example, functional MRI (fMRI) measures brain activity by detecting changes in blood flow, crucial for understanding neurological processes. Diffusion-weighted imaging (DWI) highlights the movement of water molecules within tissues, assisting in identifying areas of acute injury or stroke.
Common Reasons for an MRI
Various medical conditions necessitate an MRI scan. Joint pain, suspected fractures, or ligament tears often warrant MRI to assess soft tissue damage. Neurological issues, such as tumors, strokes, or multiple sclerosis, can be diagnosed with the help of MRI. Abdominal or pelvic pain may also prompt an MRI to visualize organs and identify potential abnormalities.
Tissues and Structures Visible on an MRI
MRI allows for detailed visualization of a wide range of tissues and structures. Bones, though visible, are not the primary focus of an MRI, as soft tissue is the forte. The detailed images show ligaments, tendons, muscles, organs, blood vessels, and the spinal cord. The brain, heart, and other vital organs are all clearly visible. The resolution is high enough to identify small lesions or abnormalities.
Normal Appearance of Structures on an MRI
The normal appearance of structures on an MRI varies based on the region being examined. For example, the normal brain appears with smooth contours and consistent tissue density. Healthy spinal cord tissue should show a uniform signal. Ligaments and tendons should exhibit a consistent signal intensity without any tears or abnormalities. Deviations from these norms may indicate underlying pathologies.
Importance of Patient Medical History
Understanding the patient’s medical history is crucial in interpreting MRI findings. Previous surgeries, injuries, or existing conditions can significantly influence the interpretation of the images. For instance, a patient with a history of osteoarthritis will likely exhibit different MRI findings in their joints compared to a patient without a history of the condition. A thorough medical history is critical for providing accurate diagnoses and treatment plans.
Typical Anatomical Structures in a Head MRI
| Structure | Description |
|---|---|
| Brain | The central organ of the nervous system, composed of gray and white matter, including various lobes. |
| Cerebellum | Located beneath the occipital lobe, responsible for motor control and coordination. |
| Brainstem | Connects the brain to the spinal cord, regulating vital functions like breathing and heart rate. |
| Skull | The bony structure surrounding the brain, visible as a dense structure on MRI. |
| Meninges | The membranes surrounding the brain and spinal cord, which can be visualized on MRI. |
| Blood Vessels | Visible as vessels with varying signal intensities. |
Identifying Potential Anomalies: What Are These Spots On My Mri

MRI scans provide detailed images of the body’s internal structures, revealing potential abnormalities that might be missed by other imaging techniques. Understanding how these abnormalities appear, their potential causes, and associated characteristics is crucial for accurate diagnosis and appropriate treatment. This section delves into the specifics of identifying anomalies, focusing on their appearance, location, and underlying causes.Spot-like abnormalities on MRI scans can arise from various sources, ranging from benign conditions to potentially serious malignancies.
Careful analysis of the appearance, location, and surrounding tissue characteristics is essential for differentiating between these possibilities.
Appearance of Abnormalities on MRI
MRI scans use different contrasts to highlight various tissues and structures. Abnormalities appear as areas of differing signal intensity, which can manifest as bright or dark spots relative to the surrounding healthy tissue. The appearance is often dependent on the specific type of tissue affected and the nature of the underlying condition. These signal intensity variations are crucial for differentiating between various conditions.
Types of Abnormalities and Locations
Abnormalities can appear in diverse locations throughout the body. Their appearance can vary significantly, ranging from small, well-defined spots to larger, more diffuse areas. Examples include:
- Brain: Lesions in the brain might appear as bright or dark spots depending on the type of tissue involved. Small, well-defined bright spots can suggest acute inflammation, while larger, more diffuse dark areas could be indicative of tissue death. Examples include strokes, tumors, or abscesses.
- Spine: Spots on spinal MRI scans can be indicative of herniated discs, tumors, or infections. These abnormalities can be characterized by varying signal intensities, which can be influenced by the presence of fluid or inflammation. Their shape and size are also key to understanding the nature of the condition.
- Liver: Focal lesions in the liver, appearing as spots or nodules, might be indicative of cysts, hemangiomas, or tumors. The characteristics of the spots, such as their margins and internal structure, are crucial in differentiating between these various possibilities.
Possible Causes of Abnormalities
Spot-like abnormalities can stem from a range of conditions, both benign and malignant.
- Benign Conditions: Examples include cysts, which are fluid-filled sacs, or hemangiomas, which are benign tumors composed of blood vessels. These often present as well-defined, rounded spots on MRI scans.
- Malignant Conditions: Cancers, like gliomas in the brain, can manifest as spots with irregular shapes or indistinct borders. Their size and surrounding effects can indicate the aggressiveness of the tumor.
Factors Influencing Appearance
The appearance of spots on MRI scans can be influenced by several factors, including:
- The type of tissue affected: Different tissues respond differently to the MRI contrast agents, leading to variations in signal intensity.
- The presence of inflammation or fluid: Inflammation and fluid accumulation can alter the signal intensity, making the abnormality appear brighter or darker than expected.
- The stage of the disease: The appearance of a lesion might change over time as the condition progresses.
Comparing Characteristics of Lesions
Different types of lesions, while appearing as spots, exhibit distinct characteristics on MRI scans.
So, you’re seeing some spots on your MRI and wondering what they could be? It’s totally understandable to be concerned. While I’m not a medical professional, I can tell you that sometimes, certain supplements, like valerian root, what you need to know about valerian , can sometimes show up on scans. Ultimately, though, only a qualified doctor can accurately diagnose and explain what those spots mean in your case.
Don’t hesitate to schedule a follow-up appointment to get clarity on what’s going on.
- Cysts: Tend to be well-defined, rounded, and often contain fluid, appearing dark on T1-weighted images and bright on T2-weighted images.
- Tumors: Can have irregular shapes and borders. They can exhibit a wide range of signal intensities, depending on their composition. Their size and location are important diagnostic factors.
Potential Causes of Spots on MRI by Body Region
| Body Region | Potential Causes |
|---|---|
| Brain | Tumors, strokes, abscesses, cysts, demyelinating diseases |
| Spine | Herniated discs, tumors, infections, degenerative conditions |
| Liver | Cysts, hemangiomas, tumors, fatty liver disease |
| Kidneys | Cysts, tumors, infections |
Benign vs. Malignant Lesions on MRI
| Characteristic | Benign Lesions | Malignant Lesions |
|---|---|---|
| Shape | Often well-defined, rounded | Often irregular, poorly defined |
| Margins | Smooth, distinct | Often indistinct, blurred |
| Size | Can vary, but typically smaller | Can vary, but may grow larger over time |
| Enhancement | May or may not enhance with contrast | Often enhances with contrast |
Evaluating the Severity and Impact
Deciphering the significance of spots on an MRI goes beyond simply identifying their presence. Understanding the context of their size, shape, location, and relationship to surrounding tissue is crucial for accurate diagnosis and effective treatment planning. This section delves into the critical factors used to assess the severity and potential impact of these anomalies.Evaluating the severity of a condition revealed by MRI findings involves a meticulous examination of multiple factors.
The size, shape, and location of the lesions directly influence their potential impact on surrounding tissues and overall health. Understanding these aspects provides vital clues to the nature and progression of the underlying disease process.
Factors Influencing Diagnosis
The size, shape, and precise location of the spots are key indicators for a radiologist. A small, well-defined lesion in a non-critical area may have a significantly different prognosis than a large, poorly defined lesion near vital organs. For example, a small, circumscribed spot in the brain might indicate a benign condition, while a large, irregularly shaped spot in the same location could signal a more aggressive tumor.
Significance of Surrounding Tissue Changes
Surrounding tissue changes, such as edema (swelling), inflammation, or mass effect, provide additional insights into the severity and aggressiveness of the condition. Edema, often visible as a brighter area surrounding the lesion on the MRI, suggests inflammation and potential tissue damage. The degree of edema can indicate the level of inflammation and the extent of tissue involvement. The presence of mass effect, where the lesion pushes surrounding tissues, is also important, especially in the brain where space is limited.
Methods for Assessing Severity
Several methods are used to assess the severity of a condition based on MRI findings. Radiologists use standardized scales to quantify the extent of edema, the size of the lesion, and the degree of mass effect. Quantitative measurements from the MRI scan, such as lesion volume, provide objective data for comparing the severity of conditions across different patients and over time.
Furthermore, the radiologist’s interpretation of the image quality and the clarity of the lesion characteristics play a critical role in the assessment.
Disease Progression and Appearance
The appearance of spots on an MRI can vary depending on the stage of the disease process. In early stages, lesions may be small, well-defined, and have minimal surrounding edema. As the disease progresses, the lesions may enlarge, become less well-defined, and exhibit more pronounced surrounding edema. For example, in multiple sclerosis, lesions may appear as small, bright spots in the early stages, which can become larger and more numerous as the disease advances.
This evolution in appearance reflects the progression of the underlying pathological process.
Patient Symptoms and Context
The context of the patient’s symptoms is crucial in evaluating the severity of a condition. Symptoms such as pain, weakness, or neurological deficits provide crucial information about the impact of the lesion. A patient experiencing severe headaches and neurological symptoms alongside a large lesion in the brain will likely have a more serious prognosis than a patient with mild symptoms and a small, well-defined lesion.
Potential Impact on Organ Systems
| Type of Spot | Potential Impact on Organ Systems |
|---|---|
| Brain Tumor (Glioblastoma) | Potential for neurological deficits, seizures, headaches, cognitive impairment, and ultimately death if left untreated. |
| Spinal Cord Lesion | Potential for motor weakness, sensory loss, and bowel/bladder dysfunction, depending on the location and severity. |
| Liver Lesion (Metastasis) | Potential for liver dysfunction, pain, and potentially life-threatening complications depending on the size and spread of the tumor. |
| Lung Lesion (Inflammatory) | Potential for respiratory distress, pain, and potential for spreading the inflammation. |
The table above provides a general overview. Each case must be evaluated individually, taking into account the patient’s specific medical history, symptoms, and other imaging findings.
Interpreting the Findings in Relation to Symptoms
Deciphering the meaning behind those mysterious spots on an MRI requires a keen understanding of the patient’s symptoms. Simply put, the appearance of these spots isn’t enough to diagnose a condition; we need to correlate them with the patient’s individual experience. This involves careful consideration of the location, size, and characteristics of the spots, alongside the patient’s medical history and the presenting symptoms.
This is where the true diagnostic power of the MRI comes into play. It helps paint a more complete picture, guiding us towards a more accurate interpretation of the findings.Understanding the correlation between MRI findings and symptoms is crucial for accurate diagnosis and treatment planning. The location and characteristics of the spots can often provide valuable clues about the underlying pathology.
For example, a spot in the brain might correlate with neurological symptoms, while a spot in the lung might be associated with respiratory issues. This correlation is often complex, as different types of spots can cause similar symptoms, and the same spot can sometimes cause varied symptoms depending on its size and location. A comprehensive understanding of the patient’s medical history, including past illnesses and surgeries, is equally important.
This information can help us to understand if the symptoms are new or if they’re a recurrence of a previous condition.
Correlation Between Spot Appearance and Symptoms
The correlation between the appearance of spots on an MRI and a patient’s symptoms is multifaceted. A spot’s size, shape, and location, combined with the patient’s history, can provide vital clues. For instance, a small, well-defined spot in the brain might be associated with a minor neurological symptom, such as a subtle change in coordination. Conversely, a large, poorly defined spot in the same area might suggest a more significant neurological issue, possibly involving seizures or cognitive impairment.
So, I’ve got these weird spots showing up on my MRI, and I’m totally freaking out. It’s making me wonder about all sorts of things, like, could it be something serious? Or maybe it’s just something totally harmless, like a benign growth? Speaking of weird stuff, I’ve also been wondering if taking creatine might be playing a role in my hair loss lately.
Recent research suggests a possible connection, and I’m trying to get to the bottom of it. You can check out this article on does creatine cause hair loss to see what others are saying. Regardless, I’m still trying to figure out what these spots on my MRI could be. It’s definitely a lot to process.
Impact of Medical History on Interpretation, What are these spots on my mri
A patient’s medical history plays a critical role in interpreting MRI findings. Consider a patient with a known history of multiple sclerosis. If they present with new neurological symptoms and an MRI shows spots in the brain, the correlation becomes more apparent and may strongly suggest a worsening of their pre-existing condition. This is in contrast to a patient with no prior neurological issues.
Similarly, a patient with a history of cancer might exhibit different symptoms associated with a spot compared to a patient with no such history.
Comparing Symptoms of Benign and Malignant Lesions
Benign and malignant lesions, while both potentially causing spots on an MRI, can manifest with different symptom profiles. Benign lesions, often slow-growing and non-cancerous, might present with subtle symptoms that develop gradually over time. Malignant lesions, on the other hand, might present with more rapid symptom onset, often accompanied by pain, swelling, or other concerning signs.
Location and Characteristics Affecting Symptoms
The location and characteristics of the spots can greatly influence the symptoms experienced by the patient. For example, a spot in the spinal cord might lead to pain, weakness, or numbness in the limbs, while a spot in the liver might lead to abdominal discomfort or jaundice.
Symptoms Associated with Spots in Different Body Regions
| Body Region | Potential Symptoms |
|---|---|
| Brain | Headache, seizures, dizziness, vision changes, memory problems, speech difficulties |
| Spinal Cord | Pain, numbness, tingling, weakness, loss of coordination, bowel or bladder dysfunction |
| Lungs | Cough, shortness of breath, chest pain, fever, fatigue |
| Liver | Abdominal pain, jaundice, fatigue, nausea, vomiting |
| Kidneys | Pain in the back or side, blood in the urine, swelling, high blood pressure |
Potential Symptoms of Different Types of Lesions
Different types of lesions, visible as spots on MRI scans, can produce a wide array of symptoms. A cyst, for instance, might cause pressure symptoms if it grows large enough, whereas a tumor might cause pain and swelling depending on its size and location. Inflammatory lesions can manifest with pain and inflammation, often accompanied by fever or other systemic symptoms.
So, you’ve got these spots showing up on your MRI, and you’re understandably worried. While I’m not a medical professional, it’s crucial to remember that unusual spots on an MRI can sometimes be related to underlying conditions. For instance, have you been experiencing any wheezing lately? If so, consulting a doctor about possible wheezing causes and their evaluation and treatment is essential.
Wheezing causes evaluation and treatment can vary depending on the root cause, so it’s important to get a proper diagnosis. Ultimately, getting those spots on your MRI properly diagnosed is key.
Preparing for Further Investigations
Armed with the MRI findings, the next crucial step is to determine if additional diagnostic procedures are necessary. This involves carefully evaluating the anomalies revealed in the images and considering the patient’s overall health and symptoms. A thorough assessment is essential to ensure the most appropriate and effective course of action is taken.
Need for Further Diagnostic Procedures
The decision to pursue further investigations is not always straightforward. It hinges on the characteristics and severity of the detected anomalies, as well as the patient’s clinical presentation. While some MRI findings might suggest a benign condition, others necessitate further investigation to confirm the diagnosis and rule out more serious possibilities.
Options for Additional Testing
Several diagnostic tools can supplement the MRI findings. These options may include biopsies, which involve taking small tissue samples for microscopic examination, and specialist consultations, such as with a neurologist or a radiologist specializing in musculoskeletal imaging.
- Biopsies: In cases where the MRI suggests a suspicious lesion, a biopsy might be necessary to definitively determine the nature of the abnormality. For example, if the MRI reveals a mass in the breast, a biopsy could help distinguish between benign and malignant tissue.
- Specialist Consultations: Depending on the location and type of anomaly, a consultation with a specialist is often crucial. If the MRI reveals potential neurological issues, a neurologist could provide valuable insights and guidance. Similarly, a musculoskeletal radiologist may be consulted if the findings suggest a problem with the bones or joints.
Referring the Patient to Specialists
Referring a patient to a specialist involves a structured process. The referring physician, often the primary care physician, plays a key role in evaluating the MRI results and determining the appropriate specialist. This referral process ensures that the patient receives the most relevant expertise for their specific condition.
A key consideration is the specialist’s expertise. If the MRI suggests a potential cardiovascular issue, a cardiologist would be the appropriate specialist, not a dermatologist.
MRI Findings Guiding Further Procedures
MRI findings often provide crucial clues for guiding further investigations. For instance, if the MRI shows a well-defined, encapsulated lesion in the liver, a biopsy might be considered to determine its nature. Conversely, if the MRI reveals a diffuse pattern of abnormality in the lungs, further imaging studies like a CT scan might be necessary to delineate the extent of the involvement.
Table of Diagnostic Procedures and Indications
| Diagnostic Procedure | Indication (Based on MRI Findings) |
|---|---|
| Biopsy | Suspicious lesions, unclear nature of abnormalities, potential malignancy. |
| CT Scan | Diffuse or extensive abnormalities, need for detailed anatomical evaluation, assessment of tissue density. |
| PET Scan | Suspicion of metabolic abnormalities, evaluation of tumor activity or spread. |
| Angiography | Suspected vascular abnormalities, evaluation of blood flow patterns, identification of blockages. |
| Specialist Consultation (e.g., Neurologist) | Anomalies in the brain or spinal cord, suspected neurological conditions. |
Summary
In conclusion, understanding “what are these spots on my MRI” requires a multifaceted approach, considering the scan’s purpose, the potential anomalies, and the overall context of your medical history and symptoms. While this exploration provides valuable insights, it’s crucial to remember that this information is not a substitute for professional medical advice. Always consult with your doctor to discuss your specific MRI findings and any associated concerns.
Further investigations, such as biopsies or specialist consultations, may be necessary, and your doctor will guide you through these procedures based on the findings and your individual situation.