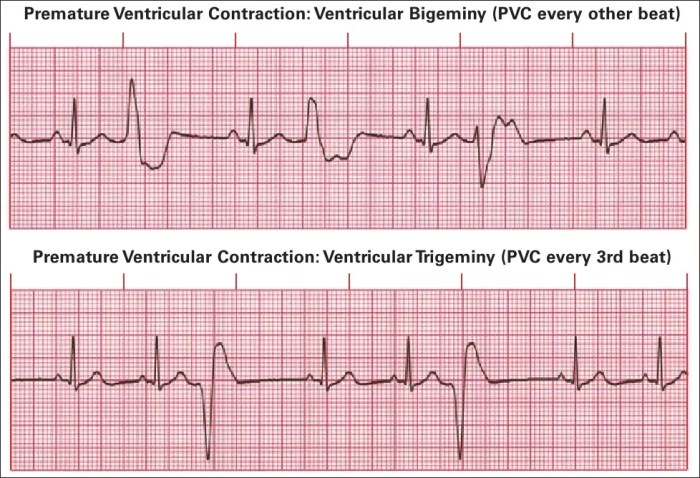
Premature ventricular complexes pvcs – Premature ventricular complexes (PVCs) are a common cardiac rhythm disturbance. This in-depth look explores PVCs, from their definition and characteristics to potential causes, symptoms, diagnosis, management, and complications. We’ll delve into the electrical mechanisms behind PVCs, the role of various factors, and the importance of patient education. PVCs, often benign,…
Category: Health & Wellness
Alcohol & Arthritis Drugs Is It Forbidden?
Is alcohol forbidden when taking arthritis drugs? This crucial question impacts many people living with arthritis, demanding careful consideration of potential interactions. Different arthritis medications interact with alcohol in various ways, and understanding these interactions is vital for safe and effective treatment. This post will delve into the potential risks and benefits, providing valuable insights…
Tirzepatide Zepbound Lowers Blood Pressure
Tirzepatide Zepbound reduces blood pressure, a promising development in managing hypertension. This innovative medication, a dual GIP and GLP-1 receptor agonist, offers a novel approach to blood pressure regulation, potentially impacting not just blood pressure but also metabolic health and weight management. Early clinical trials are exploring its efficacy and safety profile, comparing it to…
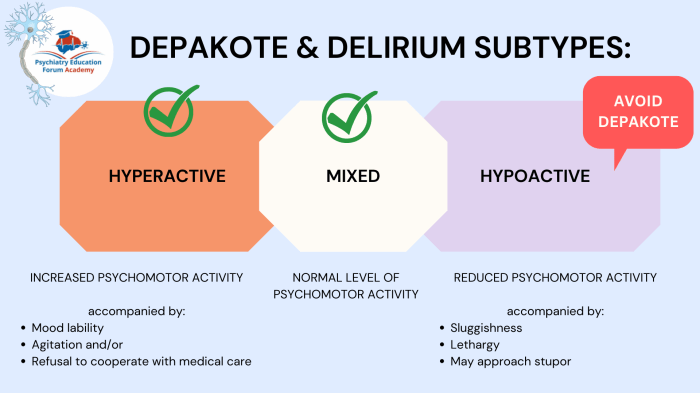
Whats the Difference Between Delirium and Dementia?
Whats the difference between delirium and dementia? These two conditions, though both affecting cognitive function, have vastly different characteristics, onsets, and courses. Understanding these distinctions is crucial for accurate diagnosis and effective treatment. Delirium typically emerges suddenly, often triggered by an underlying medical issue, and involves fluctuating attention and awareness. Dementia, on the other hand,…
How to Use Crutches A Comprehensive Guide
How to use crutches sets the stage for this in-depth guide, covering everything from understanding different crutch types to mastering safe techniques for various terrains and activities. This guide will equip you with the knowledge and confidence to navigate daily life while using crutches safely and effectively. Whether you’re a recent user or looking to…
Should I Take Vitamins During Cancer Treatment?
Should I take vitamins during cancer treatment? This crucial question weighs heavily on many facing cancer and their families. The nutritional needs of cancer patients are complex, often significantly altered by the disease and its treatments. This exploration delves into the intricate relationship between vitamins, cancer treatment, and overall well-being, offering a comprehensive overview of…
Massage Therapy Helps Relieve Pain A Deep Dive
Massage therapy helps relieve pain, offering a holistic approach to managing discomfort. This exploration delves into various massage techniques, their physiological effects, and the types of pain they can address. We’ll examine specific muscle groups and areas often targeted for relief, along with a comparative analysis of different massage styles. Beyond the basics, we’ll investigate…
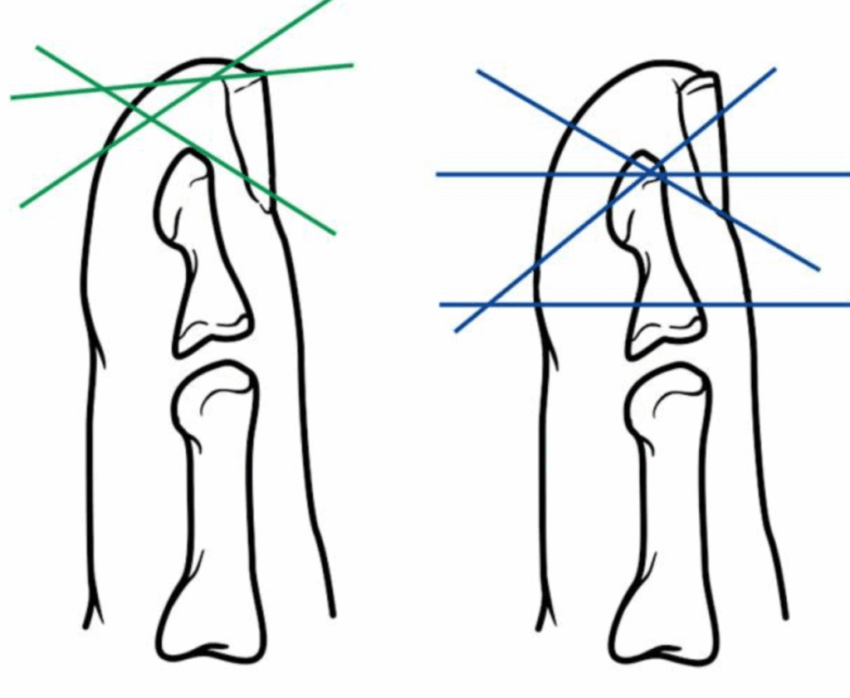
Fingertip Injury Will Tip Grow Back?
Fingertip injury will tip grow back? This in-depth exploration delves into the fascinating world of fingertip injuries, examining the intricate anatomy, diverse injury types, and the complex healing process. We’ll uncover the factors that influence regeneration, explore treatment options, and analyze the prognosis for full recovery. From the microscopic level of tissue repair to the…
Is Tramadol a Controlled Substance? Understanding the Details
Is tramadol a controlled substance? This question delves into the complexities of tramadol’s classification, legal status, and potential for misuse. We’ll explore its chemical composition, effects on the body, and legal regulations across various jurisdictions. Understanding the risks and benefits associated with this medication is crucial for both patients and healthcare professionals. Tramadol, a synthetic…
Perils of Using the Internet to Self-Diagnose
Perils of using the internet to self diagnose: Navigating the vast ocean of online health information can be tempting, but it’s crucial to understand the potential pitfalls. From misinterpreting symptoms to delaying professional care, the consequences of self-diagnosing online can be far-reaching and potentially harmful. This exploration delves into the risks associated with seeking medical…