Do I need a knee brace? This comprehensive guide delves into the complexities of knee pain and when a brace might be the right solution. We’ll explore various types of knee pain, potential causes, and the importance of consulting a healthcare professional. Beyond simply answering the question, we’ll equip you with the knowledge to make informed decisions about your knee health.
Understanding your knee pain, whether acute or chronic, is the first step in determining if a brace is necessary. This guide will walk you through evaluating the severity of your injury and the different types of braces available. We’ll discuss how to consider your activity level and overall physical condition when choosing a brace. Furthermore, we’ll explore alternative treatments for knee pain, offering a broader perspective on managing your discomfort.
Understanding Knee Pain: Do I Need A Knee Brace
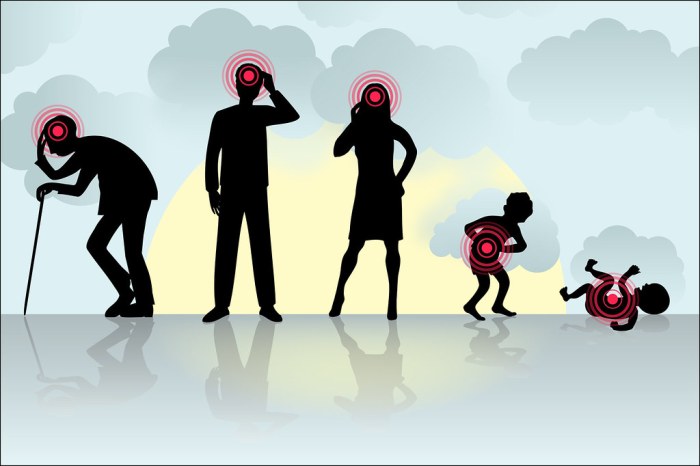
Knee pain is a common ailment affecting individuals of all ages and activity levels. It can range from mild discomfort to severe, debilitating agony, significantly impacting daily life. Understanding the various types of knee pain, their potential causes, and symptoms is crucial for effective management and prompt medical intervention. This understanding empowers individuals to make informed decisions about their health and seek appropriate care.
Types of Knee Pain
Knee pain can manifest in diverse ways, varying in intensity and duration. Differentiating between acute and chronic pain is essential for proper diagnosis and treatment. Acute knee pain typically arises suddenly, often due to an injury, while chronic pain persists for extended periods, potentially stemming from underlying conditions. Recognizing the nuances of these pain types aids in identifying the appropriate course of action.
Common Knee Pain Conditions
The following table Artikels various types of knee pain, their potential symptoms, probable causes, and suggested next steps. It’s crucial to remember that this table serves as a general guide. Accurate diagnosis and treatment always require professional medical evaluation.
| Pain Type | Symptoms | Potential Causes | Recommended Next Steps |
|---|---|---|---|
| Patellofemoral Pain Syndrome (Runner’s Knee) | Pain around the kneecap, often worsened by activities like running, squatting, or going up and down stairs; clicking or grinding sensation; stiffness; swelling. | Repetitive stress, muscle imbalances, improper footwear, overuse, poor posture. | Rest, ice, physical therapy, strengthening exercises, and potentially orthotics. |
| Meniscus Tear | Sharp, localized pain in the knee joint, especially during twisting or pivoting movements; swelling; stiffness; catching or locking sensation; limited range of motion. | Sudden twisting injury, wear and tear, degeneration. | Consult an orthopedist for diagnosis, which may involve imaging tests (MRI); possible surgical intervention depending on the severity. |
| Ligament Injury (e.g., ACL Tear) | Severe pain and swelling immediately following a sudden impact or twisting injury; instability in the knee; difficulty bearing weight. | Trauma, sudden impact, sports-related activities. | Immediate medical attention; evaluation by an orthopedist; potential need for surgery. |
| Osteoarthritis | Pain that gradually worsens over time, particularly with weight-bearing activities; stiffness, especially in the morning; creaking or grinding sensation; swelling; reduced range of motion. | Age-related wear and tear, joint degeneration, genetic predisposition, obesity. | Consult a rheumatologist for diagnosis; potential use of pain relievers, physical therapy, and assistive devices. |
| Bursitis | Pain and tenderness around the bursae (fluid-filled sacs) in the knee; swelling; increased pain with pressure. | Repetitive stress, direct impact, infection. | Rest, ice, compression, elevation; over-the-counter pain relievers; if severe or recurrent, consult a doctor. |
Importance of Professional Consultation
A comprehensive physical examination is crucial for accurately diagnosing knee pain. The examination often involves assessing the range of motion, stability, and palpation of the knee joint. A healthcare professional can evaluate the specific symptoms, medical history, and any potential underlying conditions. This careful assessment ensures appropriate and effective treatment.
Identifying Potential Need for a Brace

Knee pain can be a frustrating experience, impacting daily activities and quality of life. Knowing when a knee brace might be helpful can significantly improve recovery and prevent further complications. This section will explore the various situations where a knee brace proves beneficial, considering injury severity and the different types of braces available.Understanding the potential need for a knee brace involves considering the specifics of your knee pain, including the type and severity of any injury, and the overall stability of your knee joint.
A brace is not always the answer, but in some cases, it can be a valuable tool for support and recovery.
Situations Where a Brace Might Be Beneficial
A knee brace can provide crucial support in a range of situations, from mild discomfort to significant injury. Its effectiveness hinges on the specific circumstances. For example, a mild sprain might benefit from a simple brace, while a severe ligament tear may require a more complex and supportive model.
Injury Severity and Brace Necessity
The severity of the injury plays a critical role in determining the need for a brace. A minor strain or overuse syndrome may not require a brace, while a ligament tear or meniscus injury often necessitates support. The extent of the injury and the individual’s activity level influence the choice. For example, a moderate sprain in an athlete might require a brace for continued participation and injury prevention, while a similar injury in a less active individual might not necessitate a brace.
Types of Knee Braces and Their Applications
Numerous types of knee braces cater to different needs. Hinged braces provide significant stability and are often used for injuries like ligament tears or instability. Wraparound braces offer a more gentle level of support, useful for mild strains or general knee discomfort. Patellar braces, focused on the kneecap, are beneficial for patellofemoral pain syndrome. The selection depends on the specific issue.
Conditions Where a Brace Might Offer Support or Stability
A knee brace can be beneficial in various conditions. For example, individuals with osteoarthritis may find a brace helpful in managing pain and improving joint stability. Individuals recovering from ACL tears may use a hinged brace for support and rehabilitation. Furthermore, people with patellofemoral pain syndrome might use a patellar brace to stabilize the kneecap. The appropriateness of a brace depends on the specific condition and the individual’s needs.
- Ligament Tears: A torn ligament in the knee often requires a brace for support and stability during healing and rehabilitation. A hinged brace is typically used to control movement and prevent further damage.
- Meniscus Tears: Similar to ligament tears, a meniscus tear can benefit from a brace to limit stress on the damaged cartilage and promote healing.
- Patellofemoral Pain Syndrome: A patellar brace can help to stabilize the kneecap, reducing pain and discomfort associated with this condition.
- Osteoarthritis: A brace can provide support and stability for individuals with osteoarthritis, managing pain and discomfort while improving mobility.
Comparison of Different Knee Brace Types
The following table Artikels the features, advantages, and disadvantages of various knee brace types:
| Brace Type | Features | Advantages | Disadvantages |
|---|---|---|---|
| Hinged Brace | Provides significant stability and support; often adjustable for specific needs. | Excellent support for ligament tears, ACL reconstructions, and instability issues. | Can be bulky and restrict movement in some cases. |
| Wraparound Brace | Provides moderate support and compression; often lighter and more flexible. | Good for mild strains, general knee pain, and patellofemoral pain syndrome. | Less supportive than hinged braces; may not be suitable for severe injuries. |
| Patellar Brace | Focuses on stabilizing the kneecap. | Excellent for patellofemoral pain syndrome, tracking issues, and kneecap pain. | Limited support for other knee issues; may not be sufficient for severe ligament damage. |
Factors to Consider Before Using a Brace
Choosing the right knee brace is crucial for effective pain management and injury prevention. It’s not a one-size-fits-all solution, and careful consideration of several factors is essential to ensure optimal support and avoid potential complications. Understanding the nuances of fit, activity level, and individual physical condition is paramount for successful brace use.Proper brace selection involves a deeper understanding than simply addressing the immediate discomfort.
The brace’s function goes beyond mere aesthetics; it plays a significant role in the recovery process. It acts as a support system, mitigating stress on the injured area and preventing further damage.
Proper Fitting and Support
The efficacy of a knee brace hinges heavily on its proper fit. A poorly fitted brace can be uncomfortable, ineffective, and even potentially harmful. A snug fit that avoids slippage or pressure points is essential. Overly loose braces offer inadequate support, while overly tight braces can impede circulation and cause discomfort. A professional, such as a physical therapist or doctor, can provide guidance on appropriate sizing and application techniques.
They can ensure the brace’s fit conforms to the unique contours of your knee, offering maximum support without compromising comfort.
Influence of Activities on Brace Choice, Do i need a knee brace
The type of activity significantly impacts the ideal brace selection. A brace designed for low-impact activities like walking or light exercise will differ from one intended for high-impact sports like basketball or soccer. For instance, a brace designed for running might feature a reinforced patellar area to prevent kneecap tracking issues, while a brace for contact sports might emphasize stability and protection from lateral forces.
Consider the specific demands of your activity when choosing a brace.
Figuring out if you need a knee brace can be tricky, right? Sometimes, pain signals other underlying issues. For example, persistent knee pain might be connected to broader health concerns, like erectile dysfunction. Understanding the signs and symptoms of erectile dysfunction is important, and checking out resources like erectile dysfunction signs symptoms and complications can help.
Ultimately, if your knee pain persists or worsens, consulting a doctor is key to determine the root cause and whether a brace is truly necessary.
Impact of User’s Physical Condition on Brace Suitability
Individual physical conditions significantly affect brace suitability. Pre-existing medical conditions, such as arthritis or ligament injuries, may necessitate a specific type of brace to address the unique needs of the condition. Additionally, muscle strength and flexibility play a role in how well a brace functions. A brace might be less effective for someone with weak surrounding muscles, as the brace cannot compensate entirely for a lack of support from the body.
Consulting a healthcare professional for personalized recommendations based on your specific physical condition is crucial.
Wondering if you need a knee brace? It really depends on the specifics of your knee pain. While factors like injury history and activity level are important, your diet might also play a role. Understanding the glycemic index vs load can help you make smarter food choices, which in turn can influence inflammation and potentially reduce knee pain.
For a deeper dive into the science behind the glycemic index vs load, check out this helpful resource: glycemic index vs load. Ultimately, if your knee pain persists, consulting a doctor is crucial to determine the best course of action for your specific situation.
Potential Risks Associated with Improper Brace Use
Improper brace use can lead to a range of complications. These include skin irritation, discomfort, and decreased circulation, depending on the tightness or material. In certain cases, the brace might not provide the necessary support, potentially exacerbating the underlying injury. Improper fitting can lead to instability and discomfort, making it challenging to participate in activities. The potential for further damage is another significant risk associated with inappropriate brace use.
Always follow the manufacturer’s instructions carefully, and consult with a healthcare professional to ensure proper use.
Activity, Condition, Brace Type, and Potential Risks
| Activity | User Condition | Brace Type | Potential Risks |
|---|---|---|---|
| Running | Patellar tendinopathy | Hinged Knee Brace | Skin irritation, decreased circulation if too tight, inadequate support if not properly fitted |
| Basketball | Ligament sprain | Wraparound Knee Brace | Brace slippage, reduced support if not the correct size, potential for further injury if not fitted properly |
| Gardening | Osteoarthritis | Knee Sleeve | Reduced support, potential for discomfort if not providing adequate compression |
| Hiking | Knee instability | Knee Stabilizer Brace | Skin irritation from friction, insufficient support if not appropriate to the instability, discomfort if too tight |
Types of Knee Braces and Their Functions
Knee braces come in a wide variety of designs, each tailored to address specific knee pain concerns and support needs. Understanding the different types available allows individuals to make informed decisions about the best brace for their particular situation. From simple compression wraps to intricate hinged supports, each brace offers varying degrees of stability, support, and compression.Different knee brace designs cater to various levels of support and activity.
The choice of brace depends on the specific needs of the individual, considering factors like the type and severity of knee pain, desired level of stability, and the anticipated level of activity. Understanding these distinctions is crucial for selecting the most effective brace to manage knee discomfort and maintain optimal function.
Hinged Knee Braces
Hinged knee braces provide a high degree of support and stability, particularly for individuals with moderate to severe knee instability or those recovering from injuries. These braces feature hinges that allow controlled flexion and extension of the knee joint, while also limiting excessive movement. The hinges typically incorporate adjustable straps and buckles to customize the fit and support.
They are often made of durable materials such as neoprene or plastic.The advantages of hinged braces include enhanced stability and protection for the knee joint, especially during activities that require greater stability. They are commonly used for ACL or MCL injuries, arthritis, and post-operative recovery. However, the restricted range of motion might be a limitation for individuals who need a more flexible brace for certain activities.
Considering if you need a knee brace? It really depends on the situation, and sometimes anxieties can play a role. For example, if you have a fear of contamination, or a phobia of germs like mysophobia, phobia of germs mysophobia might affect your decision about using a brace. Ultimately, a doctor’s assessment is crucial to determine if a brace is the right solution for your specific knee issue.
Wrap-Around Knee Braces
Wrap-around knee braces, often made of a stretchy material like neoprene or elastic fabric, provide compression and support to the knee. They are generally lightweight and comfortable, and can be worn under clothing. These braces are often preferred for mild knee pain, such as patellofemoral pain syndrome or mild instability, as they offer a good balance between support and flexibility.
The wrap-around design typically utilizes straps or Velcro closures for a secure fit.Wrap-around braces are highly versatile, suitable for a wide range of activities. Their advantages lie in their flexibility and ease of use, allowing for a comfortable fit beneath clothing. However, the limited support compared to hinged braces might not be sufficient for severe knee conditions or high-impact activities.
Other Types of Knee Braces
Beyond hinged and wrap-around designs, other specialized knee braces cater to specific needs. These braces often incorporate unique features, such as patellar stabilizers, lateral support, or specific compression zones, to address particular knee conditions or activities. Custom-molded braces provide a highly personalized fit, offering tailored support for complex knee issues.These specialized braces are designed for specific knee conditions.
For example, a patellar tracking brace is designed to stabilize the kneecap, while a brace with lateral support might address lateral instability. The specific features and benefits of each type are tailored to address the individual needs of the user.
Comparison of Knee Brace Types
| Brace Type | Material | Support Level | Stability | Activities Suitable For | Target Conditions |
|---|---|---|---|---|---|
| Hinged | Neoprene, Plastic | High | High | High-impact sports, post-surgery | ACL/MCL injuries, arthritis, post-operative recovery |
| Wrap-around | Neoprene, Elastic | Moderate | Moderate | Everyday activities, light exercise | Patellofemoral pain, mild instability |
| Other (e.g., Patellar Stabilizer) | Various | Variable | Variable | Specific activities, conditions | Specific knee conditions (e.g., patellar tracking issues) |
This table provides a concise overview of the key characteristics of different knee brace types. Choosing the right brace depends on the specific needs of the individual, considering factors like the type and severity of the condition, and desired level of support.
When to Seek Professional Advice
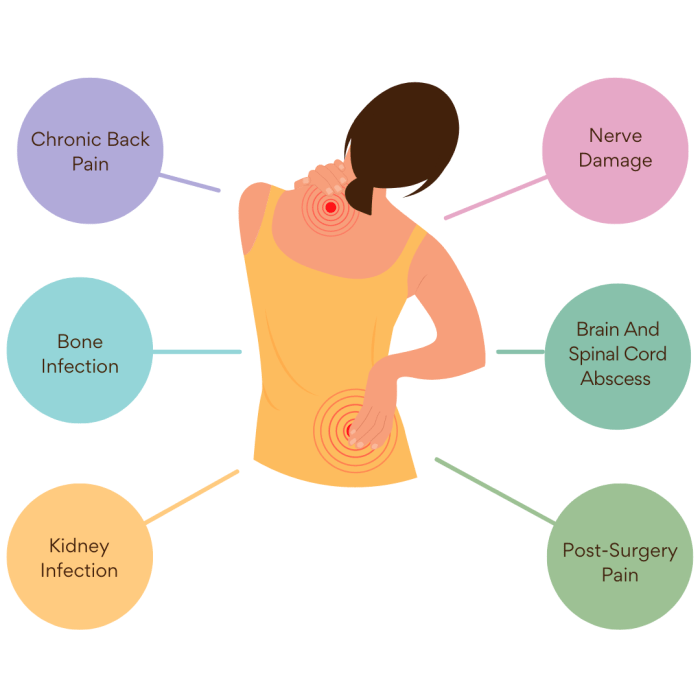
Knowing when to seek professional advice for knee pain is crucial for proper diagnosis and treatment. Ignoring persistent or worsening symptoms can lead to further complications and hinder your recovery. This section Artikels key situations where a doctor or physical therapist’s expertise is essential for managing knee pain and selecting the right brace.
Crucial Situations Requiring Professional Advice
Seeking medical advice is paramount when knee pain is accompanied by other concerning symptoms. This includes persistent pain, swelling, or stiffness that doesn’t improve with home remedies. Red flags, like difficulty bearing weight or a popping or clicking sound in the knee, demand immediate attention.
When Brace Use Needs Supervision
Proper brace use and selection are essential for optimal knee support and recovery. A healthcare professional can assess your specific needs and recommend the most suitable brace type and fit. This personalized approach ensures the brace effectively supports your knee without causing further harm or hindering your healing process. A doctor or physical therapist can also monitor your progress and adjust the brace as needed.
They can guide you on appropriate exercises and activities that don’t compromise your recovery.
Importance of Addressing Persistent or Worsening Pain
Persistent or worsening knee pain, even with a brace, warrants a visit to a medical professional. This is particularly true if the pain is accompanied by other symptoms like fever, redness, or warmth around the knee joint. These symptoms could indicate a more serious underlying condition. Ignoring such symptoms could delay diagnosis and treatment, potentially leading to long-term problems.
Personalized Approach to Brace Selection
A doctor or physical therapist can evaluate your specific knee condition and activity level to determine the ideal brace. This personalized approach ensures the brace provides the right support without hindering mobility or causing discomfort. Factors like the type of injury, the extent of damage, and your physical capabilities will all be considered. A brace that’s appropriate for one person might not be suitable for another.
Red Flags Signaling Immediate Medical Consultation
Certain symptoms signal the need for immediate medical attention. These “red flags” necessitate a prompt visit to the doctor, even if you’re already using a knee brace. A few examples include:
- Severe pain that’s sudden and intense.
- Inability to bear weight on the affected leg.
- Severe swelling or bruising around the knee.
- Deformity or instability in the knee joint.
- A popping, clicking, or grinding sound in the knee.
- Fever or chills accompanying knee pain.
- Numbness or tingling in the leg below the knee.
- Significant pain that worsens at night.
These signs could indicate a serious injury or medical condition that requires immediate diagnosis and treatment. Do not delay seeking professional help if you experience any of these red flags. Prompt medical attention can prevent further complications and improve your chances of a full recovery.
Proper Use and Care of Knee Braces
Knee braces can be a valuable tool for supporting and protecting your knee, but only when used correctly. Proper application, maintenance, and care are crucial to maximizing their effectiveness and minimizing the risk of complications. Understanding these factors ensures that you get the most out of your brace and support your recovery.
Applying the Brace Correctly
Proper application is fundamental to a brace’s effectiveness. Incorrect placement can compromise support and potentially lead to discomfort or injury. A well-fitted brace provides targeted support, reducing stress on the affected tissues.
- Inspect the Brace: Before applying, carefully examine the brace for any damage, loose parts, or signs of wear. This initial check ensures the brace is in good working order and safe to use.
- Prepare the Skin: Clean and dry the area around your knee where the brace will be placed. Remove any lotions or creams that might interfere with the brace’s adherence. This preparation helps ensure proper contact and prevents skin irritation.
- Positioning: Position the brace according to the manufacturer’s instructions. Ensure the brace aligns correctly with the knee joint. A properly aligned brace provides the most support and prevents undue pressure.
- Secure the Straps: Tighten the straps, making sure they are snug but not excessively tight. Excessive tightness can restrict blood flow, while insufficient tightness compromises the brace’s support. Use a moderate and even tension. The goal is to find the sweet spot between support and comfort.
- Check for Comfort: After applying the brace, take a moment to ensure it’s comfortable. Any pressure points or areas of discomfort should be adjusted before continued use. Pay close attention to the comfort level.
Maintaining Brace Effectiveness and Hygiene
Regular maintenance ensures a brace’s effectiveness and prevents the build-up of bacteria, promoting hygiene.
- Regular Cleaning: Clean the brace regularly, following the manufacturer’s instructions. Some braces may require daily cleaning, while others may need cleaning only every few days. The specific frequency is indicated by the manufacturer. Cleaning helps to maintain the brace’s functionality and prevent the build-up of dirt, sweat, and bacteria.
- Drying the Brace: Always dry the brace thoroughly after cleaning. Moisture can promote bacterial growth, potentially causing skin irritation. Air drying is often the best method.
- Storage: Store the brace in a clean, dry place away from direct sunlight. Storing the brace in a cool, dry place helps maintain its integrity and longevity. Avoid extreme temperatures or damp environments.
Adjusting and Removing the Brace
Knowing how to adjust and remove the brace safely and effectively is crucial for proper use.
- Adjusting Straps: Adjust the straps as needed throughout the day, ensuring the brace remains snug and supportive. Regular adjustments maintain optimal support.
- Removing the Brace: Carefully unfasten the straps, ensuring the brace is not pulled or yanked. This method prevents potential injury and maintains the brace’s structural integrity.
Following Manufacturer’s Instructions
Adherence to manufacturer’s instructions is essential for safe and effective brace use.
“Always refer to the manufacturer’s instructions for specific details on cleaning, application, and adjustments.”
Following the manufacturer’s instructions guarantees optimal brace performance and minimizes the risk of complications.
Alternative Treatments for Knee Pain
Knee pain can be a debilitating condition, impacting daily activities and overall well-being. While medical interventions and bracing are often necessary, alternative therapies can play a significant role in pain management and recovery. These methods, often combined with traditional care, can offer a holistic approach to alleviating knee discomfort and improving function.Alternative treatments for knee pain encompass a wide range of approaches, from physical therapy and exercise to lifestyle modifications and various forms of complementary therapies.
These methods can help address the underlying causes of pain, improve joint function, and promote overall healing and recovery.
Physical Therapy and Exercise
Physical therapy plays a crucial role in managing knee pain by strengthening the muscles surrounding the joint. Exercises specifically designed to improve flexibility, stability, and range of motion can effectively reduce pain and improve function. A qualified physical therapist can develop a personalized exercise program tailored to the individual’s specific needs and limitations. This personalized approach is key to successful outcomes.
Regular exercise, even simple activities like walking, can contribute significantly to knee health and pain relief.
Lifestyle Modifications
Maintaining a healthy weight is vital for reducing stress on the knees. Excessive weight can significantly exacerbate existing knee pain or contribute to new problems. Dietary changes that focus on nutrient-rich foods and adequate hydration also support overall health and can contribute to pain relief. Avoiding activities that put excessive stress on the knees, such as prolonged periods of standing or high-impact exercises, is also important.
Warm-up and Cool-down Routines
Proper warm-up and cool-down routines are essential components of any exercise program. A warm-up prepares the muscles and tissues for activity, reducing the risk of injury and improving performance. A cool-down allows the body to gradually return to its resting state, reducing muscle soreness and stiffness. A simple 5-10 minute warm-up, such as light cardio and dynamic stretching, can significantly reduce the risk of injury during exercise.
Similarly, a cool-down involving static stretches can help prevent muscle stiffness and promote recovery.
Ice and Heat Therapy
Ice and heat therapy are frequently used to manage knee pain. Ice therapy is often used in the acute phase of injury or inflammation to reduce swelling and pain. Heat therapy, on the other hand, is often used to improve blood flow and reduce muscle stiffness and pain. The choice between ice and heat depends on the specific cause and stage of the knee pain.
For example, ice may be preferable immediately following an injury, while heat may be more beneficial for chronic pain.
Potential Alternative Treatments
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body. It’s believed to stimulate the flow of energy and reduce pain.
- Massage Therapy: Manual manipulation of soft tissues can improve circulation, reduce muscle tension, and alleviate pain.
- Chiropractic Care: A chiropractor focuses on the musculoskeletal system, identifying and correcting any misalignments or restrictions that may contribute to knee pain.
- Yoga and Tai Chi: These gentle practices can improve flexibility, strength, and balance, potentially reducing knee pain and improving overall well-being.
- Herbal Remedies: Some herbal remedies are believed to possess anti-inflammatory properties and may help reduce knee pain. However, it’s crucial to consult with a healthcare professional before using any herbal remedies.
Final Conclusion
Ultimately, deciding whether or not you need a knee brace is a personal choice, informed by your specific situation and medical advice. This guide aims to empower you with the knowledge to make an educated decision. Remember, a knee brace is not a substitute for professional medical care. If your knee pain persists or worsens, seek immediate medical attention.
Proper use and care of a brace, when appropriate, can aid recovery and prevent further complications.